CHAPTER 360 The Natural History of Cerebral Aneurysms
Natural History of Unruptured Aneurysms
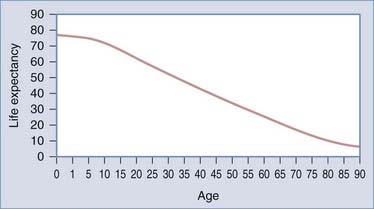
Intact or unruptured intracranial aneurysms (UIAs) are aneurysms with no recent or remote history of subarachnoid hemorrhage (SAH). Management of these patients is controversial because the natural history from the current studies is unclear.1 The treating physician must evaluate not only the aneurysm but also patient factors such as age, medical condition, and family history. Such information allows the neurosurgeon to make a calculated judgment about the lifetime risk associated with UIAs in comparison to the risk related to treatment. For example, a relatively benign natural history would favor conservative therapy (i.e., observation), particularly in the older population. In contrast, a more malignant natural history in a younger patient would make intervention more urgent. Life tables, which are based on population studies, are an estimate of life expectancy (Fig. 360-1), but an individual may vary considerably from these averages. Therefore, assessment of an individual patient’s risk involves evaluating not only the likelihood of rupture of an intact aneurysm but also the patient’s life expectancy.
Prevalence of Unruptured Aneurysms
There is considerable variation in the reported prevalence of UIAs (Table 360-1). This variation can be attributed to multiple factors, such as the nature of the study (i.e., retrospective or prospective), the mechanism and accuracy of detection (i.e., autopsy, CT, computed tomographic angiography [CTA], MRI, magnetic resonance angiography [MRA], catheter angiography), the interest and focus of the investigator (i.e., pathologist, neuropathologist, or vascular neuropathologist), and definition of a cerebral aneurysm (i.e., 1-mm versus larger expansion at a vessel bifurcation). In addition, the characteristics of the population, such as age (e.g., elderly) and nationality (i.e., Finnish and Japanese), will influence the prevalence. Lifestyle (i.e., tobacco use) and environmental factors (alcohol) may also explain variations in reported prevalence rates of UIAs. Finally, it is becoming more evident that genetic influences are involved in aneurysm formation (for further discussion, please see Chapter 362).
TABLE 360-1 Prevalence of Unruptured Aneurysms
| NO. OF PATIENTS | PREVALENCE | |
|---|---|---|
| Autopsy | ||
| Fox et al., 1983 | 164,764 | 0.8% |
| Radiology | ||
| Pre-CT era: Winn et al., 1978 | 4658 | 0.65% |
| Post-CT era: Ujie et al., 1993 | 1612 | 2.7% |
CT, computed tomography.
Rinkel and colleagues comprehensively reviewed 23 studies including more than 50,000 patients and noted a prevalence, on average, of 0.4% in retrospective autopsy studies, 3.6% in prospective autopsy studies, 3.7% in retrospective angiography studies, and 6.0% in prospective angiography studies.2 As just noted, this variation can be attributed to the nature of the population studied and the mechanisms used to document the presence of a UIA. Most of the angiographic studies analyzed by Rinkel and coworkers originated in the post-CT/MRI era, which may have skewed the prevalence of UIAs upward.2 In the post-CT/MRI era, angiography is used mainly for patients with vascular disease and therefore encompasses an older segment of the patient population. In contrast, a pre-CT (see Table 360-1) study based on angiography revealed a prevalence of 0.65%. In the pre-CT era, angiography was used more liberally; a broader segment of the population was surveyed and therefore may be more representative of the true prevalence of UIAs.
Rupture Rate of Unruptured Aneurysms
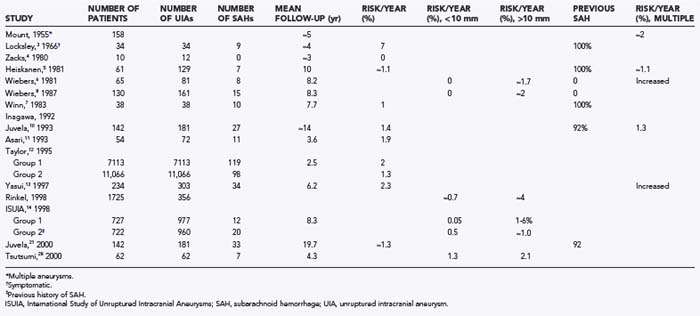
Despite intensive investigations, the incidence of SAH in patients with UIAs is not perfectly defined, as shown in the following studies (summarized in Table 360-2):
The strengths of the ISUIA include its multicenter design, which minimizes referral and treatment bias, and its size, which provides robust statistical power to formulate conclusions.14 The study has, however, been challenged on a number of points that are largely related to selection bias, the retrospective nature of the study, and the inclusion of patients with cavernous aneurysms in the study population.1,15–17 Cavernous carotid aneurysms are known to have a lower risk for hemorrhage.18 However, after excluding intracavernous aneurysms, the investigators concluded that the rate of hemorrhage was only slightly increased from 0.05% to 0.066% per year for small aneurysms and from 0.95% to 1.38% for large aneurysms.19
The most significant criticism of the study is related to the possibility of selection bias. Does the population studied truly represent a population of patients with UIA, or has some selection bias created a population with an inherently lower risk for rupture? This concern is particularly significant because selection bias cannot be corrected with any statistical methods. In regard to selection bias, all patients were selected for observation or surgery after consultation with a neurosurgeon.1,15–17,20 If it is assumed that most experienced neurosurgeons have an intuitive concept of what constitutes an aneurysm at high risk for rupture (e.g., size, configuration, family history), it is reasonable to presume that high-risk patients were treated and removed from the study pool. Removal of these high-risk patients could potentially skew the risk for rupture downward. Indeed, a calculation by Winn and associates based on the low rupture rate in the ISUIA project resulted in an extraordinary high UIA prevalence rate of 16% to 33%.1,20 This calculated prevalence rate derived from ISUIA data is several magnitudes larger than the reported prevalence rates of UIAs2 (see Table 360-1).
As with other studies, the analysis by Juvela and colleagues21 has limitations. Although the study generally lacked selection bias, the aneurysm population was derived from 30 to 50 years ago, before the introduction of imaging techniques, and it may represent a different group of patients than seen today.22 In addition, the data were compiled from a single center with the inherent single-center bias.23 A potential does exists for genetic bias because the Finnish population is known to have a higher prevalence of UIAs, a higher incidence of SAH (13 to 16 per 100,000 persons per year24,25) than in other Western countries (10/100,000 persons per year26), and a different aneurysm distribution (higher frequency of middle cerebral artery aneurysms).17,27 Most importantly, with regard to the validity of the natural history of UIAs, the study had insufficient numbers of truly incidental asymptomatic aneurysms; only 5 (4%) of the 142 patients had no previous history of SAH.21 The patients in the study by Juvela and associates21 were similar to those reported by Winn and coauthors7 in that the study involved long-term follow-up of patients with multiple aneurysm who suffered an SAH and had the offending lesion clipped, as well as similar to the patients in group 2 of the ISUIA study. All three studies reported a rate of rupture approximating 1%.
However, this study by Tsutsumi and colleagues28 must be interpreted with caution because the sample population was small and the power of the statistical analysis is therefore in question. Moreover, the follow-up period was relatively short, and the data were derived from a single center, with the associated single-center bias. The patients were obtained from a population of patients undergoing cerebral angiography who were older (mean age, 70.8 years) and had a high concomitant rate of ischemic and hemorrhagic events.
Factors Associated with Rupture
Aneurysm Size
Aneurysm size has long been considered to be an important independent variable in the risk for rupture. This was first clearly demonstrated in the study by Wiebers and coworkers in 1981, who reported a zero risk of rupture for aneurysms less than 10 mm in diameter versus an approximate 1.7% risk per year for aneurysms larger than 10 mm.6 These findings were supported in their later study reported in 1987.8 Other studies have also supported the relationship between size and rupture rate.2,7,21,28,29
Aneurysm Location
The large ISUIA study found that site was an independent variable in the incidence of SAH: basilar tip, vertebrobasilar, posterior cerebral, and posterior communicating artery aneurysms had a higher risk for rupture. The increased risk for rupture of aneurysms with a basilar artery location was also noted by Wiebers and colleagues in an earlier study.6 Rinkel and associates demonstrated that the relative risk for aneurysm rupture was higher for aneurysms located in the posterior circulation, with a relative risk of 4.1.2
In summary, UIAs located at the basilar bifurcation, and posterior communicating artery locations appear to have a higher risk for rupture than do UIAs at other sites. In contrast, as noted earlier,18 aneurysms within the cavernous sinus appear to have a lower likelihood of bleeding.
Multiple Aneurysms
For example, in 1974 Mount and Brisman reviewed 158 patients with unruptured, multiple aneurysms (which included the earlier study of Heiskanen and Marttila30) monitored for an average of 5 years and noted a bleeding rate of at least 2% per year.30 Wiebers and associates also found that multiple aneurysms had a greater propensity for rupture than did solitary aneurysms.6,8 This was consistent with the data from Winn and colleagues.7 Yasui and coworkers demonstrated an annual rupture rate of 6.8% in patients with multiple aneurysms and 1.9% in those with single UIAs.13 A meta-analysis by Rinkel and associates found that the risk for rupture was higher in patients with multiple aneurysms, with a 1.7 relative risk for rupture in patients with multiple lesions in comparison to those with an asymptomatic lesion.2 In contrast, a study conducted in Helsinki by Juvela and colleagues with 2 decades of follow-up did not confirm a higher risk for SAH in patients with multiple UIAs.10,21
Aneurysm Growth
The report by Juvela and coauthors of patients harboring a UIA had a median follow-up period of 14 years and noted that aneurysms that subsequently ruptured (17 patients) displayed a significant increase in size.10 Among the 14 patients for whom angiographic follow-up was available and in whom there was no sign of rupture, no significant increase in aneurysm size was noted. Interestingly, growth was strongly associated with cigarette smoking (odds ratio [OR], 3.48; 95% CI, 1.14 to 10.64; P < .05).10 In contrast, Sampei and coworkers observed the growth of aneurysms between successive angiographic examinations in 25 patients and noted that rebleeding did not appear to be affected by the growth rate or by the initial size of the aneurysm.31 However, 11 of the patients were monitored for only less than 1 month.
Symptomatic Aneurysms
Symptomatic aneurysms are aneurysms accompanied by signs and symptoms related to the lesion, excluding clinical features related to SAH. The symptoms may be mild, such as headaches, or more severe, such as cranial nerve palsies and brainstem signs. The studies of Locksley3 and Rinkel and colleagues2 support the existence of a relationship between symptomatic UIAs and an increased propensity for rupture. In the Cooperative Aneurysm Study, 34 patients with symptomatic, unruptured aneurysms were observed for almost 4 years (47 months), and 26% died of SAH (≈7%/yr).3 This rate was significantly higher than the rupture rate for incidental aneurysms (0.8%/yr). Rinkel and colleagues found that the relative risk for rupture of a symptomatic aneurysm was 8.2 times that of an asymptomatic lesion.2 However, in a multivariate analysis by Wiebers and associates, no correlation could be found between risk for hemorrhage and symptoms.6 This was also the case for Juvela and coworkers, who found that the percentage of patients without SAH was 65% to 80% at 20 years of follow-up, which did not differ significantly when symptomatic and nonsymptomatic (i.e., incidental) aneurysms were compared.10
Excluding headaches as a symptom, the majority of symptomatic aneurysms are associated with cranial nerve III dysfunction and are therefore most likely located at the posterior communicating location. This location has been found to have a higher rate of rupture of UIAs.14,32–34 Moreover, to affect cranial nerve III function, a UIA must enlarge. Increased size has been demonstrated to be correlated with hemorrhage. Thus, the perception that symptomatic UIAs have an increased rate of rupture may be an epiphenomenon related to aneurysm location and size.
In summary, the data are equivocal on an association between symptoms and rupture in UIAs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree