FIGURE 49.1 Vascular territories. Gold, anterior cerebral artery (ACA); pink, middle cerebral artery (MCA); blue, posterior cerebral artery (PCA). (From http://rad.usuhs.edu/rad/stroke/index.html, accessed July 31, 2011, with permission).
Carotid Artery
Each internal carotid artery (ICA) arises in the neck as one of the terminal branches of the common carotid artery. The cervical portion of the ICA ascends the neck (cervical segment) without branches and enters the skull through the carotid canal in the petrous portion of the temporal bone, courses through the petrous bone (petrous segment), and emerges intracranially within the cavernous sinus (intracranial segment). The vessel has an S-shaped course in the sinus, referred to as the carotid siphon. Within the cavernous sinus, the ICA lies in close proximity to cranial nerves (CNs) III, IV, V1, 2, and VI. Ascending sympathetic fibers surround the artery. Involvement of these structures may occur with intracavernous carotid disease, for example, aneurysm. The menin-gohypophyseal trunk arises from the presellar or juxtasellar ICA to supply the posterior lobe of the pituitary and adjacent meninges. Immediately after exiting the sinus, the ophthalmic artery arises and then the posterior communicating artery, which connects the internal carotid and posterior cerebral arteries (PCAs), followed by the anterior choroidal artery. The ophthalmic artery gives rise to orbital, extraorbital, central retinal, anterior ciliary, and long and short posterior ciliary branches. The two carotids, their communicating branches, and the basilar artery make up the arterial circle of Willis at the base of the brain (Figures 49.2 to 49.5). The circle of Willis is subject to wide variations in configuration, with frequent anomalies. There may be hypoplasia of one or more components, which may have a string-like caliber, or duplication of vessels, absent vessels, or persistent embryonic origin of some of the constituents (Figure 49.6). The circle is normal and completely formed in only about half of individuals without evidence of nervous system disease. Anomalies occur in about 80% of patients with neural dysfunction.
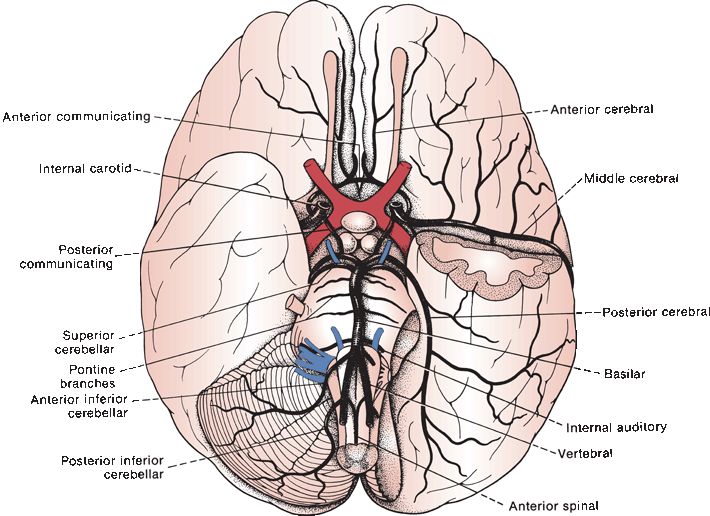
FIGURE 49.2 Base of the brain showing the major cerebral arteries and some of their branches.
FIGURE 49.3 The circle of Willis and its relationship to adjacent structures. Note innumerable perforating branches arising from every part of the circle to supply the deep midline structures. A1, horizontal segment of ACA; A2, vertical segment of ACA P1, horizontal segment of PCA; P2, ambient segment of PCA; SCA, superior cerebellar artery; OA, ophthalmic artery; ON, optic nerve; I, infundibulum; CNIII, oculomotor nerve; CN IV, trochlear nerve. (From Osborn AG. Diagnostic Cerebral Angiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)

FIGURE 49.4 Right internal carotid arteriogram performed with temporary cross compression of the left common carotid. Both ACAs (large arrows) fill via the anterior communicating artery (small arrow). (From Osborn AG. Diagnostic Cerebral Angiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
FIGURE 49.5 Lateral view of left internal carotid arteriogram showing filling of the posterior communicating (small arrows) and posterior cerebral (large arrow) arteries. (From Osborn AG. Diagnostic Cerebral Angiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
FIGURE 49.6 Variations in the circle of Willis. A. Hypoplasia of the anterior communicating artery. B. Anomalous ACAs. C. Fusion of the ACAs. D,E. Hypoplasia of branches of the internal carotid artery (ICA). F. PCA from the ICA. (Modified from Alpers BJ, Berry RG, Paddison RM. Anatomical studies of the circle of Willis in normal brain. Arch Neurol Psychiatry 1959;81:409–418.)
Branches of the posterior communicating artery enter the base of the brain between the infundibulum and the optic tract and supply the antero-medial thalamus and the walls of the third ventricle. The anterior choroidal artery arises from the ICA artery just before its termination. It passes backward along the optic tract and around the cerebral peduncle as far as the lateral geniculate body, where its main branches turn to enter the inferior horn of the lateral ventricle; it supplies the choroid plexus of the lateral ventricle. During its course, it gives branches to the optic tract, hippocampus, tail of the caudate nucleus, medial and intermediate portions of the globus pallidus, posterior two-thirds of the posterior limb of the i nternal capsule, middle third of the cerebral peduncle, and outer part of the lateral geniculate body. The retrolenticular and sublenticular portions of the internal capsule are also supplied by this artery.
The ICA terminates just lateral to the optic chiasm, near the medial side of the temporal pole and the medial and lower portion of the sylvian fissure by dividing into its major terminal branches: the anterior cerebral artery (ACA) and the middle cerebral artery (MCA). The deep, central, or lenticulostriate arteries, 2 to 12 in number, originate from the main trunk, terminal trunks, the bifurcation site, and/or leptomeningeal branches of the MCA, either separately or from common trunks. They dip perpendicularly into the brain substance to supply the basal ganglia and the genu, anterior limb, and superior part of the posterior limb of the internal capsule. They are terminal branches and do not anastomose with each other (end arteries), and occlusion produces localized infarction in the distribution of the involved vessel (lacunar infarction).
The Anterior Cerebral Artery
The ACA, normally the smaller of the two terminal ICA branches, crosses the anterior perforated space above the optic nerve and runs forward and medially to the medial longitudinal fissure; just in front of the optic chiasm, it is linked to the opposite ACA by the anterior communicating artery (Figures 49.4 and 49.7). It is divided into three segments angiographically: A1 (horizontal or precommunicating), A2 (vertical or postcommunicating), and A3 (distal and cortical branches). It then travels forward and rostrally within the interhemispheric fissure, lying on the medial surface of the hemisphere close to the corpus callosum (Figures 49.8 and 49.9). Along its course, the ACA artery gives off four primary cortical branches. The orbital or orbitofrontal artery arises proximally, where the main trunk turns upward, and spreads out over the orbital surface of the frontal lobe, supplying the olfactory lobe, gyrus rectus, and medial and inferior portions of the orbital gyri. Near the genu of the corpus callosum, the frontopolar artery arises to supply the medial surface of the prefrontal region as far forward as the frontal pole. The ACA arcs around the genu of the corpus callosum and then gives off the callosomarginal artery, which courses backward in the cingulate sulcus; it gives off the anterior internal frontal branch about the middle of the superior frontal gyrus, the middle internal frontal branch at the posterior extremity of the superior frontal gyrus, and the posterior internal frontal branch in the region of the paracentral lobule, and then continues backward to the posterior parietal region. The ACA continues as the pericallosal artery, which follows the body and posterior part of the corpus callosum to end by anastomosing with branches of the PCA.
FIGURE 49.7 Drawing of the ACAs and branches. A1, horizontal segment; A2, vertical segment; mLSAs, medial lenticulostriate arteries; RAH, recurrent artery of Heubner; ACoA, anterior communicating artery. Large arrows indicate the vascular watershed or border zone between the anterior and middle cerebral arteries. (From Osborn AG. Diagnostic Cerebral Angiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
FIGURE 49.8 Blood supply of the cerebral cortex. A. Lateral surface of the brain. B. Medial surface of the brain.
FIGURE 49.9 Lateral view of magnetic resonance angiogram, showing major arteries and venous sinuses. ICA, internal carotid artery; MCA, middle cerebral artery; PCA, posterior cerebral artery. (From Fix JD. Neuroanatomy. 4th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins, 2009, with permission.)
Numerous small branches of both the anterior cerebral and pericallosal arteries penetrate the corpus callosum. The cortical branches of the ACA supply the medial and orbital surfaces of the frontal lobe, the medial surface of the parietal lobe as far as the parietooccipital fissure, the cingulate gyrus, and the genu and anterior four fifths of the corpus callosum; these areas include the motor and somesthetic centers in the paracentral lobule. The terminal branches, like those of the PCA, wind around to supply a small portion of the lateral surface of the hemisphere, in this case, of the frontal and parietal lobes.
The largest of the deep, or central, branches of the ACA is the recurrent artery of Heubner (medial striate artery). It takes a recurrent course, and after giving a few branches to the orbital cortex, passes through the anterior perforated space to join the deep branches of the MCA. It supplies the lower part of the head of the caudate nucleus, the lower part of the frontal pole of the putamen, the frontal pole of the globus pallidus, the adjacent frontal half of the anterior limb of the internal capsule, and the anterior portions of the external capsule and lateral ventricle. The anteromedial group of central arteries arises from the anterior cerebral and anterior communicating arteries and supplies the anterior hypothalamus, including the preoptic and suprachiasmatic regions, the genu of the corpus callosum, the septum pellucidum, the anterior pillars of the fornix, and part of the anterior commissure.
The Middle Cerebral Artery
The MCA is the largest of the cerebral arteries (Figures 49.8 and 49.9). It is divided into four segments angiographically: the M1 (horizontal), M2 (insular), M3 (opercular), and M4 (cortical branches). After giving off the posterior communicating artery, it turns laterally (its M1 segment) and along this segment gives off the lenticulostriate arteries (Figures 49.10 and 49.11). These pierce the anterior perforated substance and supply all of the putamen except for its anterior pole, the upper part of the head of the caudate nucleus and all of its body, the lateral part of the globus pallidus, and the posterior part of the anterior limb, the genu, and the anterior third of the posterior limb of the internal capsule. The lenticulostriate arteries are the vessels most often involved in hypertension-induced fibrinoid necrosis, leading to either occlusion (lacunar stroke) or hemorrhage. It is not usually possible to distinguish any dominant individual branch. Charcot thought there was such a vessel, the largest of the group, which he termed the “artery of cerebral hemorrhage” because of the frequent occurrence of cerebral hemorrhage in this region.
FIGURE 49.10 Drawing of the middle cerebral artery (MCA). Segments as indicated. (1), internal carotid; (2), anterior cerebral; (3), recurrent artery of Heubner; (4), anterior temporal artery; (5), lateral lenticulostriate arteries; (6), MCA bifurcation/trifurcation; (7), genu of MCA; (8), top of the sylvian fissure. (From Osborn AG. Diagnostic Cerebral Angiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
FIGURE 49.11 AP carotid arteriogram showing the middle cerebral artery (MCA) branches. (1), M1 segment (prebifurcation); (2), M1 segment (postbifurcation); (3), MCA genu; (4), lateral lenticulostriate arteries; (5), M2 segment; (6), M3 segment; (7), M4 segment (cortical branches); (8), apex of sylvian fissure (angiographic sylvian point); (9), anterior choroidal artery. (From Osborn AG. Diagnostic Cerebral Angiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
The MCA then travels first laterally to enter the sylvian fissure and then turns up and back to course in the depths of the fissure, laterally, posteriorly, and upward, over the surface of the insula and between the frontal and temporal lobes. The MCA gives off many cortical branches that supply the lateral surface of the brain. The anterior temporal artery curves out of the sylvian fissure and runs over the temporal lobe to supply the temporal pole and the anterior third of the superior and middle temporal gyri. The orbitofrontal artery supplies the lateral part of the orbital surface of the frontal lobe, the lateral surface of the orbital gyri, and the lateral surface of the inferior frontal convolution. The prerolandic artery runs for a short distance in the central fissure and then curves over the precentral gyrus to enter the precentral fissure, supplying the lower and anterior portions of the precentral gyrus and the posterior portions of the middle and inferior frontal convolutions.
The rolandic artery runs over the opercular part of the postcentral gyrus and then enters the central sulcus; it supplies the posterior portion of the precentral gyrus and the anterior portion of the postcentral gyrus. The anterior parietal artery curves over the opercular portion of the parietal lobe and extends to the interparietal fissure, supplying the posterior border of the postcentral gyrus and the anterior parts of the other parietal convolutions. The posterior temporal artery descends from the sylvian fissure and supplies the posterior two-thirds of the superior and middle temporal convolutions. The posterior parietal (supramarginal) artery arises near the end of the sylvian fissure and supplies the supramarginal gyrus and the posterior part of the inferior parietal lobule. The MCA terminates as the angular artery, which supplies the angular gyrus and the adjoining parts of the parietal lobe.
The MCA breaks up into terminal cortical branches near the apex of the sylvian fissure. These enter the pia mater where they form a superficial plexus of anastomosing vessels; from these plexuses, smaller terminal branches enter the brain substance at right angles. These branches anastomose with branches of the anterior and PCAs that project onto the lateral surface of the hemispheres. These anastomotic branches create a collateral blood supply that can compensate to a variable extent for occlusion of a particular vessel.
Vertebrobasilar System
The PCAs are formed by the bifurcation of the basilar artery. The PCA is divided into four segments angiographically: the P1 (precommunicating or mesencephalic), P2 (ambient), P3 (quadrigeminal) and P4 (calcarine). They arch backward and laterally around the cerebral peduncle, close to the upper border of the pons, parallel to the superior cerebellar artery (SCA), and above the oculomotor nerve (Figures 49.12 and 49.13). After receiving the posterior communicating branch from the ICA, the PCA continues along the medial surface of the corresponding cerebral hemisphere, beneath the splenium of the corpus callosum, to reach the medial and inferior surfaces of the temporal lobe and the medial surface of the occipital lobe (Figure 49.8), where it divides into its four cortical branches: (a) the anterior temporal artery supplies the uncus and the anterior parts of the inferior temporal, fusiform, and hippocampal gyri, except for the temporal pole, which is supplied by the MCA; (b) the posterior temporal artery supplies the rest of the fusiform and inferior temporal gyri; (c) the calcarine artery supplies the lingual gyrus and the inferior half of the cuneus; and (d) the parietooccipital, or posterior occipital, artery supplies the upper part of the cuneus, with branches to the splenium of the corpus callosum. The cortical branches of the PCA provide blood to the medial surface of the occipital lobe, including the entire visual cortex, the medial and inferior surfaces of the temporal lobe, and the splenium of the corpus callosum. Terminal branches wind around onto the lateral surfaces of the temporal and occipital lobes and a small part of the superior parietal lobule, where they anastomose with branches of the MCA and ACA.
FIGURE 49.12 Drawing of the anatomy of the PCA and its relationship to nearby structures from above. PCA segments as indicated. (1), perforating branches; (2), posterior communicating artery; (3), basilar artery; (4), oculomotor nerve; (5), trochlear nerve; (6), posterior choroidal arteries; (7), temporal branches; calcarine (solid line) and parietooccipital (dotted line) terminal branches. (From Osborn AG. Diagnostic Cerebral Angiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)








