Fig. 21.1
Large extracranial trigeminal schwannoma with small middle fossa extension (type A)
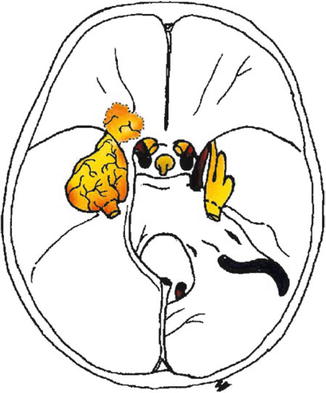
Fig. 21.2
Drawing of trigeminal schwannoma with main portion in the middle fossa and small extracranial extension (type B)
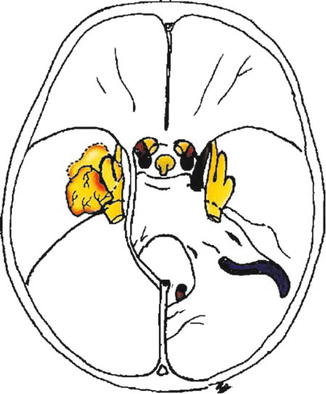
Fig. 21.3
Middle fossa trigeminal schwannoma (type C)
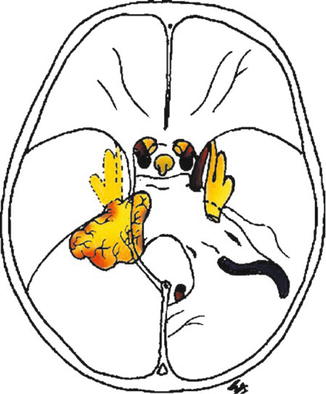
Fig. 21.4
Schematic drawing showing a posterior fossa trigeminal schwannoma (type D)
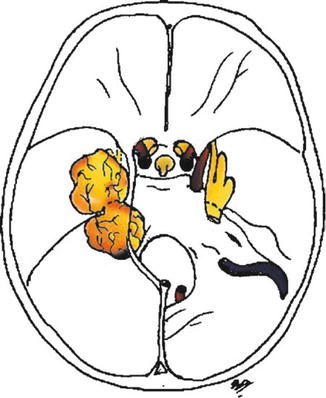
Fig. 21.5
Drawing of trigeminal schwannoma with middle and posterior fossa extensions (type E)
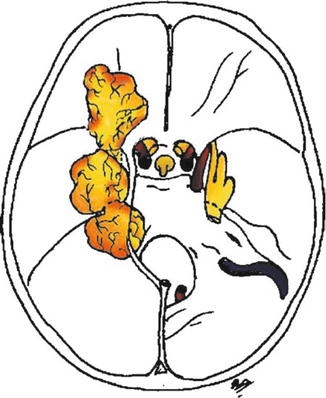
Fig. 21.6
Schematic drawing showing a trigeminal schwannoma with extracranial, middle and posterior fossa extensions (type F)
In our opinion, these modifications are important to assure the best surgical approach for each type of lesion. In the experience of the senior author (R.R.), each subgroup of this modified classification presents a different surgical challenge. Tumor types are ordered according to the level of difficulty as A, C, D, B, E, and F. The degree of difficulty in radical surgical removal depends on the particularities of each case, but according to this modified classification, Type A tumors have the lowest level of difficulty and Type F tumors, on the contrary, the highest.
21.4 Clinical Material
This series includes 21 patients who were surgically treated between 1987 and 2012 at our institution. Two patients received a diagnosis of NF2. One patient presented with a posterior communicating artery aneurysm on the same side as the TS. There were 3 Type A, 2 Type B, 8 Type C, 2 Type D, 4 Type E, and 2 Type F tumors (Table 21.1). The cavernous sinus was involved in 16 cases. The sizes of the lesions were small (<3 cm) in 5, medium (between 3 and 4 cm) in 6, large (>4 cm) in 6, and giant (> 5 cm) in 4 cases.
Table 21.1
Types of tumors and surgical approaches in 21 patients with TSs
Level of difficulty | Type of tumor | No. of patients (%) | Approach |
|---|---|---|---|
Easiest | A | 3 (14.3) | Extradural (TM or TM + EMF) |
B | 2 (9.5) | Intradural (IMF) | |
C | 8 (38.2) | IMF or EMF | |
D | 2 (9.5) | Retrosigmoid | |
E | 4 (19) | Presigmoid or 2-staged retrosigmoid/middle fossa | |
Hardest | F | 2 (9.5) | Combination of all of the above |
The clinical symptoms in these patients included trigeminal hypesthesia (10 patients), facial pain (9 patients), headaches (6 patients), hearing impairment (3 patients), seizures (3 patients), diplopia (4 patients), ataxia (2 patients), exophthalmos (1 patient), and hemiparesis and increased ICP with papilledema (1 patient) (Table 21.2). Prior to 1990, postoperative CT imaging studies confirmed the extent of resection. After 1990 all patients underwent pre- and postoperative CT and MR imaging studies. In our series, postoperative imaging examinations were routinely performed 3 days after surgery. Postoperatively, imaging examinations are performed every 6 months for 2 years, then once a year for 5 years, and after that every 2 years. Recurrence was defined as a new lesion identified on routine MR imaging in a patient considered to have had total resection. Progression was related to tumor growth in a patient considered to have had subtotal or partial resection, as demonstrated by immediate postoperative MR imaging. Total tumor excision was possible in 20 patients, whereas total removal was not achieved in 1 patient with NF2 due to adherences within the cavernous sinus. There were no surgery-related deaths (Table 21.3). Nine patients developed postoperative anesthesia in at least one branch of the trigeminal nerve. Trigeminal motor function was preserved in 8 patients. Two individuals developed a CSF leak and were successfully treated by lumbar CSF drainage. Only 1 of the 9 patients who reported facial pain preoperatively remained symptomatic postoperatively. Two patients exhibited minimal facial palsy that resolved during the follow-up period. The patient with preoperative hemiparesis showed progressive improvement after surgery. There were two recurrences: one in a patient with NF2, which occurred 5 years after a radical removal of a Type C tumor, and one in a patient with a Type A tumor 6 years after a radical resection. In this patient recurrence occurred in other portion of the trigeminal nerve (tumor Type C). In both cases, the recurrent tumor was removed, with an uneventful postoperative outcome.
Table 21.2
Preoperative clinical symptoms in 21 patients with TSs
Symptom | No. of patients (%) |
|---|---|
Trigeminal hypesthesia | 10 (47.6) |
Facial pain | 9 (42.9) |
Headache | 6 (28.6) |
Diplopia | 4 (19) |
Seizure | 3 (14.3) |
Hearing symptoms | 3 (14.3) |
Ataxia | 2 (9.5) |
Exophthalmos | 1 (4.8) |
Hemiparesis and increased ICP with papilledema | 1 (4.8) |
Table 21.3
Results of surgical procedures in 21 patients with TSs
Op outcomes | No. of patients (%) |
|---|---|
Total resection | 20 (95.2) |
Near-total resection | 1a (4.8) |
Recurrence | 2 (9.5) |
Op-related death | 0 |
21.5 Surgical Approaches
According to the aforementioned classification (Table 21.1), Type A tumors are resected via a transmaxillary (Fig. 21.7) approach (TM) or TM associated with an extradural middle fossa approach (EMF) if there is broad extension to the middle fossa. Type B lesions are removed through an intradural middle fossa approach (IMF); large extradural extensions, however, may require a transmaxillary exposure (Fig. 21.8). Type C tumors are extirpated via a middle fossa approach, either intradurally or extradurally (Figs. 21.9 and 21.10). Resection of Type D tumors is best achieved via the retrosigmoid approach. Tumors Type E are extirpated using a presigmoid approach or 2-staged retrosigmoid and middle fossa approaches [4] (Figs. 21.11 and 21.12). As stated before, Type F tumors are considered the most challenging lesions and may demand a combination of all previously described approaches (Fig. 21.13).
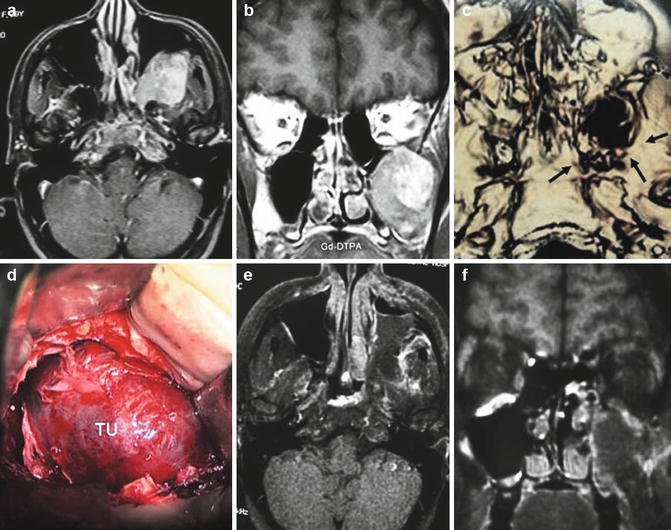
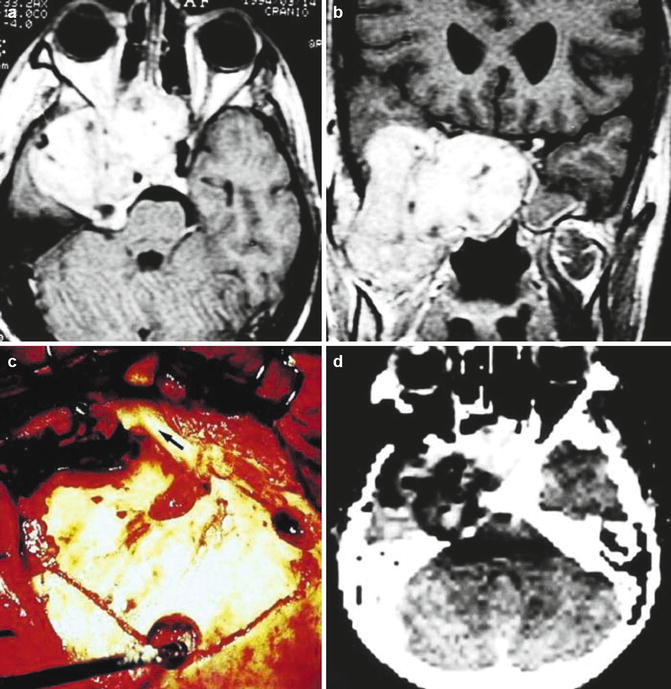
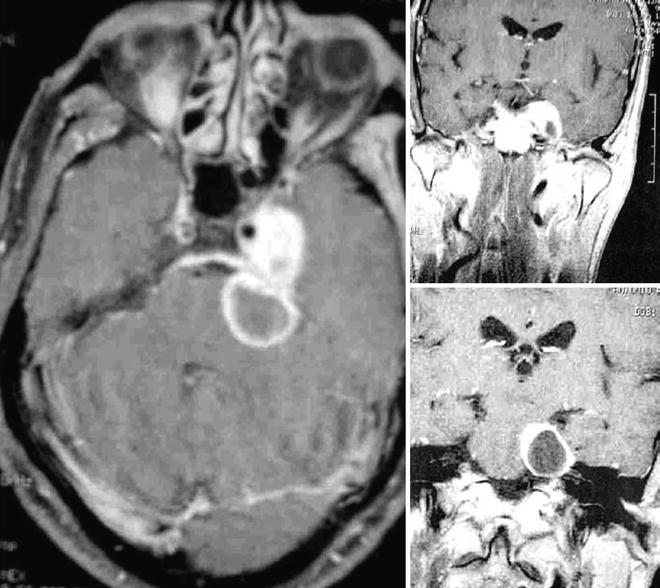
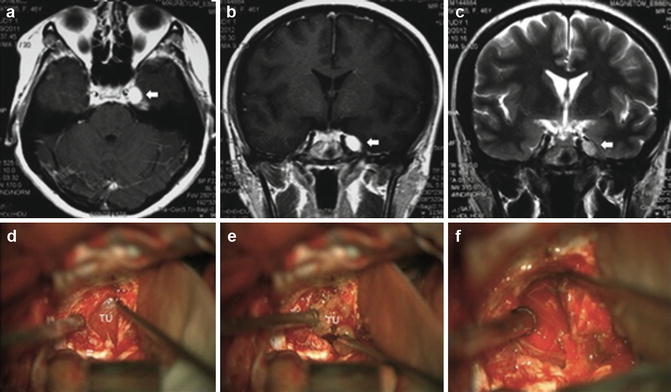
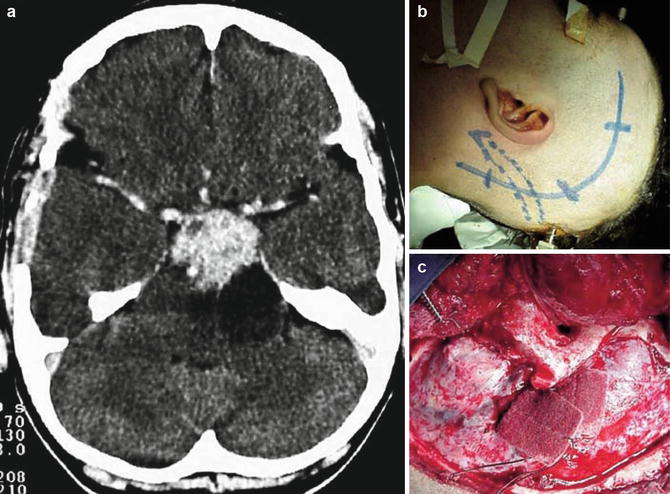
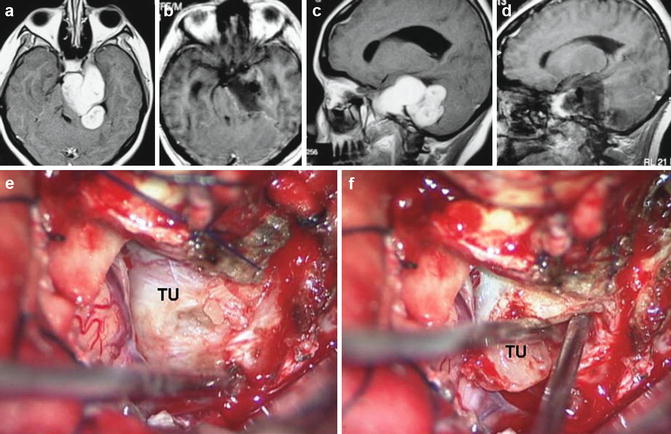
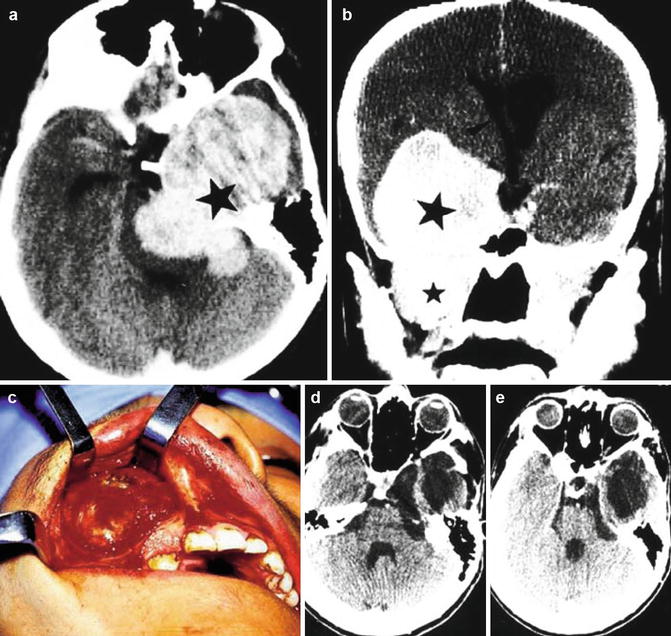
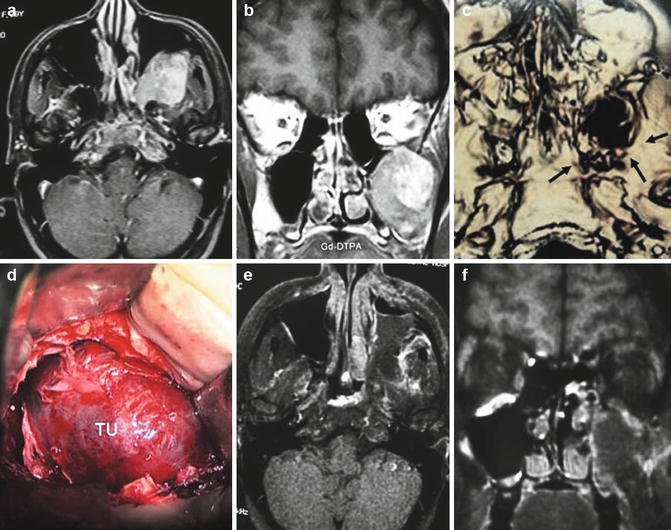
Fig. 21.7
(a, b) Magnetic resonance imaging (MRI) scan of a large trigeminal schwannoma with main portion in the maxillary sinus (type A). Gd-DPTA Gadopentetate. (c) Computed tomography (CT) scan showing enlargement of the foramen rotundum (arrows). (d) Surgical picture: transmaxillary approach exposing the tumor (TU). (e, f) Postoperative MRI
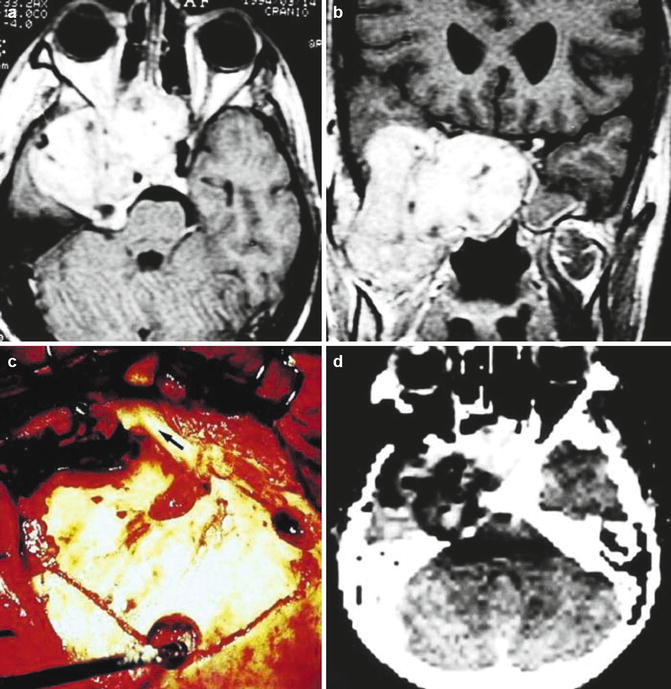
Fig. 21.8
(a, b) MRI of a large trigeminal schwannoma with middle fossa and extracranial extension (type B). (c) Middle fossa craniotomy. Zygomatic arch (arrow). (d) Postoperative CT scan
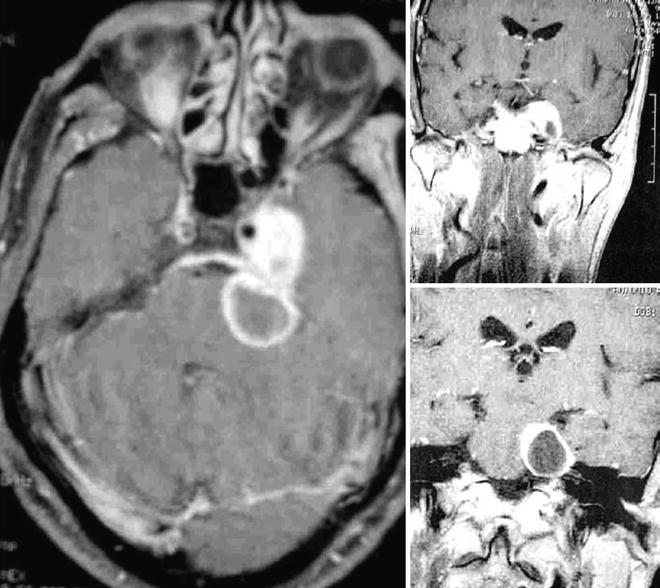
Fig. 21.9
MRI studies showing middle fossa trigeminal schwannoma with cystic posterior fossa portion (type C)
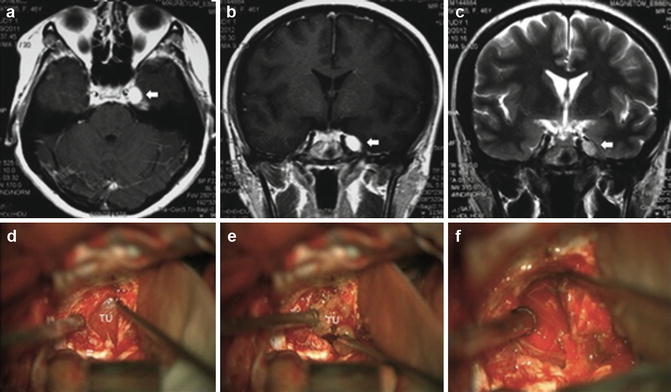
Fig. 21.10
Axial (a) and coronal (b, c) MR imaging study of a Type C TS with cavernous sinus involvement (arrows). (d) Intraoperative photograph showing tumor exposure (TU) in a middle fossa intradural approach. The lateral wall of cavernous sinus was opened. (e) Intraoperative photograph showing dissection of the tumor capsule (TU) and preservation of trigeminal fibers after total removal (f)
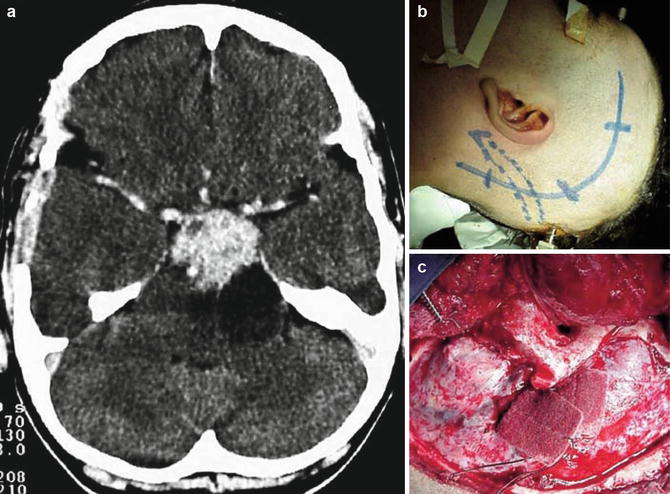
Fig. 21.11
(a) Preoperative MRI showing a posterior fossa trigeminal schwannoma (type D) with cystic portion. (b) Skin incision. (c) Presigmoid craniotomy
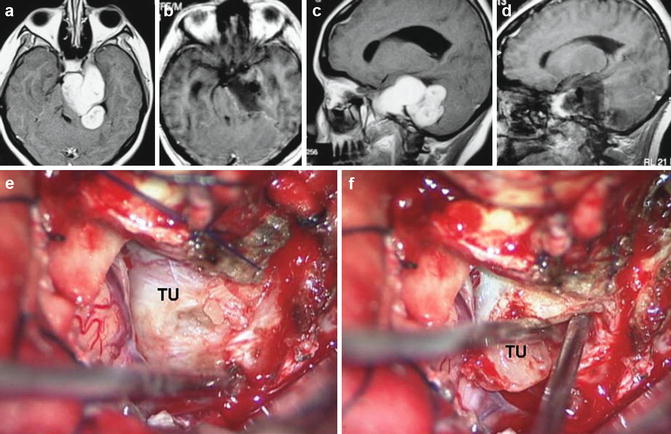
Fig. 21.12
Pre- (a, c) and postoperative (b, d) MRI scans of a large trigeminal schwannoma (type E) with extension within the middle and posterior fossa. (e) Surgical picture of presigmoid approach for removal of the tumor. (f) Removal of the tumor capsule from the brainstem
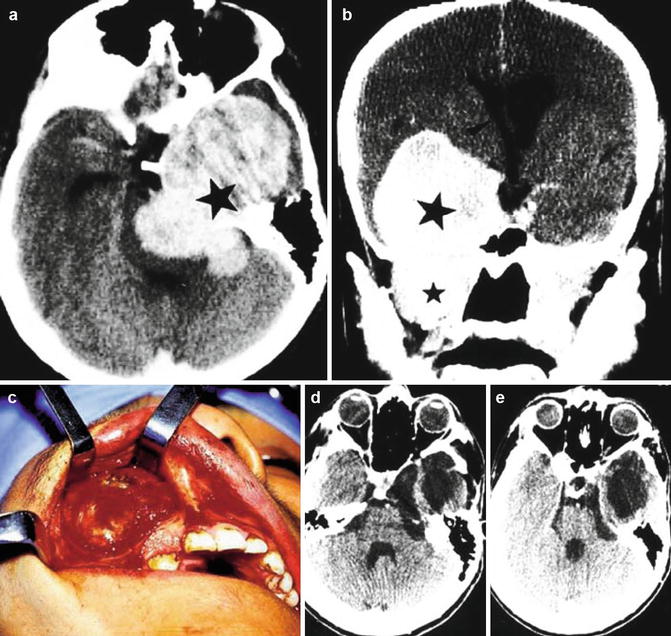
Fig. 21.13
CT scan of a large trigeminal schwannoma (type F) with extensions in the posterior fossa, middle fossa and maxillary sinus (a, b; stars). (c) Transmaxillary tumor exposure. (d, e) Postoperative CT scans
21.5.1 The Transmaxillary Approach (Caldwell-Luc Procedure)
This procedure is usually performed in association with the middle fossa approach to remove large TSs. In our series, it was used to remove a large schwannoma within the maxillary sinus with small extension to the middle fossa and the cavernous sinus. After induction of general anesthesia, the gingiva is infiltrated with lidocaine 1.0 % with 1:100,000 epinephrine solution. A 3-cm incision is made over the upper canine and the upper first premolar tooth. To improve the suturing, 1 cm of gingival tissue is left intact above the dentition. The soft tissue and periosteum are elevated from the anterior wall of the maxilla. The infraorbital nerve is identified as it exits the infraorbital foramen (midpupillary line). The anterior wall of the maxillary sinus is opened. The tumor is identified and microsurgical intracapsular debulking is performed. Total removal of the maxillary, middle fossa, and cavernous sinus portions is accomplished with this approach. The incision is closed with 4–0 absorbable sutures.
21.5.2 The Middle Fossa Zygomatic Approach
The patient is placed supine with the head fixed in a 3-pin device and rotated ~30° to the opposite side. A C-shaped skin incision over the pterion is performed. The temporalis muscle fascia is incised to protect the frontal branch of the facial nerve, and the scalp-fascia flap is lifted anteriorly. The temporalis muscle is retracted inferiorly and posteriorly. A pterional craniotomy is performed and enlarged to the base of the temporal fossa by removing bone with a rongeur to obtain a flat viewing angle across the floor of the middle fossa. The dura mater is then dissected and elevated from the middle fossa, exposing the superior orbital fissure. The middle meningeal artery is coagulated and transected. The second and third branches of the trigeminal nerve are identified. The foramen ovale and rotundum are exposed using a drill. The dura mater is elevated from the lateral cavernous sinus wall, revealing the tumor extradurally and the branches of the trigeminal nerve. The tumor is debulked and its capsule is dissected from the intact branches of the trigeminal nerve, which allows radical removal of the lesion. The tumor may be approached intradurally by opening the Sylvian fissure and exposing the optic nerve, the internal carotid artery, and the third cranial nerve. The lateral cavernous sinus wall is exposed via a temporopolar approach, and the tumor is removed. The trigeminal fibers are preserved as much as possible. The petrous apex is drilled, and the petroclinoidal ligament is cut to expose the posterior fossa portion, allowing complete excision of the remaining tumor. Neuronavigation can provide valuable intraoperative information during tumor debulking as the location of vascular structures is distorted by the tumor [7].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








