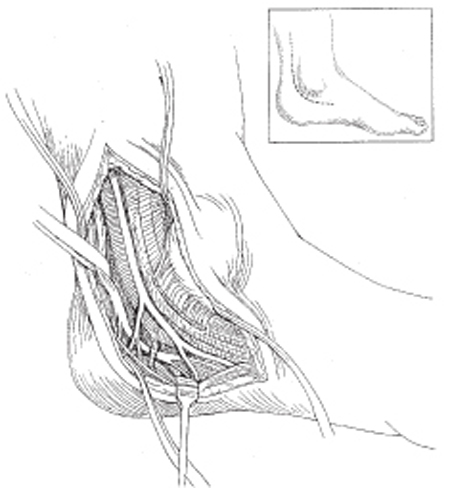
47 Tarsal Tunnel Syndrome A 44-year-old female presented with a one and a half year history of numbness and pain along the instep of her left foot. She was treated initially for plantar fasciitis with a course of nonsteroidal anti-inflammatory agents, two cortisone injections, and then an endoscopic release. Her symptoms did not improve. They were worse with weight-bearing for more than 15 minutes but were improved with lying or sitting. Examination demonstrated an area of markedly increased sensitivity on the instep of her left foot with a palpable nodular mass of dense tissue within the plantar fascia near its insertion on the calcaneus. Sensation was diminished to light touch over the bottom of the foot, the heel, and the plantar aspect of all toes. Percussion over the tibial nerve at the level of the medial malleolus caused local tenderness and reproduced the dysesthesias in the plantar aspect of the foot. Motor strength and deep tendon reflexes were normal. Range of motion in the lumbar spine and foot and ankle was normal. Electrical studies were normal. These included sensory responses of the sural, medial, and lateral plantar nerves and motor nerve conduction of the left tibial nerve, and needle electromyography of the foot intrinsics, abductor hallucis, and lumbar paraspinals. Plain films and magnetic resonance imaging showed evidence of a calcaneal spur and plantar fasciitis. No abnormalities were detected on a bone scan. Because of the patient’s persistent complaints and the distribution of her pain, she elected to undergo redo plantar fascia release and tibial nerve decompression. The plantar fascia nodule was resected. Next the tibial nerve was identified proximal to the medial malleolus and traced distally. The tarsal tunnel was released. The bifurcation of the medial and lateral plantar and a separate calcaneal branch were identified. The plantar tunnels were released and the septum between the medial and lateral plantar tunnels was resected. The tibial nerve and the major branches were neurolysed circumferentially. No focal abnormality in the tibial nerve or its branches was identified, but intraoperative nerve action potentials showed mild slowing from the tibial nerve into both the medial and lateral plantar branches. She had a good outcome at 1-year postoperative follow-up. She had a 2-hour limit on her feet but was able to resume playing tennis. On examination, there was a mild Tinel sign near the medial malleolus and slight decrement in sensibility on the lateral aspect of the foot. Mild tibial nerve irritation Plantar fasciitis Other nerve disorders must be excluded, including generalized peripheral neuropathy, spinal root compression, proximal tibial nerve or isolated calcaneal branch compression, or interdigital neuromas. Other orthopedic conditions must also be considered, including plantar fasciitis or plantar fascia rupture, or tendinitis. These conditions may coexist with tarsal tunnel syndrome, however. Foot deformity (e.g., pronation of the hindfoot) and swelling should be assessed with the patient standing. The remainder of the foot examination can be performed with the patient seated. Careful inspection and palpation of the ankle may demonstrate retromalleolar or submalleolar swelling, synovitis, or mass. The patient has tenderness in the retromalleolar region. Percussion or manual pressure over the tarsal tunnel characteristically reproduces radiating symptoms distally along the course of the nerve(s). Subjective numbness may be difficult to quantify with pin, vibratory testing, or routine two-point discrimination. Rarely, there may be subtle weakness of the foot intrinsic muscles or reduced sweating. A detailed neurological examination should be normal otherwise. The tibial nerve passes by the medial malleolus of the ankle posterior to the tendons of the posterior tibialis and toe flexors and the tibial artery deep to the flexor retinaculum, which forms the tarsal tunnel (Fig. 47–1). The tibial nerve typically bifurcates into the medial and lateral plantar nerves beneath the retinaculum or within 2 cm of the medio-malleolar-calcaneal axis; occasionally there may be a more proximal bifurcation. One of the calcaneal branches also may be given off beneath the flexor retinaculum, but the calcaneal branching pattern is quite variable. Within the tarsal tunnel, bony walls consisting of the medial calcaneus, posterior talar process, and medial malleolus of distal tibia surround the tibial nerve. In addition to compression of the tibial nerve at the level of the flexor retinaculum, the medial and lateral plantar branches may be compressed more distally beneath the deep fascia of the abductor hallucis muscle as these nerve branches pass through their own respective tunnels. Rare compression of the inferior calcaneal nerve, the first branch of the lateral plantar nerve, and the nerve to the abductor digiti minimi have also been described.
Case Presentation
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Anatomy
Anatomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


