Figure 46.1. Subtype mechanism of ischemia in patients between 20 and 44 (white bar) and more than 45 years (black bar) of age at first stroke in the Northern Manhattan Stroke Study [Jacobs, 2002].
The NOMASS study, like other epidemiological studies, shows that the incidence, prevalence and consequences of stroke differ across different racial or ethnical groups. In younger patients, the relative risk of stroke in Hispanic or African-Americans is about 2.5 times higher than in white Caucasians. Even more significant are the racial differences observed in the Greater Cincinnati/Northern Kentucky Stroke Study which involved 3136 patients with first stroke. The sample analyzed a biracial metropolitan population composed mostly of white Caucasians (~70%) and African-Americans (29%). Compared to Caucasians, the relative risk of first stroke in African-Americans was 2.2 for those under 35 years of age, 5.0 for those aged 35-44 years, and 2.6 for those aged 45-54 years. These racial differences were attenuated at older ages (Figure 46.2).
Although the causes of these differences have not been determined, epidemiological studies suggest differences in vascular risk factors. Population studies show an increased prevalence and suboptimal control of cardiovascular risk factors (hypertension, diabetes, and obesity) in populations with low socioeconomic status and a higher prevalence of smoking in middle-high socioeconomic levels.
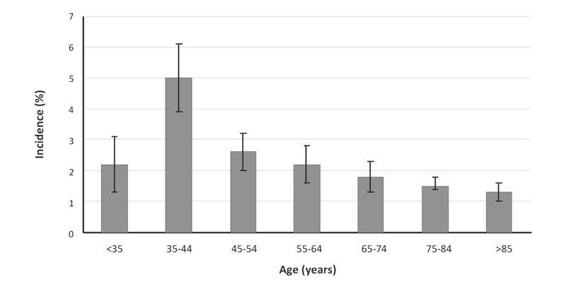
Figure 46.2. Relative incidence of first stroke by age in African-Americans as compared to whites in the Northern Manhattan Stroke Study [Jacobs, 2002].
46.2.2 Prevalence
In 2005, the “Behavioral Risk Factor Surveillance System” (BRFSS) survey was performed in the United States. The study used randomly generated telephone numbers for questioning the civilian outpatient population over 18 years of age. Subjects had to answer the question “Have you ever been told by a doctor or other health professional that you had a stroke?”. Of a total of around 356,000 individuals, approximately 2.6% responded affirmatively. On the basis of the data obtained from this survey, it has been estimated that the prevalence of cerebrovascular disease is 0.8% in individuals aged 18-44 years, 2.7% for those between 45 and 64 years, and 8.1% in those over 65 years.
Many strokes are asymptomatic or unrecognized. This suggests that the prevalence of this disease is in the general population underestimated. The NOMASS study illustrates this concept. In this trial, 892 subjects aged 55 years and older who were never diagnosed with stroke were assessed by magnetic resonance imaging (MRI) of the brain. The overall prevalence of subclinical brain infarction was 17.7%. Due to the design of this study, no data are available for patients younger than 55 years. However, the prevalence of subclinical ischemic stroke in relatively young individuals (55-65 years) was 9.5%; this rate is higher than that expected on the basis of the information obtained in the BRFSS survey. Similar to what was observed with incidence, the prevalence of ischemic stroke in relatively young African-Americans (55-65 years) was significantly higher (28.9%) than that observed in Caucasians (4.1%). These results confirm that the prevalence of stroke in the general population, even in relatively young patients, is greater than estimated.
46.2.3 Risk Factors
Cerebral ischemia in adult patients is close linked to traditional cardiovascular risk factors like hypertension, hypercholesterolemia, diabetes, obesity, and smoking. The presence, severity and suboptimal control of these co-morbidities increase the risk of small-vessel atherosclerotic disease, large-vessel occlusive disease, cardiomyopathy, valvulopathy, and cardiac conduction disorders. A worrying observation is the exponential increase observed in the last two decades in the prevalence of vascular risk factors related to eating habits, sedentary lifestyle, obesity and diabetes. Population studies conducted in the United States indicate that these conditions affect mostly African-Americans and Hispanics.
Cardiovascular risk factors are the pathophysiological basis for the vast majority of strokes in adults. In young patients suffering from cerebral ischemia, the prevalence of cardiovascular risk factors is significantly higher than in the general youth population. As in adult patients, the severity of these risk factors is directly related to the risk of developing cerebral ischemia. For example, data obtained in the Stroke Prevention in Young Women Study show that the risk of stroke in young women between 15 and 49 years of age increases with the number of cigarettes smoked per day (odds ratio [OR] = 2.2 for 1 to 10 cigarettes/day, 2.5 for 11 to 20 cigarettes/day, 4.3 for 21 to 39 cigarettes/day, and 9.1 for 40 or more cigarettes/day).
46.3 Stroke Etiology in Young People
Stroke in adult patients is, in most cases, the result of endothelial injury caused by sustained exposure to vascular risk factors. As a corollary of this phenomenon, the vast majority of studies carried out to delineate the causes, evaluation, management and prognosis of cerebral ischemia have been conducted in groups of adult patients. However, as noted above, stroke in young patients differs significantly from that of adults. With a sample of 428 subjects, the Baltimore-Washington Cooperative Young Stroke Study is perhaps the largest epidemiological study carried out in 15 to 44 year-old patients with first stroke. The biracial population analyzed included approximately 60% of African Americans and 36% of Caucasians. In this study, about 50% of patients had at least one probable cause of stroke, 20% had at least one possible cause of stroke, and 30% had no probable or possible causes of stroke. The frequency distribution by cause of stroke seen in the first subgroup is summarized in Figure 46.3. Drug abuse, contraceptive use, thrombophilia and non-atherosclerotic arterial disease (including vasculitis and vascular dissection) are relatively uncommon causes of stroke in adult patients. However, in this study, these conditions were the etiologic factor for approximately 50% of cases of cerebral ischemia.
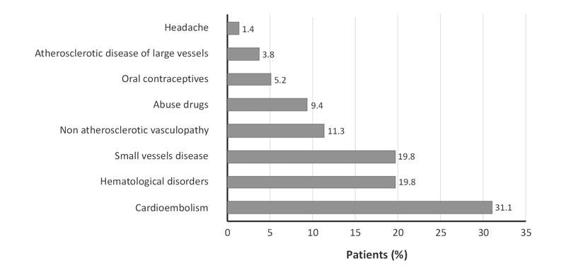
Figure 46.3. Causes of ischemic stroke in young patients (15-44 years) in the Baltimore-Washington Cooperative Young Stroke Study [Kittner, 1998].
Like other epidemiological estimates, vascular risk factors and causes of stroke vary with race or ethnic group studied. In a retrospective study including 264 young patients of Chinese origin aged between 15 and 45 years of age, the stroke subtype more frequently observed was the cryptogenic type (Figure 46.4).
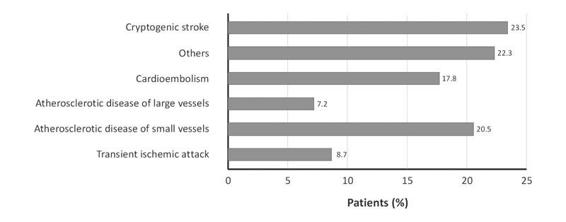
Figure 46.4. Causes of stroke in young patients (15-45 years) of Chinese origin [Lee, 2002].
The most prevalent risk factors were hyperlipidemia (53%), smoking (50%), hypertension (46%) and family history of stroke (29%). Within the subgroup with stroke due to other causes, the most common etiologies were arterial dissection (39%), antiphospholipid syndrome (17%), and Moyamoya disease (15%). Observed subtypes of stroke in epidemiological studies that include younger patients belonging to certain races or ethnic groups are summarized in Table 46.1.
Area | Age | n | Subtype (%) | ||||
ASVD | ALVD | CE | OC | C | |||
South America | |||||||
Brazil | 14-40 | 106 | 12.5 | 8.5 | 28.3 | 34.9 | 16.0 |
North America | |||||||
Canada | 14-45 | 356 | 8 | 6 | 14 | 28 | 44 |
USA-NOMASS** | 20-44 | 74 | 18 | 15 | 6 | 6 | 55 |
USA-BWCYSS | 15-44 | 428 | 10 | 2 | 15 | 23 | 32 |
Mexico | <40 | 300 | 3* | 24 | 40 | 32 | |
Asia | |||||||
Taiwan** | 15-45 | 241 | 22.4 | 7.9 | 19.5 | 24.5 | 25.7 |
Korea | 15-44 | 149 | 17.4 | 20.8 | 18.1 | 26.8 | 16.8 |
Europe | |||||||
Spain | 15-45 | 272 | 5 | 19.5 | 17.5 | 22 | 36*** |
Italy | 15-44 | 333 | 33.1* | 23.7 | 8.1 | 35.1 | |
Sweden | 18-44 | 107 | 4.7 | 12.1 | 32.7 | 29.9 | 20.3 |
Switzerland | 15-44 | 202 | 2.5 | 5.4 | 21.4 | 46 | 22.8 |
Table 46.1. Subtypes of stroke observed in epidemiological studies in young patients.
* Represents the sum of individuals and ALVD ASVD;
** Transient ischemic attack patients were not included;
*** Includes patients with cryptogenic stroke, with more than one possible cause, and incomplete assessments;
ASVD = atherosclerotic small-vessel disease; ALVD = atherosclerotic large-vessel disease; CE = cardioembolic; OC = other known cause; C = cryptogenic; NOMASS = Northern Manhattan Stroke Study; BWCYSS = Baltimore-Washington Cooperative Young Stroke Study.
Table 46.2 summarizes the conditions associated with the development of cerebral ischemia in young patients. The following sections discuss the most relevant pathologies.
Atherosclerotic arterial disease | |
NO-atherosclerotic arterial disease | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|



