Figure 85.1. Proposed algorithm for the evaluation of patients with multilobar and multilesional epilepsy. The algorithm departs from the findings in the brain MRI. The first element to consider is whether lesions in contiguous lobes or not. Contiguous lesion algorithm continues on the left side of the scheme with next step focused in the relationship of the lesion with the eloquent cortex and the presence of functional neurologic deficit. Noncontiguous lesions follow the path of the right side of the scheme with the next step determining if the lesions are noncontiguous in the same hemisphere or bihemispheric and the presence or not of functional neurologic deficit or involvement of the eloquent cortex. Cases illustrating the use of the algorithm can be found at the end of the chapter.
SELECTION OF CASES WITH MULTILOBAR AND MULTILESIONAL EPILEPSY FOR SURGICAL CANDIDATES
The selection of surgical cases from patients with multilobal and multilesional epilepsy is based on several factors: brain MRI findings, VEEG, other neuroimaging techniques, and clinical data, including seizure semiology and findings of the clinical exam.
MRI FINDINGS
The role of the MRI in the identification of surgical candidates has been well established. The proposal from the Pediatric Epilepsy Surgery Subcomission (17) and the practice parameters of the Quality Standards Subcommittee of the American Academy of Neurology (18) mandate a brain MRI using a specified epilepsy protocol as part of the minimal presurgical evaluation of children and adults for temporal lobe and neocortical epilepsies. Brain MRI is a diagnostic tool that is readily available in most epilepsy centers around the world, particularly those in developed countries (19).
The definitions of multilobar and multilesional epilepsies used in this chapter will be based on brain MRI findings. The results of the brain MRI are the first step at the beginning of the algorithm proposed in Figure 85.1. A brain MRI will identify the type, etiology, and location of a lesion. Although the etiology of the lesion is important in following the algorithm, for surgical planning purpose, the location of the lesion is equally important.
Etiology of the Lesion
The MRI findings in multilobar epilepsies include dysplasias, hemimegalencephalic syndromes, Sturge–Weber syndrome, Rasmussen encephalitis, polymicrogyria, periventricular encephalomalacia, or other encephalomalacias from trauma, stroke, tumors, etc.
MRI substrates in multilesional epilepsies include tuberous sclerosis complex, inflammatory and postinfection lesions, bilateral strokes or watershed infarcts, tumors, and vascular malformations.
All these etiologies are discussed in detail in Section B of this book. The frequency with which these lesions are seen in tertiary epilepsy centers has been extensively discussed in the medical literature. Cortical dysplasia remains the most common of all multilobar and multilesional epilepsies. Nevertheless, one community-based epidemiologic study of lesions identified by brain MRI in children with epilepsy found that 16% of the children (82 out of 518) had abnormalities in the brain that could be responsible for their epilepsy (20). 37% of the patients in this group had pre- and perinatal-acquired cerebral injuries, 27% had cortical dysplasia, 22% had other discrete lesions such as tumors, and 15% had lesions associated with genetic conditions.
Location and Extent of the Lesion
The brain MRI will help to determine whether the lesions are located within one hemisphere or are bilateral, and whether the lesion(s) is unilobar or multilobar. The brain MRI also determines whether the lesion is cortical, subcortical, or both and its relationship with the eloquent cortex. Cortical lesions located near the eloquent cortex, as well as lesions located near the major tracks (pyramidal tract, optic tract, arcuate fasciculus, etc.), put the patient at risk for neurologic deficit during surgical resection. Adding Diffusion Tensor Imaging (DTI) sequences could help with the surgical planning in such cases (21,22).
Forty-six percent of the cases in a community-based study involved bihemispheric brain lesions (20). We have learned in recent years that bilateral lesions do not preclude successful epilepsy surgery (23).
In addition to brain MRI, surgical decision in patients with multilobar and multilesional epilepsy includes data from other imaging modalities such as PET, SPECT, and DTI. In some patients MRI postprocessing are needed. The role of these techniques in the evaluation of epilepsy surgical candidates is covered in Chapters 75, 77, and 78.
Refractory Epilepsy
Since our surgical selection algorithm is based on brain MRI findings, this chapter minimally discusses the role of refractory epilepsy and incidental findings in patients with nonsurgical epileptic syndromes or patients with epilepsy-related findings in brain MRI who never have had a seizure.
Refractory epilepsy is defined as the failure of two to three drugs that are used appropriately and adequately for the seizure type, although some variations on time of seizure freedom and time required from onset of seizures to time of evaluation have been used for research purposes (17,18,24,25). While brain MRI opened a new era in epilepsy surgery, its results must be interpreted with caution and in the appropriate clinical setting before referring the patient for epilepsy surgery. One study reported incidental brain abnormalities in 23% of normal children (26). A study of candidates for cochlear implants found incidental or unexpected brain abnormalities in 18% of the sample, including a few cases of periventricular nodular heterotopia (27). The incidental findings of brain lesions led to additional investigation and sometimes to surgeries—for example, in cases with brain tumors. A more complicated situation occurs when the patient has a history of epilepsy or seizures. Incidental brain abnormalities have been described in 3% of children with idiopathic epileptic syndrome and 10% of children with nonidiopathic epilepsy, normal neurologic exams, and nonpharmacoresistant epilepsy (20). Thus, the definition of refractory epilepsy is necessary but not indispensable for the referral for epilepsy surgery. A community study found that 6 of the 82 children with epilepsy as well as brain abnormalities and brain tumors (4 neoplasias and 2 DNETs) underwent surgeries even when their epilepsy was not pharmacoresistant (20).
Clinical Aspects: Semiology, Exam Findings, Weight, and Age
Semiology
The semiology of the seizures, specifically early in the course of seizures, is very important when considering epilepsy surgery. The presence of focal features can point to a specific brain region or location (15,28–32). Auras, lateralizing signs, and postictal symptoms are also very important in assigning both hemispheric and lobar localizations (28,30,33).
Semiology is even more critical in patients with multilobar or multilesional substrates. In multilobar cases, semiology may help predict early seizure spread in relationship to a large lesion. For example, in patients with posterior quadrant dysplasia, limb clonic or versive seizures at the onset may suggest anterior ictal spread. Hypomotor semiology may suggest a posterior spread. In multilesional patients, semiology may help narrow down the inventory of lesions that could possibly result in the semiology. More than one semiology during VEEG may suggest multiple ictal-spread patterns from one region or multiple independent seizure-onset zones. Hence, a critical review of history and VEEG with an appropriate sampling of seizure data is vital to building an effective surgical strategy.
Age-related syndromes in infants and children, such as epileptic spasms or Lennox–Gastaut-type seizures, could be the manifestation of focal epilepsy secondary to a focal, unilobar, multilobar, or hemispheric lesion (15,32,34,35). Seizures characterized by arrest of activity with very subtle limb movements and/or automatisms are also seen in this group, and some seizures with clear asymmetric features fail to point to a generalized or a focal epilepsy (15,36). Detailed evaluation of seizure semiology during VEEG becomes very important in these cases.
Clinical Exam
The clinical exam is equally important when determining the type of brain surgery to be performed. In addition to the proximity of the lesion to the eloquent area, the presence of motor deficit, hemianopsia, neglect, etc., are important when deciding the extension of the surgery. The degree of motor deficit is equally important. The possibility of a new neurologic deficit is a deterrent to patients and relatives when considering epilepsy surgery, and worsening of an existing neurologic deficit is also not desired. Risk of neurologic deficit was the cause for refusing resection in seven of nine children with subdural grids who were studied at the Cleveland Clinic (37). In these cases, an early consent discussion that includes clearly defined risks and benefits could lead to alternative or palliative treatments. In some patients, assessment of hemiparesis may be difficult because it fluctuates with acute worsening and recovery over weeks to months. Such phenomenon is seen in Rasmussen’s. This is also reported in Sturge–Weber syndrome where a component of ischemia makes a pattern of observation over time more important rather than one-time assessment. Occurrence of epilepsia partialis continua in patients of Rasmussen’s, poststroke cases, and rarely in focal cortical dysplasia makes this even harder as the patient may not be able to cooperate or part of the deficit could be ascribed to Todd paralysis.
Weight and Age
These are important factors in scheduling surgery. Infants as young as 1 month and weighing 4 kilograms have undergone surgery for catastrophic epilepsy (14,15,38). Although operative risks are greater in very small infants or the elderly, there are no absolute age or weight limitations for epilepsy surgery if seizures are difficult to control. The expertise and comfort of the neurosurgeon and the hospital team are the ultimate determining factors.
THE SELECTION OF THE SURGICAL PROCEDURE
Multilobar Resection/Disconnection
Patients with multilobar and multilesional epilepsy involving contiguous lobes and located in or near eloquent cortex are candidates for multilobar resection or disconnection, assuming the absence of a significant preexisting neurologic deficit. These cases may require additional invasive evaluation if a more tailored surgery is possible or desired.
A variety of multilobar resections or disconnections can be performed, depending upon the location of the lesion and information provided from the presurgical and invasive evaluations. Types of multilobar resections or disconnections include occipital plus, frontotemporal (FT), temporoparietal (TP), and frontoparietal (12,39,40).
The most common type of multilobar resection or disconnection is the occipital plus or posterior quadrant surgery. The posterior quadrant resection/disconnection includes temporoparietal–occipital (TPO), parietooccipital (PO), and temporo-occipital surgeries. The most common of these procedures is the TPO, which accounts for 21% to 46% of the multilobar resections or disconnections (12,39,40). In adults, TPO is less commonly performed and only accounts for approximately 5% of the surgeries (12,41,42). The TPO is selected when data support the fact that the frontal lobe is free of lesions, is not epileptogenic, and can be preserved. It is also the procedures of choice when there is need to preserve the motor and sensory cortex.
The decision to perform a multilobar resection versus a disconnection depends on the experience and expertise of the center. Daniel et al. described a series of patients in which the selection of the technique changed over the years. Earlier surgeries included anatomical posterior quadrantectomy or TPO resection; years later, the predominant procedure was the functional posterior quadrantectomy or extended temporal lobectomy with PO disconnection. Peri-insular posterior quadrantectomy has been described as the latest approach for posterior quadrant epilepsy (43). This technique includes disconnection of the temporal lobe followed by disconnection of the PO lobes during the same surgical procedure (39,42,43). Other approaches— rationale of this is not clear—such as a two-stage procedure with PO lobectomy followed by a temporal lobectomy in a separate surgery were used in some of the patients (43). Etiologies for occipital plus resections include malformation of cortical development, sequels of stroke or other vascular injuries, tumors, tuberous sclerosis, and Sturge–Weber syndrome. In general, occipital plus resection has a better long-term outcome than FT and TP resections.
Variations of focal resections with or without multiple subpial transections have been described in patients with perirolandic epilepsy (44). Nevertheless, seizure outcome with complete seizure freedom has been reported only in 31% of the cases with new neurologic deficits present in up to 23% of the cases. In other patients with multilobar lesions in which sparing of the motor cortex is desired, proposed surgery includes the premotor resection of the frontal lobe combined with a TPO resection (44,45). This technique provides seizure improvement but not freedom. Random cases with multifocal epilepsy can have improved quality of life when the resection is targeted toward the region producing more disabling or frequent seizures (46).
Hemispherectomy, Hemispherotomy, and Other Disconnective Procedures
Patients with epilepsy secondary to large multilobar brain lesions generally undergo hemispherectomy, although there are some exceptions, particularly when the surgical procedure is risking a new neurologic deficit.
Hemispherectomy or other disconnective procedures may be indicated for patients with multilobar and multilesional epilepsy involving contiguous lobes and located in or near the eloquent cortex who have a preexisting significant, complete or nearly complete neurologic deficit (47,48). In some patients with this scenario, the benefits from hemispherectomy may outweigh the risks of continuing seizures, hence favoring a more aggressive approach. In some patients with Rasmussen syndrome, hemispherectomy may be preemptively done due to anticipated deficits. Although quite controversial and not a widely accepted practice, there is a school of specialists who believe patients with Sturge–Weber syndrome should get early hemispherectomy rather than a focal resection. Etiologies for patients with epilepsy who require hemispherectomy include Rasmussen encephalitis, vascular or posttraumatic encephalomalacia, in particular perinatal infarction, cortical dysplasia, and hemimegalencephaly. Pathologic analysis of samples from 34% of patients with encephalomalacia found additional abnormalities consistent with cortical malformation (48). Functional or anatomical hemispherectomy is a procedure that is very well tolerated in infants and young children with catastrophic epilepsy (49). Compelling data indicate that the presence of mild or moderate MRI abnormalities in the hemisphere contralateral to the one with the main MRI abnormality is not a contraindication for epilepsy surgery. Surgery in these cases has a short-term positive outcome of 79%, compared to results in patients who did not have contralateral abnormalities (23). Similarly, patients with generalized epilepsy and generalized or contralateral EEG findings, who had congenital, perinatal, or early-acquired brain lesions on MRI, underwent successful epilepsy surgery (35,50). Sixty-four percent of patients in the series reported by Wyllie et al. received a hemispherectomy, and 14% had a posterior quadrant or occipital plus resection. Seven out of the 10 patients with bilateral EEG abnormalities in the series reported by Gupta et al. underwent hemispherectomy; 5 out of the 7 patients were completely free of seizures at follow-up (50). Six out of 27 (22%) patients with Lennox–Gastaut syndrome underwent hemispherectomy, with Engel class I archived in 5 out of the 6 patients (51).
Multilesional/Multifocal Resections and Multistage Surgeries
Following a complete presurgical evaluation, multilesional and multifocal resections are performed in patients with multiple epileptogenic lesions or multiple ictal onset zones. The medical literature covering this topic is limited because patients with multilobar surgeries are often lumped together with those requiring multifocal /multilesional surgeries. The indications for evaluation and outcomes of the surgical procedures are, therefore, difficult to determine. Another limitation is that documentation of the success of multifocal epilepsy surgery is sometimes limited to case reports.
Tuberous sclerosis (TS) is the most common etiology for a multilesional resection. Other etiologies include cortical dysplasias, postinfectious encephalitis, posttraumatic epilepsy, vascular injuries, tumors (in particular, brain metastases), postradiation epilepsy, etc. Some patients have dual pathologies that include malformations of cortical development and mesial temporal sclerosis (52,53). Multiple pathologies are reported in up to 10% of the specimens from patients with medically refractory epilepsy studied in one anatomopathology laboratory (54).
In the past, patients with multifocal ictal onset zones were considered nonsurgical candidates. Multifocal ictal onset zones were the reason for not performing resections in four out of nine children studied with subdural electrodes and reported by Pestana Knight et al. (37). One study in adult patients with epilepsy documented that resections were not performed after invasive evaluation in 10 out of 22 patients because of diffuse or multifocal ictal onset zones (52). Another study reported poorly localized epilepsy in 9 out of 17 cases in which resections were not performed after invasive monitoring (55). Currently, patients with multifocal epilepsy who were deemed ineligible for surgery on the basis of evaluations with subdural grids alone, or subdural grids in combination with a few depth electrodes, are benefitting from stereo-electroencephalographic (SEEG) evaluation (56,57). Vadera et al. reported 14 patients who failed subdural grid evaluation and received a second evaluation with SEEG. Ten of these patients had resections after SEEG placement. At 11 months, 60% of the patients were seizure free (56). SEEG offers some advantages to patients with multifocal, unilateral, or bilateral epileptogenic foci or lesions. These include the possibility of studying epileptogenicity in deep gyri, sulci, and bilateral brain structures when noninvasive or invasive studies had failed to localize the epileptogenic zone (57,58).
Some patients with multifocal or multilesional epilepsy may also benefit from multistage procedures. Implantation of electrodes is followed by resection and reimplantation of electrodes with further evaluations and resections, depending upon the patients’ characteristics (45,55,59). Multistage procedures have been performed in patients who require up to four admissions and two to three operations at each admission (55), with a relatively low complication rate (45,55,59). Staged and bilateral invasive evaluations have changed the outcomes for seizure control for patients with TS and those with lesions involving the motor cortex (60,61). Chapter 30 also discusses surgical strategy in patient with tuberous sclerosis complex.
Other Surgical Procedures
Multiple Subpial Transections
Some patients are candidates for limited brain resection as a palliative, more than a curative, treatment. Multiple subpial transection is another technique that has been used in cases with lesional or nonlesional epilepsy. The technique has been used alone or in combination with lesionectomies, lobectomies, or multilobar resections (61,62) and is discussed further in Chapter 88.
Limited Resection for Extensive Lesions
Catenoix et al. (63) studied seven patients with large multilobar lesions and seizure semiology consistent with mesiotemporal epilepsy who underwent temporal lobectomies. All patients became free of seizures after the surgery and remained so after a mean follow-up period of nearly 3 years. The researchers concluded that patients with ictal symptoms that are consistent with temporal lobe epilepsy have excellent seizure outcomes following temporal lobectomy, regardless of the size or extent of the brain lesions. This study analyzed only a limited number of patients with a very specific seizure semiology.
Seizure outcome of 75% at follow-up was also described in a series of four patients with infrasylvian multilobar polymicrogyria who underwent partial resection of the polymicrogyria (3/4 patients) combined with anterior mesial temporal resection. These patients had complex malformations that include polymicrogyria, squizencephaly, focal cortical dysplasia, and hippocampus malrotation (64).
Nonsurgical Candidates
Some patients do not receive epilepsy surgery because of the extent of the lesion, high risk for new postsurgical deficits, or the suspicion of multifocal epilepsy. Selwa et al. (65) followed patients for 4 years who were not surgical candidates. Twenty-one percent of the patients were seizure free at follow-up; others reported reduced seizure frequency. Roth et al. (55) reported on seven patients who became seizure free after invasive monitoring alone, without epilepsy surgery. Particular cycling of the epilepsy could possibly explain the findings that seizure freedom in these two different patient groups is possible in some refractory cases.
Some other cases considered not surgical candidates could benefit from palliative procedures such as corpus callosotomy or neurostimulation.
OUTCOME OF MULTILOBAR AND MULTIFOCAL EPILEPSY
There are data supporting the position that complete resection obtains the best seizure control after surgery and that incomplete resection of the lesion is a predictor of poor outcome. Seizure outcomes in patients with epilepsy due to large hemispheric or multifocal lesions who underwent small or limited resections are not well known.
Sarkis et al. (12) from the Cleveland Clinic reported 71% seizure freedom at 6 months in 63 patients who underwent multilobar epilepsy surgery. Seizure-free outcome was reduced to 52% at 5 years and 41% at 10 years after surgery. They did not study patients with extensive brain lesions who underwent limited resections. Bulacio et al. (66) (Fig. 85.2) reported a probability of a little above 0.1 of seizure freedom at 10-year follow-up for patients who underwent multilobar resection. This population included patients who had invasive evaluation only, which is not representative of current trends in pediatric epilepsy surgery in some tertiary care centers.
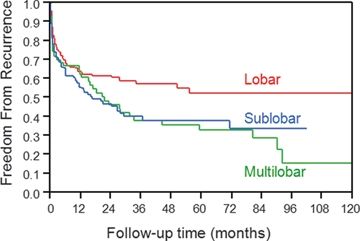
Figure 85.2. Probability of seizure freedom for the lobar, sublobar, and multilobar resections.
(Modified from Bulacio JC, Jehi L, Wong C, et al. Long-term seizure outcome after resective surgery in patients evaluated with intracranial electrodes. Epilepsia. 2012;53(10):1722–1730.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








