Chapter 107 Spondylectomy for Spinal Tumors
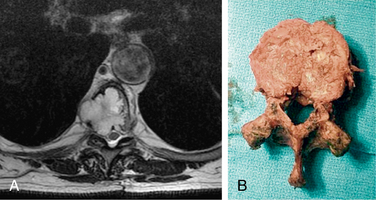
Spondylectomy is defined as removal of an entire segment of the spine, including the vertebral body, pedicles, superior and inferior articulating processes, pars, transverse processes, lamina, and spinous process. Removal of the entire spinal segment en bloc is possible only with sacrifice of the spinal cord or the cauda equina, as the spinal cord and cauda equina lie within the spinal canal, incarcerated by the spine. Tumors within the spine can be removed either in a piecemeal fashion (intralesional) or en bloc (in one piece, without violation of the tumor margin). To achieve an en bloc resection of a tumor, the technique of a total spondylectomy can be employed (Fig. 107-1). As a point of semantics, the tumor is removed en bloc, but the spondylectomy is usually not an en bloc spondylectomy.1
General Concepts and Surgical Planning
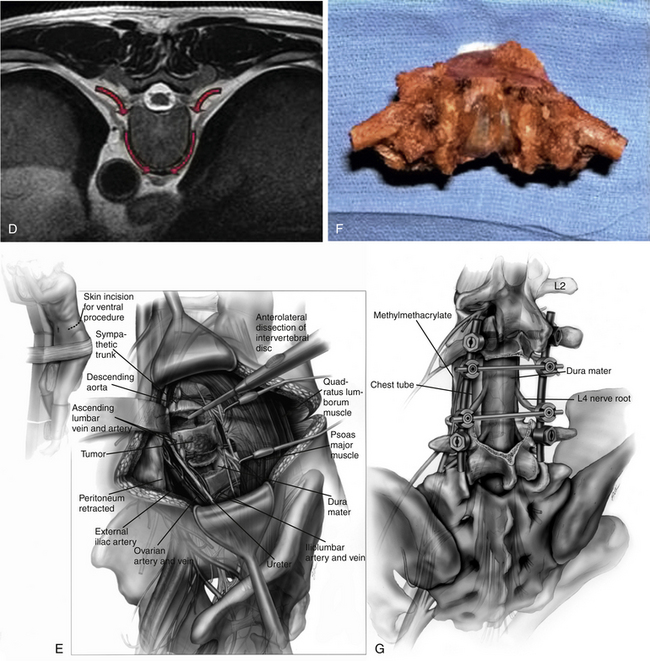
The anatomic location of the tumor to be removed within a particular vertebral segment or segments will dictate the steps in achieving an en bloc resection via a spondylectomy.1 For simplicity, the planning can be divided into two stages: a preparatory stage and a stage in which the tumor is delivered. Accomplishment of the first stage, the preparatory stage, may require multiple procedures.
The vascular structures involved in the resection vary at different levels of the spine. In the cervical spine, a vertebral artery might need to be sacrificed to achieve a resection, and doing so might result in posterior fossa ischemia and stroke. In the thoracic spine, multiple segmental vessels might need to be ligated, increasing the risk of ischemia to the spinal cord. In the lumbar spine, the iliac arteries and veins might need to be manipulated or even bypassed, potentially causing ischemia to the bowel, kidneys, or lower extremities. Manipulation or sacrifice of the inferior vena cava and iliac vessels increases the chance for thrombus formation and consequent pulmonary embolus.
Neurologic sacrifice can be entertained only if the deficit that will be produced is tolerable to the patient’s expectations and lifestyle acceptance. Sacrifice of a certain root alone might not produce a significant deficit, but combinations of roots sacrificed can be crippling (Table 107-1). C1-4 can usually be sacrificed without significant morbidity. Sacrifice of C3 and C4 together could result in diaphragm weakness. Cutting C5, C6, C8, or T1 usually results in profound weakness. Sacrifice in the thoracic spine (T2-12) will result in a bandlike distribution of numbness but usually has inconsequential motor loss. Sacrifice of L1 or L2 in isolation will produce weakness, but over time, patients usually are able to compensate for the loss quite well. L3 loss will result in quadriceps weakness and may require bracing of the knee to walk. L4 sacrifice can also result in quadriceps weakness, but the problem that is usually noted is proprioceptive difficulty of the knee joint. Without proper proprioception of the knee, a patient may find the knee week and can complain of the knee buckling at times during ambulation. L5 loss results in footdrop. S1 sacrifice is usually well tolerated but does results in gastocnemius weakness, which can make it difficult for a patient to stand on the toes. S4, S5, and the coccygeal nerves can usually be sacrificed without significant consequences. Loss of bilateral S2 and S3 nerve roots will result in loss of bowel, bladder, and sexual function. Unilateral S2 and S3 sacrifice usually allows a patient to have fairly normal bowel, bladder, and sexual function. Bilateral S3 sacrifice and S2 preservation will provide some function, but most patients will have difficulty with bowel, bladder, and sexual function.
Table 107-1 Deficits from Specific Nerve Root Sacrifice
| Nerve Sacrifice | Deficit |
|---|---|
| C3 and C4 | Possible diaphragm weakness |
| C5 | Deltoid weakness |
| C6 | Bicep weakness |
| C8 or T1 | Hand intrinsics weakness |
| T2–T12 | Dermatomal sensory loss |
| L1 or L2 | Iliopsoas weakness, usually compensated over time |
| L3 | Quadriceps weakness |
| L4 | Quadriceps weakness, knee proprioceptive difficulty, and footdrop |
| L5 | Footdrop |
| S1 | Minimal deficit |
| Unilateral S2 and S3 | Bowel/bladder/sexual function abnormal but functional |
| Bilateral S2 and S3 | Loss of bowel/bladder/sexual function |
| Bilateral S3 with S2 sparing | Some bowel/bladder/sexual function |
| S4, S5, and coccygeal nerves | Dermatomal sensory loss |
Level-Specific Challenges
Thoracic Spine (T2-12)
The thoracic spine (T2-12) has a unique advantage over other spinal segments in that the nerve roots in this region can be sacrificed with minimal morbidity. In performing a multilevel spondylectomy, increasing the number of nerve roots and segmental vessels that are sacrificed increases the risk of ischemic injury to the cord. The exact tolerance of the human spinal cord for ischemia has not yet been defined, and there is probably a fair amount of variability between patients. Kato et al. have described a canine model, in which they set out to determine the number of segmental vessels that can be ligated before ischemia occurs.2 They found that the interruption of bilateral segmental arteries of four or more consecutive levels, including the level of the Adamkiewicz artery, risks producing ischemic spinal cord dysfunction.
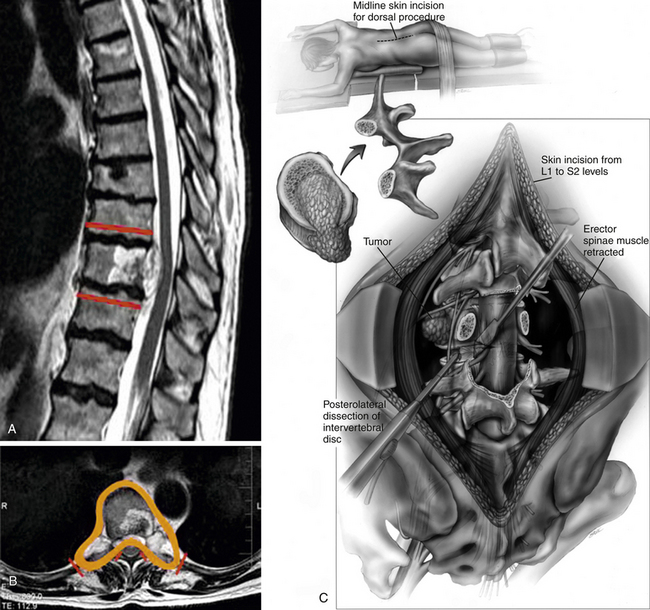
Tumors that are located ventrally, in the vertebral body, will need to undergo a preparatory stage from a dorsal approach. The approach is a standard midline approach with a subperiosteal exposure and exposure of the level of interest and two to three levels above and below index level(s) (Fig. 107-2A). Laterally, the exposure is carried out over the ribs for at least 6 cm on either side. Preoperatively, the MRI and CT are examined critically to understand exactly how far into the dorsal elements the tumor might extend. If the tumor extends into the pedicles and transverse process, this portion of the vertebral segment cannot be violated and must be dissected such that it can remain in continuity with the specimen3 (Fig. 107-2B). The dorsal elements that are uninvolved with tumor at the index level(s) are removed, as are the dorsal elements above and below this level (Fig. 107-2C). Because the spinal column will be completely destabilized after the resection, instrumentation is placed at this part of the operation. The ribs at the index level(s) and the level above and below are cut 6 cm lateral to the transverse processes and, if not involved in tumor, are removed and retained as graft material. Care is taken not to injure the neurovascular bundle or pleura ventral to the rib.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree