seems related, in part, to differences in methodology. Prospective follow-up studies of individuals identified at their first seizure suggest that only approximately 25% experience a second episode within the next 2 years (12,13); this contrasts considerably with the overall recurrence risk of 70% or more reported in retrospective studies (14). Also influencing the reported variation is the heterogeneous nature of clinical epilepsy. For example, when several factors were assessed in a single study, recurrence risk at 2 years varied from less than 15% in those with no identified risk factors to 100% in those with a combination of two or more risk factors (Table 9.1) (12). Although multiple factors appear to influence recurrence risk after a first unprovoked seizure, and not all studies have identified the same predictors, a meta-analysis of studies performed through 1990 suggests some consistency in predictors and in recurrence risk after controlling for these factors (15).
TABLE 9.1 SEIZURE RECURRENCE AFTER A FIRST UNPROVOKED SEIZURE: AN EXTENDED FOLLOW-UP | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
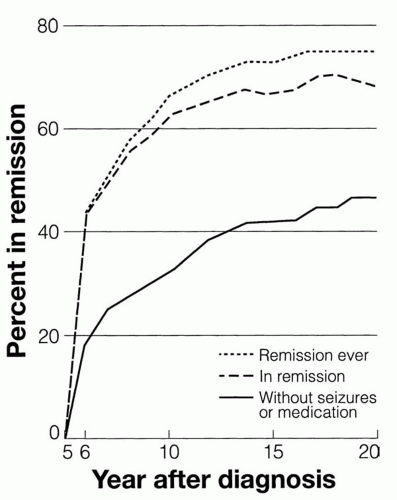
palsy), occurrence of a primary or secondarily generalized seizure, and abnormal EEG findings—particularly a generalized spike-and-wave pattern (18,26)—are linked to a reduced likelihood of remission. The number and duration of seizures prior to diagnosis are inversely proportional to the likelihood of remission (30,31). On multivariate analysis, remote symptomatic cause, family history of epilepsy, seizure frequency, and slowing on the initial EEG were independent predictors of a reduced likelihood of remission (29). In some studies, remission was less likely in children whose epilepsy began before age 1 year, but when syndrome was taken into account, early age of onset was not a factor (32,33). Numerous seizures before initiation of treatment negatively impacted chances for remission in other studies (29,30).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree