Surgery for Posttraumatic Kyphosis
Maneesh Bawa
Steven R. Garfin
Sagittal balance of the spine is designed to position the head over the pelvis. This minimizes the muscular effort necessary to maintain an upright posture and be bipedal (1). Cervical lordosis is critical to normal sagittal plane balance of the spine. It compensates for thoracic kyphosis and lumbar lordosis. Cervical kyphosis is defined as an anterior angulation of the head in the sagittal plane (2). It can be diffuse throughout the cervical spine or segmental. Segmental kyphosis is present when there is an angular relationship between two vertebrae with a posteriorly directed apex. Cervical kyphosis alters the biomechanics of the neck. There are many causes of cervical kyphosis, including trauma, tumor, surgery, congenital deformities, musculoskeletal dysplasias, inflammatory conditions, neuromuscular condition and degenerative diseases. This chapter focuses on cervical kyphosis associated with previous trauma. The prior injury may or may not have been recognized and treated. Prior treatment may not have fully accounted for the nature of the injury. Or the treatment may have been well designed and executed but failed to prevent evolution of a sagittal plane deformity due to host factors, such as metabolic bone disease, noncompliance, nicotine addiction, or simply bad luck. But once recognized, posttraumatic kyphosis may require treatment.
ANATOMY AND BIOMECHANICS
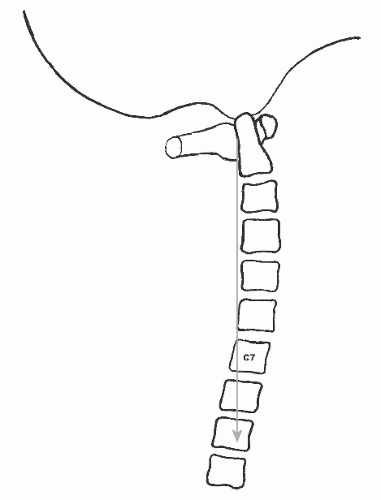
The normal weight-bearing axis of the head (sagittal vertical axis) passes through the middle of the C1 and T1 vertebral bodies and falls behind the C2 through C7 vertebral bodies (Fig. 88.1) (3). The normal mean sagittal contour of the adult cervical spine is 14.4 degrees of lordosis (4). Anatomically, the cervical spine is composed of an anterior column made up of the vertebral bodies, disks, and associated ligaments, and a posterior column made up of the facet joints, laminae, and posterior ligamentous structures (2,5,6). The normal lordotic cervical spine distributes 36% of the axial compressive load through the anterior column and 64% of the load through the posterior column. Thus, each side of the posterior column supports 32% of an applied axial load (7). Ligament sectioning studies have documented the importance of both the anterior and posterior osteoligamentous structures in maintaining spinal stability. With regard to the development of kyphosis, at least one of the posterior columns in addition to an intact anterior column is required to prevent failure of the spinal segment (5,6).
The dorsal osteoligamentous complex, in particular the facet joints and the ligamentum flavum, is critical to the maintenance of a lordotic cervical posture. Using finite element analysis, Saito et al. (8) found that loss of one or more posterior elements (such as the spinous process, ligamentum flavum, or intraspinous ligaments) subjected the facet joints to tensile forces rather than the normal compressive loads. A unilateral facetectomy decreased the strength of the vertebral motion segment by 31%, whereas bilateral facetectomy resulted in a 53% decrease in strength during axial loading. In addition, facetectomy caused anterior displacement of the instantaneous axis of rotation in the sagittal plane, leading to increased compressive loads on anterior column structures (9). Kumaresan et al. (10), using finite element analysis, demonstrated that removal of more than 50% of the facetjoints bilaterally transferred high stresses to the annulus fibrosis during flexion and rotation. Both Raynor and Carter (11) and Zdeblick et al. (12,13) demonstrated flexion and torsional instability with resection of more than 50% of the facetjoint. Fifty percent facetectomy allowed exposure of only 3 to 5 mm of a nerve root but did not result in failure at the facet joint. A 70% facetectomy allowed exposure of 8 to 10 mm of a nerve root but resulted in failure via a fracture at the facet joint during shear loading (11). Nowinski et al. (14) demonstrated significantly increased motion with resection of as little as 25% of the facet joint in a multilevel laminectomy model. Indeed, one of the most common causes of cervical kyphosis is iatrogenic, after multilevel laminectomies. Similarly, a dorsal ligamentous injury or a facet fracture can lead to kyphosis if not recognized and adequately treated.
Injury to the anterior column can also lead to kyphosis with inability to resist compressive loads. The disks make up about 15% of cervical height and are normally slightly trapezoidal, with a greater height anteriorly than posteriorly. Collapse of the vertebral body secondary to fracture or loss of disk height secondary to a disk injury can contribute to cervical kyphosis. This alters the biomechanics of the neck, creating tensile and shear forces to the posterior column, and shifts the weight-bearing axis more anteriorly.
In addition to the bony and ligamentous structures, cervical musculature also plays a role in maintaining normal cervical lordosis. Some have argued that extensor muscle paralysis does not necessarily lead to notable instability as long as the bony and ligamentous restraints remain intact (15). However, an in vitro study demonstrated that any forward shift in the gravitational center of the head promoted cervical kyphosis (8). Nolan and Sherk (1), studying the extensor musculature, found that the semispinalis cervicis and capitis were primarily responsible for extension of the spine and that about 14 kg of force was required to maintain the head in an upright position. They emphasized the importance of preserving the attachment of the muscles to the C2 arch whenever possible. Finally, muscle denervation and fibrosis secondary to aggressive retraction or neuromuscular disorders can lead to the development of a kyphotic deformity (16,17).
Regardless of the initial pathology, kyphosis initiates a vicious cycle of abnormal forces that can result in the development of a progressive deformity (3). As the head shifts forward, the weight-bearing axis is translated anteriorly, causing the anterior column to be loaded with increased compression, while the posterior column is placed under increased tensile loads. Posterior extensor muscles are elongated and placed at a mechanical disadvantage, becoming less effective at holding the head upright (1). The dorsal ligamentous complex also becomes attenuated and contributes to the kyphosis. This causes the neural elements to be translated forward, becoming draped over the kyphosis and resulting in spinal cord dysfunction (Fig. 88.2). This can lead to a triad of progressive deformity, neurologic compromise, and further stretching of the dorsal soft tissue restraints.
Ventral compression of the spinal cord is generated as it is pulled against the apex of the deformity. This can result in irritation or dysfunction of the cord, or nerve roots, or both. Just like the forces on the osteoligamentous structures in cervical kyphosis, the spinal cord is subject to similar forces. In the dorsal spinal cord, tensile forces predominate, while the ventral spinal cord is compressed against an osteophyte or protuberant disk. The spinal cord may also be subjected to a bending load across the apex of the kyphosis. This can result in tethering. The additive effect of these internal stresses results in complex changes within the spinal cord, including potential compromise of cord microvasculature resulting in ischemia. Variations in cord stresses and ischemia are partly responsible for the wide spectrum of neurologic manifestations observed in patients with a cervical kyphotic deformity (18,19).
CLINICAL PRESENTATION
The symptoms of cervical kyphosis can vary depending on the nature and severity of the underlying condition. The most commonly experienced symptoms include radiculopathy, myelopathy, neck pain, muscle fatigue, and/or loss of forward gaze.
Initially, patients may be asymptomatic and have only neck pain or mild radiculopathy secondary to their trauma. How quickly this progresses depends upon the initial pathology. The initial symptom typically is worsening neck pain and, if left undiagnosed or untreated, can lead to radiculopathy and myelopathy. The worsening neck pain can be due to muscle fatigue and spasm, instability, or both. Myelopathy can present as subtle clumsiness in the hands, gait unsteadiness, or sphincter dysfunction. Signs of hyperreflexia and pathologic reflexes such as Hoffmann and Babinski signs should be assessed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree