Diagnosis of Skeletal Dysplasia |
Cervical Problems |
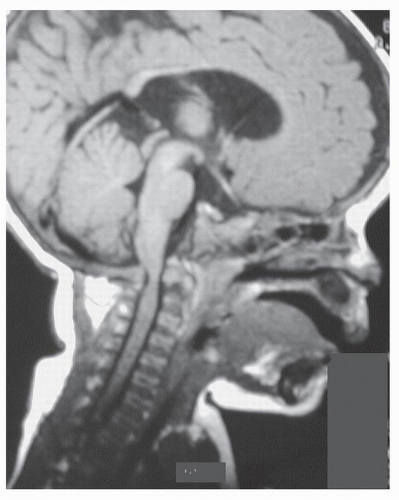
Achondroplasia |
Craniocervical stenosis (1, 2, 3, 4 and 5,7,8)
Developmental cervical subaxial stenosis (11) |
Pseudoachondroplasia |
Atlantoaxial instability due to odontoid hypoplasia and ligamentous laxity (12) |
Spondyloepiphyseal dysplasia |
Atlantoaxial instability due to odontoid hypoplasia or os odontoideum and ligamentous laxity (13,14,15,16) |
Spondylometaphyseal dysplasia |
Atlantoaxial instability due to odontoid hypoplasia and ligamentous laxity (18) |
Kniest’s dysplasia |
Atlantoaxial or occipitoatlantal instability (17, 18, 19) |
Metaphyseal chondrodysplasia |
Atlantoaxial instability due to ligamentous laxity (21,22) |
Metatropic dysplasia |
Atlantoaxial instability due to odontoid hypoplasia or lateral mass defect of C2 (23,24) |
Chondrodysplasia punctata |
Atlantoaxial instability due to os odontoideum (Conradi-Hunermann type) (22)
Subaxial canal stenosis (rhizomelic type) (25)
Coronal clefts or hypoplasia of the vertebral bodies (26) |
Diastrophic dysplasia |
Kyphosis due to hypoplasia of vertebral bodies, hypotonia, and/or spina bifida (28,29)
Atlantoaxial instability due to dysmorphism of the odontoid process(30) |
Camptomelic dysplasia |
Excessive lordosis and/or kyphosis (34,35) |
Mucopolysaccharidosis |
|
Type 1 Hurler’s syndrome |
Odontoid dysplasia (37)
Abnormal soft tissue formation around the tip of the odontoid (37,38) |
|
Type 2 Hunter’s syndrome |
Cervical canal stenosis with thickening of the soft tissue (dura) posterior to the odontoid (39,40) |
|
Type 4 Morquio’s syndrome |
Atlantoaxial instability due to odontoid hypoplasia or os odontoideum with soft tissue thickening (41, 42, 43, 44, 45, 46, 47, 48 and 49) |
Oculoauricular vertebral dysplasia |
Atlantoaxial instability due to odontoid hypoplasia
Occipital-C1 instability
Occipitalization of C1
Failure of segmentation or formation of vertebrae (50) |
Osteopathia striata |
Kyphosis due to dysplasia and hypotonia (51) |
Pyknodysostosis |
Kyphosis due to C2 and/or C3 spondylolysis (52, 53) |
Thanatophoric dysplasia |
Platyspondyly
Atlantoaxial instability due to odontoid hypoplasia (55) |
Multiple epiphyseal dysplasia |
Atlantoaxial instability due to os odontoideum (56) |
Osteopetrosis |
Spondylolysis (57)
Foramen magnum narrowing (58) |
Osteopoikilosis |
Canal stenosis (59) |
Cleidocranial dysostosis |
Basilar impression with enlarged foramen magnum (60)
Atlantoaxial instability (61) |
Spondyloepimetaphyseal dysplasia |
Atlantoaxial instability due to odontoid hypoplasia and ligamentous laxity (62) |