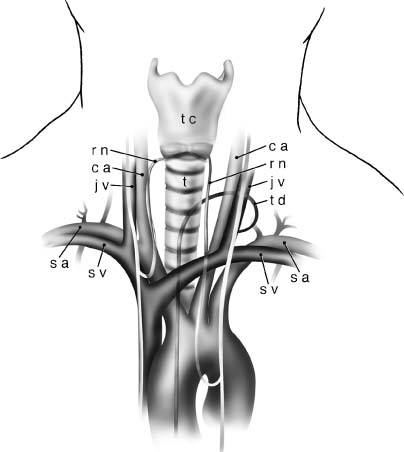
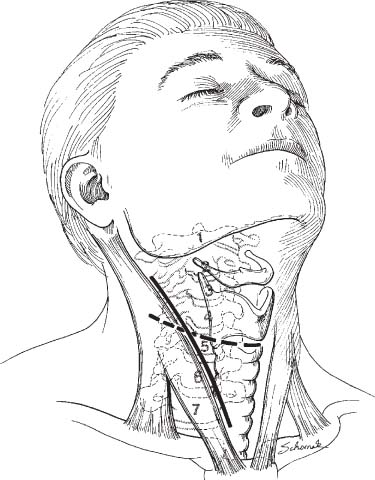
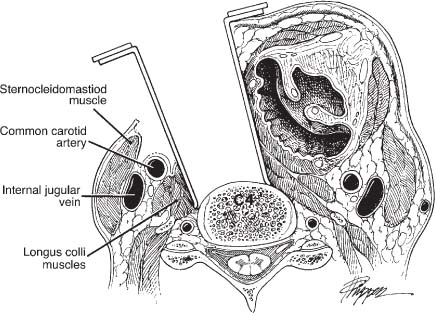
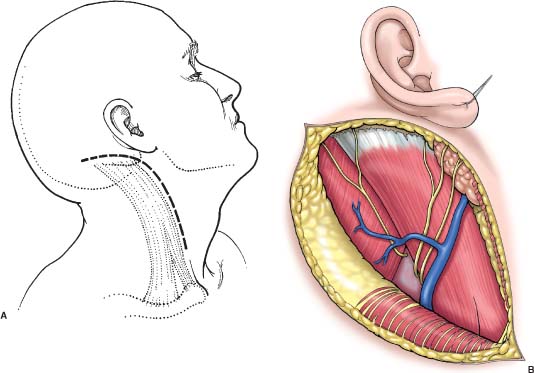
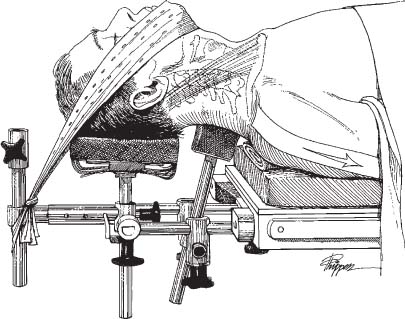
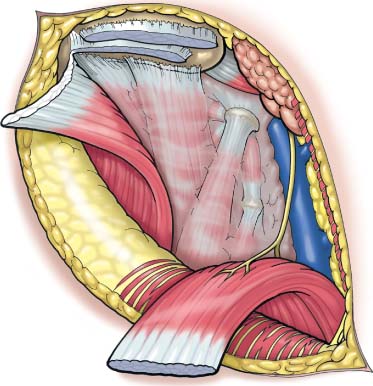
27 The pathology and location of tumors of the spine vary. Ventral lesions can cause spinal cord compression or mechanical instability. The anterior approach to the cervical spine is a well-recognized method to gain access to the ventral cervical vertebrae and spinal cord. This approach provides spinal surgeons ample exposure for tumor resection and reconstruction with internal fixation via natural fascial planes with minimal disturbance of the surrounding structures. This method, first popularized in the 1950s,1,2 was originally used to treat discogenic disease and spondylosis. With advances in imaging and instrumentation, this approach is now commonly used to treat a variety of spinal pathologies including neoplasia. The overall goals of surgery to treat spine tumors are palliation and pain relief, maintenance of stability, preservation of neurologic function, and debulking/ resection for tumor control. The use of the anterior approach is intended for the treatment of lesions located in the ventral cervical spine, for reconstruction due to mechanical instability, and for the correction of postoperative kyphosis. At our institution, a formal corpectomy is an indication for cervical plate fixation in addition to the arthrodesis. The nature of pathology encountered in the cervical spine varies and is discussed in detail elsewhere in this text. Careful preoperative planning helps to promote a successful procedure and to minimize intraoperative difficulty. Neurophysiologic monitoring, fluoroscopy or image guidance, instrumentation, and graft material should be readily available. Preoperative imaging should include computed tomography (CT), magnetic resonance imaging (MRI), and a vascular examination to study the course of the vertebral artery. Anatomic variations may preclude the placement of instrumentation. Knowledge of this anatomy can prevent catastrophic complications from occurring during resection or reconstruction (Fig. 27-1). The patient is brought to the operating room and transferred to the operating table while awake and wearing antiembolic stockings. Prophylactic antibiotics are administered ~30 minutes before the skin incision. Steroids are administered if the patient is myelopathic but should be avoided if possible because they discourage bone fusion.3 If the mass is compressing the cervical spinal cord, fiberoptic intubation may be needed. It should be performed via the orotracheal or nasotracheal route while the patient is awake. The amount of movement and trauma should be minimized. Baseline motor-evoked potentials (MEPs) and somatosensoryevoked potentials (SSEPs) can be recorded to document any abnormalities before intubation. FIGURE 27-1 Surgical anatomy relevant to an anterior cervical discectomy. Subclavian artery (sa), subclavian vein (sv), carotid artery (ca), jugular vein (jv), recurrent laryngeal nerve (rn), thoracic duct (td), trachea (t), and thyroid cartilage (tc). (Courtesy of the Barrow Neurological Institute.) After the appropriate vascular access is achieved and baseline SSEPs are established, the patient is placed supine and all bony prominences are well padded. The head is placed in the midline position and extended slightly to expose the anterior surface of the neck. If overt instability is present, the patient may be positioned in the neutral position. A halo adapter can be used if the patient is wearing an orthosis. Typically, the patient is placed in a Caspar headholder with a chin strap. An interscapular bolster, which immobilizes the head and adds posterior support, is placed to further expose the area of interest (Fig. 27-2). Fluoroscopy is used from the beginning of the procedure and is available during the entire operation. FIGURE 27-2 Patient positioning with the Caspar head-holder. The patient’s head is maintained in a neutral position by means of an elastic chin strap. The cervical spine is carefully maintained in either a neutral or minimally extended posture to re-create the cervical lordosis. Adhesive tape is run along the lateral margin of the shoulder joint and arm and affixed to the foot of the bed to assist with intraoperative fluoroscopic visualization of the distal cervical spine. The tape should not be run directly over the clavicle to avoid a pressure injury to the brachial plexus. An intrascapular roll functions to facilitate operative access by allowing the shoulders to fall below the coronal plane of the cervical spine. Both the scalp leads for evoked potential monitoring and the endotracheal tube (not shown) would be rostral in the operative field. (Courtesy of the Barrow Neurological Institute.) The operative approach is directed toward the side that is most comfortable for the surgeon. A right-handed surgeon may perform the operation from the right but must appreciate that the course of the recurrent laryngeal nerve can vary, leaving it susceptible to injury. Therefore, some surgeons may elect to operate from the left, where the recurrent laryngeal nerve may course deeper in the tracheoesophageal groove. For a reoperation, we expose the ipsilateral side to avoid the possibility of bilateral vocal cord paralysis. Operative access can be extremely challenging in these cases because postoperative scarring and radiation may distort the anatomic planes. The cervical level can be estimated using external landmarks (Fig. 27-3); however, fluoroscopy helps place the skin incision accurately. Furthermore, the rostral and caudal extremes of the surgical site can be viewed to determine the orientation of the incision. Usually, a horizontal incision in a skin crease is used for a one-level corpectomy, and a longitudinal incision along the medial border of the sternocleidomastoid is used when multiple levels must be decompressed. After the patient had been prepared and draped, the skin is incised down to the platysma muscle. Careful dissection and broad undermining of tissues allow better mobilization of the cervical structures and full surgical exposure. The sternocleidomastoid muscle is identified, and the fascial plane between the sternocleidomastoid muscle and tracheoesophageal bundle is developed. The carotid artery should be palpated so that the dissection can be directed medially. For multilevel procedures, the omohyoid muscle may need to be divided. The carotid sheath is retracted laterally with the trachea and esophagus medially (Fig. 27-4). The prevertebral fascia may be pushed away with a Kittner clamp with a small gauze sponge at the end to expose the anterior longitudinal ligament covering the ventral spine. The longus colli muscles are visible bilaterally. Fluoroscopy is then used to confirm the vertebral level. The ventral spine is cleared of soft tissues, and the longus colli muscles are dissected using electrocauterization. Radiolucent self-retaining retractors can be inserted under the longus colli in the cephalocaudal position to provide full exposure. Distraction posts may be placed at the superior and inferior vertebral bodies. Care must be exerted to avoid compromising the integrity of the vertebral body for later screw placement. FIGURE 27-3 Orientation to the vertebral column may be estimated by palpating superficial anatomic structures. The hyoid bone sits roughly at the level of the C2–3 disc space. The top of the thyroid cartilage can be estimated as the C3–4 disc space. The inferior border of the thyroid cartilage can be estimated as the C4–C5 level. The cricoid ring approximates the level of the C5–6 disc space. The C7-T1 disc space sits approximately one fingerbreadth above the clavicle. Our preference is to expose the vertebral column through a transversely oriented skin incision. Adequate extension beyond the midline or across the substance of the sternocleidomastoid muscle allows exposure comparable to that afforded by a longitudinally oriented incision along the medial border of the sternocleidomastoid muscle. Furthermore, the cosmetic result is superior. (Courtesy of the Barrow Neurological Institute.) The lateral approach described by Verbiest4 also may be useful to expose lesions that extend from the uncovertebral joint out the neural foramen as well as the vertebral artery. The superficial exposure is similar to the anterior approach; however, the carotid sheath may be retracted medially to obtain a more lateral trajectory of approach. The longus colli musculature encountered at the lateral edge also is dissected medially. Care should be taken not to injure the cervical sympathetic chain. These maneuvers provide a direct view of the uncovertebral joint and outer surface of the neural foramen. The patient is placed in a lateral position with the head turned 10 degrees toward the downturned side. The skin incision is made longitudinally down the anteriorly border of the sternocleidomastoid and hooks posterior as the base of the mastoid process and curves back along the base of the skull 6 to 8 cm (Fig. 27-5). The platysma and fascia are divided in the neck. The insertions for the sternocleidomastoid and the splenius capitis are cut, leaving a cuff for reattachment. The muscles are mobilized inferiorly, and the deep fascia is identified, as well as the course for the accessory nerve. The C1 transverse process should be palpable 1 cm below and 1 cm in front of the mastoid tip (Fig. 27-6). The deep fascia is incised from the tip of the transverse process of C1 obliquely downward and parallel to the course of the spinal accessory nerve. The attachments of the elevator scapulae and the splenius cervicis to C1 are identified and elevated, keeping in mind that the vertebral artery is underneath them (Fig. 27-7). Once the vertebral artery is identified, the muscular attachments to the lamina of C1 and C2 are taken as well as those attached to the transverse process of C2. The muscle can be cleared almost to the midline (Fig. 27-8). The bone dissection is performed with a high-speed drill. The arch of C1 and the lamina of C2 should be removed first. The dissection proceeds laterally to within a few millimeters of the transverse foramen of C2, sparing the C2–C3 facet and pedicle if the pathology is intradural and stability is to be maintained. Otherwise, the transverse foramen and pedicle can be removed to mobilize the vertebral artery, if needed (Fig. 27-9).5 FIGURE 27-4 The relative anatomy and trajectory for an anterior transcervical retropharyngeal approach to the cervical vertebral column. A plane of dissection is maintained lateral to the tracheoesophageal bundle and medial to the carotid sheath. Bilaterally, the longus colli muscles are dissected subperiosteally to provide a submuscular pocket for seating the toothed retractor blades. Failure to seat these blades beneath the longus colli muscles properly places the esophagus and adjacent vascular structures at risk for perforation. When the vertebral column is approached anterolaterally, the tendency is to direct decompression eccentric to the contralateral side. Thus, regardless of whether the operative approach is conducted from the patient’s left or right side, it is important to ensure that the ipsilateral neural foramen receives adequate attention and decompression. When anterior cervical plates are applied, the tendency is to place the plates slightly eccentric to the ipsilateral side of dissection. The plates, however, should be applied in as midline a position as possible to minimize the risk of injuring the vertebral artery and to provide as optimal a biomechanical construct as possible. (Courtesy of the Barrow Neurological Institute.) Once the level of pathology is confirmed, the decompression can be performed. Discectomies should be performed above and below the lesion. Exposure of the end plates laterally to the uncovertebral joints helps orient the surgeon to the midline. A bone rongeur or pituitary forceps can be used to remove tissue for pathology. Bleeding from vascular lesions and engorged epidural veins may be profuse. Hemostasis is achieved with the use of Gelfoam and bipolar coagulation. The decompression is continued to the posterior longitudinal ligament with the use of the operating microscope. A highspeed drill is helpful for decompression of a bony mass as well as for later preparation of the end plates for fusion (Fig. 27-10). The extent of the resection depends on the nature of the tumor. A standard corpectomy trough can be extended safely to 20 mm. If the tumor extends through the lateral and posterior elements of the vertebral segment, resection may be limited by the course of the vertebral artery. Mobilization of the vertebral artery may be necessary and is well described.6 Injury to the vertebral artery can add significant morbidity to the procedure. Primary repair is advocated but is not always feasible.7 Endovascular techniques may be helpful if this situation arises. If en bloc resection is intended, the resection may be extended laterally and require a posterior procedure. The corpectomy should be extended to the posterior longitudinal ligament, which is then resected to expose the ventral dura. Midline orientation is paramount because the tumor may have blurred the normal anatomic landmarks. Appreciation of the position of the longus colli, uncovertebral joints, and pedicles and fluoroscopy permits appropriate orientation and safe decompression. Once the decompression is completed, attention must be directed toward reconstruction. Many substrates are available for promoting fusion if that is the intended goal. In patients with highly malignant disease, only structural support may be desired. Numerous graft materials are available for use as corpectomy spacers and range from autologous bone to titanium mesh. For patients with benign disease, we prefer to use autograft iliac crest for a single-level corpectomy or for a multilevel decompression. Polymethylmethacrylate (PMMA) and titanium cages are reasonable alternatives associated with acceptable outcomes in patients with malignant tumors.8 In such cases, we prefer to use PMMA combined with a Steinmann pin. PMMA must be used carefully because the exothermic polymerization reaction leads to hardening. The supine position makes it challenging to avoid contact with the dura. A layer of Gelfoam or novel methods such as the use of chest tubes have prevented PMMA from leaking onto the surface of the thecal sac (Fig. 27-11). FIGURE 27-5 Patient positioning and incision for lateral approach to the cervical spine. (A) The patient is placed in the true lateral position. The neck is extended and the chin turned 10 degrees toward the down side. The skin incision is made along the anterior border of the sternocleidomastoid muscle, beginning ~1 cm below the level of the cricoid cartilage, and extended up to the base of the mastoid process, where it is curved back across the base of the skull for 6 to 8 cm. (B) The platysma muscle and the superficial fascia are divided in the neck, exposing the sternocleidomastoid muscle, splenius capitis muscle, greater auricular nerve, and lesser occipital nerve. (From Shucart W, Borden J. Lateral approaches to the cervical spine. In: Menezes AH, Sonntag VK, eds. Principles of Spinal Surgery. New York: McGraw-Hill, 1996:1325–1332, with permission.) Spinal instrumentation represents a bridge to allow the process of fusion to occur. Understanding this principle allows surgeons to take the necessary steps to promote fusion (Table 27-1) when performing spinal arthrodesis and reconstruction after the removal of spinal tumors. Some factors that impair fusion are often part of the treatment of spinal neoplasms. Steroids are a very effective group of medications in terms of providing neural protection, but their use has been associated with decreased rates of fusion in an animal model.3 A major modality in the treatment of cancer is radiation. Radiation has profound effects on the healing process in general and on bone healing and fusion specifically.9,10 A fibrous union may be the goal when PMMA is used in patients with a malignancy The addition of cervical plates to the arsenal of spinal surgeons has allowed successful reconstruction in the presence of complex pathology. After a ventral defect has been filled by bone graft or PMMA, the construct can be stabilized with internal fixation. The evolution of cervical plates has paralleled that of spinal surgery Many varieties of plates are available, but the goal is the same: internal fixation. We prefer the Atlantis plate because of the flexibility of using it with different screw configurations, depending on the surgical circumstance. Before a plate is placed, ventral osteophytes should be removed to create a flat contact surface. Care must be taken to avoid perforating an extensive amount of cortical bone, which can decrease the strength of the screws to resist pulling out. Fluoroscopy is used to measure the plate size in situ. If needed, a bending device can be used to achieve a lordotic curve. A set pin holds the plate in place while the holes are drilled using the appropriate drill guide under radiographic guidance. Screws are placed firmly into the vertebral body. Unicortical screws are used, so the longer a screw is, the greater will be its pullout strength. If the screw does not purchase the bone well, a larger diameter rescue screw may be helpful. The screw trajectory is also confirmed with fluoroscopy. The screw should pass into the dense bone of the vertebral body. The distal end plate should be avoided because violating it may attenuate the screw purchase (Fig. 27-12).
Surgical Approaches for Tumor Resection and Reconstruction of the Cervical Spine
 Anterior Approach (C3–C7)
Anterior Approach (C3–C7)
Operative Indications and Pathology
Preoperative Preparation and Anesthesia
Positioning and Approach
 Lateral Approach
Lateral Approach
Tumor Resection
Internal Fixation and Arthrodesis
Tenets for Optimizing Fusion
Plate Fixation
| Maneuver | Benefit |
| Insert graft under compression | Improves graft incorporation |
| Maximize surface of implantbone interface | Improves graft incorporation |
| Remove soft tissue from fusion interface | Avoids fibrous healing |
| Maintain integrity of cortical end plate | Prevents telescoping of graft |
| Irrigate while drilling | Prevents thermal injury with impaired bone healing/resorption |
| Avoid contouring plate | Avoids fatiguing of implant |
| Avoid overtightening screws | Prevents stripping screw hole and diminishing bone purchase |
| Insert angulated screws | Improves pullout strength |
| Use longest screws possible | Improves pullout strength |
From Baskin JJ, Vishteh AG, Dickman CA, et al. Techniques of anterior cervical plating. In: Operative Techniques in Neurosurgery. Philadelphia: WB Saunders, 1998:94, with permission from Elsevier.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree