Surgery for Kyphosis Associated with Ankylosing Spondylitis and Related Disorders
Theodore A. Bdanger
Daniel K. Riew
BACKGROUND
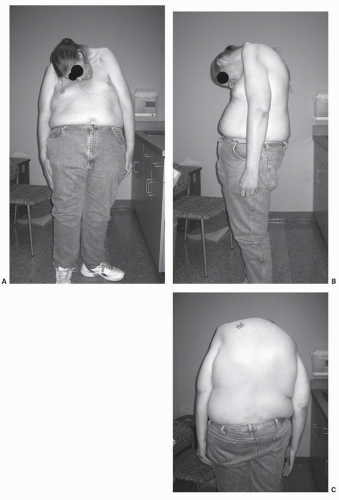
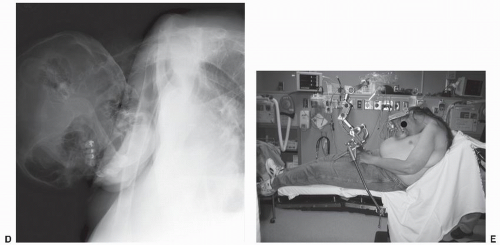
Among the cervical spinal deformities for which patients can seek surgical treatment, few are as dramatic or as challenging as kyphosis of the spine related to ankylosing spondylitis (AS) (Fig. 91.1A-D and 91.1). Surgery for this clinical problem requires exacting planning and execution in order to achieve success and avoid serious complications such as quadriplegia or death. While keeping this word of caution in mind, it should also be noted that a successful cervicothoracic extension osteotomy in a patient with AS can be life-transforming for the patient and therefore is often very rewarding.
Patients with AS develop rigid spines secondary to progressive bony ankylosis across their facet joints and intervertebral disks (1,2). Kyphotic deformity of the spine may develop as the disease progresses. They complain of spinal stiffness, back or neck pain, and difficulty standing erect. Their physical examination is characterized by kyphotic deformity, spinal stiffness (proven with Schober’s test), and absent costovertebral motion resulting in “abdominal breathing” (1, 2, 3, 4 and 5). AS affects men far more commonly than women (9:1) and generally more severely and at a younger age (15 to 30 vs. 25 to 40 years of age) (1,2). Most patients with AS are HLA-B27 positive (90%), but most people who are HLA-B27 positive will never develop AS (98%), which limits the usefulness of testing for this genetic marker. Radiographically, these patients have osteopenia, squaring of vertebral bodies, bridging marginal syndesmophytes, sacroiliitis, diminished or reversed lumbar lordosis, and exaggerated thoracic kyphosis. Advanced cases will have total ankylosis across the sacroiliac joints and the classic “bamboo spine” appearance (1,2). Occasionally, an AS patient will present with atlantoaxial instability due to transverse ligament attenuation or fracture of the dens, usually in the setting of ankylosis of the cervical spine. Other presentations include severely unstable fractures from low-energy trauma or a hypermobile pseudarthrosis of the spine (historically known as “spondylodiskitis” or the “Andersson lesion”), which may be a result of an unrecognized, nonunited fracture or a remnant of progressive ankylosis of the rest of the spine causing concentration of motion at one remaining segment that never ankyloses. This has the radiographic appearance of a hypertrophic nonunion (1, 2 and 3). There are several nonspinal manifestations of AS that occur, including restrictive pulmonary disease from rib ankylosis (100%) and/or pulmonary fibrosis (rare, late), hip or other peripheral joint involvement (25%), cardiac abnormalities such as aortic valve (10%) or conduction defects (4%), inflammatory eye disorders such as iritis/anterior uveitis (30%), inflammatory bowel disorders such as Crohn’s disease or ulcerative colitis, and amyloidosis (rare) (1,2,6). Patients with AS have diminished life expectancy, mainly due to cardiac concerns, but are also known to suffer more frequently than the average population from psychiatric issues such as alcoholism, depression, and suicide (7).
The focus of this chapter is on surgical treatment of AS patients who present with a functionally significant kyphosis of the cervical spine or cervicothoracic junction (2, 3, 4 and 5,8, 9, 10 and 11). In the extreme, they present clinically with “chin-on-chest” deformity. Rigid apposition of their chin to their chest contributes to impairment of horizontal gaze, hygiene, shaving, chewing, and swallowing. Many patients have neck pain secondary to fracture or continuous muscular effort to compensate for their deformity. Some will also have features of global sagittal imbalance (flat-back syndrome), which must be evaluated contemporaneously to determine which issue is of greater clinical concern (4).
In addition to the clinical appearance of chin-on-chest deformity and the associated symptoms of that rigid posture, it is also important to note that neurologic abnormalities are common at the time of presentation. In the series published by the author, 10 of 26 patients who had
undergone cervicothoracic osteotomy had presented with myelopathy ranging from mild to severe (2). This may be due to an acute or chronic fracture or due to the more subtle, gradual spinal cord compromise due to kyphosis and relative elongation of the spinal cord as the deformity progresses. Notably, these deficits generally improve with successful realignment via osteotomy (2,11).
undergone cervicothoracic osteotomy had presented with myelopathy ranging from mild to severe (2). This may be due to an acute or chronic fracture or due to the more subtle, gradual spinal cord compromise due to kyphosis and relative elongation of the spinal cord as the deformity progresses. Notably, these deficits generally improve with successful realignment via osteotomy (2,11).
Urist first reported his experience with an extension osteotomy done for severe cervical flexion deformity in a patient with AS in 1958. He reported a technique similar to a Smith-Petersen osteotomy previously reported in the lumbar spine, done with the patient in the seated position under local anesthesia. He pointed out the advantages that the unique anatomy of the C7/T1 level has over the rest of the cervical spine, including a relatively wide spinal canal with more mobile exiting (C8) nerve roots and less proximity of the vertebral arteries that enter the foramen transversarium at the C6 level (3,10). Since then, several authors have reported their experience with the technique, with some variations along the way. The largest series to date detail the career-spanning experience of Edward H. Simmons (11) who reported a series of 131 patients over the course of 36 years, and of Henry H. Bohlman who reported the results of 26 patients over the course of 25 years (4). The reader is referred to those original references for additional advice from those distinguished and experienced authors.
INDICATIONS AND CONTRAINDICATIONS FOR SURGICAL TREATMENT
There is not a universally applicable treatment algorithm to apply to a clinical situation as complex as this one. The decision to proceed with cervicothoracic osteotomy for chin-on-chest deformity associated with AS must be based on the consideration of several factors. Complaints of persistent, severe symptoms that correspond to clinically and radiographically severe deformity are the cornerstones of decision-making (2, 3 and 4,11, 12 and 13). The presence of an acute fracture in this setting requires careful handling and is dealt with in a separate chapter in this text. When a chronic, occult fracture (or “spondylodiskitis”) is present in the context of severe deformity as a contributing factor, this needs to be given additional weight in surgical decision making.
In general, the AS patient (without a fracture) must have severe disability as a result of the deformity, usually quantified in terms of difficulty with horizontal gaze, chewing
and swallowing, and hygiene tasks such as shaving; pain; and neurologic complaints. Such patients may have signs of myelopathy but often are severely debilitated even when neurologically normal. Standard workup includes thorough history and physical examination focusing on complaints, deformity, and neurologic status, as well as general medical status. Understanding the severity and influence of medical comorbidities is imperative. Attention must be paid to the nonspinal abnormalities common in AS, as they may impact surgical decision-making significantly. Full-length standing radiographs must be obtained with the knees fully extended, supplemented by focused images centered on each region of the spine deemed necessary by the treating surgeon. Advanced diagnostic imaging via computerized tomography (CT) and/or magnetic resonance imaging (MRI) can help the surgeon understand the anatomy and identify issues such as occult fractures, which are often low energy and can contribute significantly to the progression of deformity and the worsening of symptoms.
and swallowing, and hygiene tasks such as shaving; pain; and neurologic complaints. Such patients may have signs of myelopathy but often are severely debilitated even when neurologically normal. Standard workup includes thorough history and physical examination focusing on complaints, deformity, and neurologic status, as well as general medical status. Understanding the severity and influence of medical comorbidities is imperative. Attention must be paid to the nonspinal abnormalities common in AS, as they may impact surgical decision-making significantly. Full-length standing radiographs must be obtained with the knees fully extended, supplemented by focused images centered on each region of the spine deemed necessary by the treating surgeon. Advanced diagnostic imaging via computerized tomography (CT) and/or magnetic resonance imaging (MRI) can help the surgeon understand the anatomy and identify issues such as occult fractures, which are often low energy and can contribute significantly to the progression of deformity and the worsening of symptoms.
Patients with severe involvement from AS may have global sagittal imbalance as well as chin-on-chest deformity. Hip flexion contractures may also contribute to their global posture difficulties. It is incumbent on the surgeon to understand what contribution each problem makes to the clinical situation. If a given AS patient has severe involvement from both sagittal imbalance and chin-on-chest deformity such that an extension osteotomy is contemplated in both the lumbar and cervical regions, it is generally recommended that the surgeon should first address the lumbar osteotomy and secondarily consider the cervical procedure (4). Often, performing a lumbar osteotomy will address the patient’s complaints well enough (by improving their global posture and horizontal gaze) that a cervical procedure can be obviated. Conversely, if the reverse order is undertaken, the surgeon may be prone to misjudge the degree of correction that needs to be achieved with the cervical procedure, only truly understanding that the patient was overcorrected or undercorrected after a lumbar osteotomy is performed and the final result is viewed clinically. Since AS patients’ spines are rigid, they cannot compensate very well for miscalculations in their spinal alignment. In any given patient, the relative contribution from the hips and each region of the spine needs to be considered carefully in order to optimally prioritize and plan any surgical intervention.
Cervicothoracic extension osteotomy is contraindicated when the major deformity is in the lower thoracic or lumbar spine or in the hips. Medical issues such as severe cardiac or pulmonary disease, clotting abnormalities, or psychiatric disturbance that might interfere with postoperative compliance or rehabilitation are also contraindications to this type of surgery (2,4).
SURGICAL TREATMENT OF CHIN-ON-CHEST DEFORMITY ASSOCIATED WITH ANKYLOSING SPONDYLITIS (SMITH-PETERSEN OSTEOTOMY)
The surgical technique of choice for severe kyphosis of the upper thoracic or cervicothoracic spine in AS is a dorsal extension osteotomy at the cervicothoracic junction (1, 2, 3, 4 and 5,8, 9, 10, 11, 12, 13, 14 and 15). This technique is analogous to a Smith-Petersen osteotomy of the lumbar spine, in that the surgeon creates a dorsal wedge-shaped defect via laminectomy and facetectomy (at the cervicothoracic junction) and completes the osteotomy via osteoclasis, extending the spine at the osteotomy site until the desired correction is achieved. The spine is then fixed in this position internally, externally, or both (Fig. 91.2, 91.2, 91.2, 91.2 and 91.2). A pedicle subtraction osteotomy of C7 (also known as a decancellation or eggshell osteotomy) has also been described, and the details of the technique will be illustrated separately (14).
Preoperative planning needs to be meticulous (4). Medical clearance should include pulmonary function testing and cardiac clearance since all AS patients have restrictive pulmonary disease, and many have cardiac involvement. The lack of costovertebral motion and kyphotic alignment contribute to poor breathing mechanics, diminished lung volumes, and an impaired cough. A clear understanding of the severity of these issues is important to determine the wisdom of operating, the safe administration of anesthesia, proper airway protection, and postoperative ventilator management. If the patient is a smoker, an additional note of caution is in order, and abstinence prior to surgery is wise. Preoperative dysphagia and/or malnutrition may necessitate placement of a PEG tube for preoperative nutritional repletion and postoperative feeding. Transient worsening of dysphagia is common in these patients after corrective osteotomies.
Preoperative studies should include full-length spinal radiographs and focused cervical and/or cervicothoracic junction radiographs in the anteroposterior and lateral projections. Advanced axial imaging such as CT, with or without contrast or myelography dye, or MRI should be done preoperatively to define the anatomy and pathology in detail, with emphasis on identifying important vascular structures (vertebral arteries) and looking for spinal canal compromise, occult fractures, or atlantoaxial instability that may affect surgical planning. Standard CT or MR angiography may be helpful in clarifying vertebral artery anatomy, which is relevant in the cephalad segments where fixation points may be planned (i.e., C2 pedicle screws, C1 lateral mass screws, transarticular C1/C2 screws). Since the vertebral arteries generally enter the spine caudally in the foramen transversarium at C6, the osteotomy is generally performed at the C7/T1 level. Estimation of the amount of correction to be achieved is also done preoperatively, both by evaluation of the patient clinically in the standing position and on lateral radiographs. The chin-brow vertical angle (CBVA) is determined and correction planned to position the head with slight residual kyphosis (roughly 15 degrees of CBVA). Overcorrection is poorly tolerated because the patients will be unable to see the floor at their feet and their rigid spines make it impossible to compensate. Such a situation may require revision surgery.
Preoperative planning must also include consideration of how the osteotomy will be stabilized at the time of surgery. Historically, external immobilization had been used with a Risser body cast and halo ring (2, 3, 4 and 5,8, 9, 10 and 11). A halo vest, which generally goes only over the rib cage, is generally regarded as inferior to a Risser cast, which can gain better fixation around the pelvis and torso. Given the
severe thoracic hyperkyphosis in these patients, halo vests will often fit poorly over the chest and in the worst scenarios may restrict abdominal breathing if they extend too low over the abdomen. An abdominal cutout can be made in a Risser cast to accommodate the abdominal expansion necessary for these patients to breathe. This form of immobilization has traditionally been used either as a stand-alone form of stabilization or to supplement previous generation, less-than-rigid internal fixation (i.e., wiring, Luque rectangle) (2, 3 and 4,11). If rigid internal fixation is to be used, then less extensive external immobilization may be required at the surgeon’s discretion (12, 13, 14 and 15).
severe thoracic hyperkyphosis in these patients, halo vests will often fit poorly over the chest and in the worst scenarios may restrict abdominal breathing if they extend too low over the abdomen. An abdominal cutout can be made in a Risser cast to accommodate the abdominal expansion necessary for these patients to breathe. This form of immobilization has traditionally been used either as a stand-alone form of stabilization or to supplement previous generation, less-than-rigid internal fixation (i.e., wiring, Luque rectangle) (2, 3 and 4,11). If rigid internal fixation is to be used, then less extensive external immobilization may be required at the surgeon’s discretion (12, 13, 14 and 15).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree