ETIOLOGY
Congenital muscular torticollis was first described by Hippocrates over 2,000 years ago (
2). Alexander the Great was believed to have congenital muscular torticollis and its associated facial deformities (
3). In 1643, Minnius was the first to attempt surgical treatment of this condition (
4). Anderson (
5) gave a more detailed description of this deformity in an article in 1893, and in that same year Warren published the first case report of surgical release in the United States (
2).
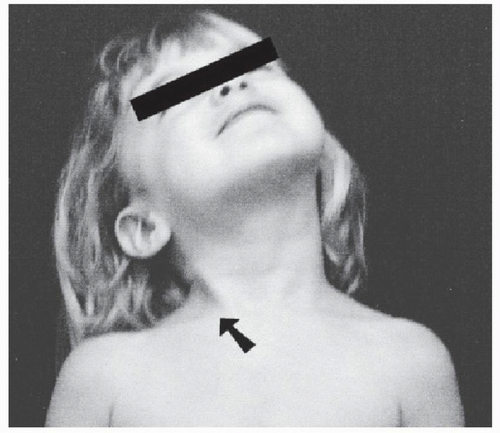
The deformity is caused by a contracture of the sternocleidomastoid muscle that results in tilting of the head to the involved side and rotation of the head and neck away from the involved muscle (
Fig. 36.1). The family usually consults a physician because of the cosmetic deformity. Often, a child has a misshapen skull or plagiocephaly, and the torticollis is unnoticed until it is brought to the parents’ attention.
The reported incidence of congenital muscular torticollis varies from 0.084% to 2.1% (
6,
7 and
8). The exact etiology is unknown, but there are several theories. Volkman in 1885 believed that torticollis was the result of an intrauterine infection that resulted in myositis and fibrosis of the sternocleidomastoid muscle. This theory is probably of historical interest only, because no evidence of underlying infection has been found on histologic examination of the sternocleidomastoid muscle, and there have been no reports of isolating an infecting organism in patients with muscular torticollis.
Stromeyer described a birth trauma theory in which the sternocleidomastoid muscle is torn during a difficult labor and delivery, resulting in bleeding, hematoma formation, fibrosis, and contracture (
2,
3,
9). Although this has been a popular theory, it is not supported by histologic studies, which have failed to show evidence of acute bleeding, hematoma formation, or chronic blood breakdown products (
3). Also, this theory does not explain the occurrence of congenital muscular torticollis in patients delivered by cesarean section (
10).
Tang et al. (
11) proposed a cellular cause for torticollis. They found myoblasts and fibroblasts in varying stages of differentiation and degeneration in sternocleidomastoid pseudotumors. The source of these myoblasts and fibroblasts are unknown. However, after birth, environmental changes stimulate the cells to differentiate and a sternocleidomastoid tumor develops. The occurrence of torticollis depends on the fate of the myoblasts. If the myoblasts continue normal development and differentiation, no persistent torticollis will occur. If the myoblasts begin degeneration, the remaining fibroblasts produce large amounts of collagen, producing a scar-like contraction of the sternocleidomastoid muscle and the torticollis persists (
10,
11).
Genetic causes or predisposition for congenital muscular torticollis also have been suggested (
12,
13). Thompson et al. (
12) reported congenital muscular torticollis in five related females (three of the five were sisters). Although genetics may have some role in the etiology of this condition, reports of a positive family history are rare.
A primary neurogenic theory is supported by findings of progressive denervation and reinnervation on histopathologic specimens of an involved sternocleidomastoid muscle (
14). Initial trauma may cause a primary myopathy that unequally involves the two heads of the sternocleidomastoid muscle. With continuing fibrosis of the sternal head, the branch of the spinal accessory nerve to the clavicular head of the muscle can become trapped, leading to a progressive deformity (
10,
14).
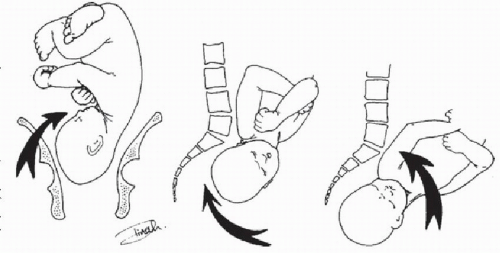
Probably the most popular theory is one of a compartment syndrome of the sternocleidomastoid muscle
caused by compression of the neck at the time of birth and delivery. This is supported by surgical histopathology sections that suggest venous occlusion of the sternocleidomastoid muscle, which may lead to localized ischemia of the muscle and result in edema, degeneration of muscle fibers, and muscle fibrosis (
15). Davids et al. (
3), using cadaver dissections, demonstrated a definite muscle compartment for the sternocleidomastoid. This compartment was defined by the external investing fascia of the neck, a substantial structure that completely envelops the sternocleidomastoid muscle. The compartment was further documented by radiopaque injection studies (
3). Manipulation of the head and neck into a position of forward flexion, lateral bending, and lateral rotation caused the ipsilateral sternocleidomastoid muscle to kink in its midsubstance similar to what occurs as a child passes through the birth canal (
Fig. 36.2) (
3). Davids et al. (
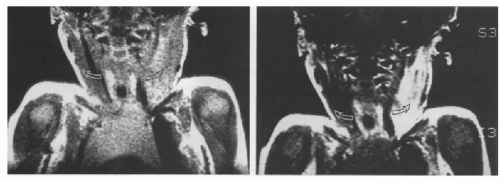
3) also obtained magnetic resonance imaging studies on 10 infants with muscular torticollis that showed signal changes similar to those seen in compartment syndromes of the muscles of the forearm or leg (
Fig. 36.3). This mechanism of localized kinking of the sternocleidomastoid muscle can lead to ischemia, reperfusion, and neurologic injuries to the muscle similar to those that occur in compartment syndrome elsewhere. Although this theory is the most attractive etiology for congenital muscular torticollis, it does not explain why children who are born by cesarean section develop this deformity or why there is a familial tendency (
10,
12,
16,
17).
All of the theories have some merit, but the compartment syndrome theory appears to be the most plausible. This theory is further supported by the association of torticollis with primiparous birth, breech positioning, hip dysplasia, metatarsus adductus, and clubfeet (
17,
18,
19 and
20). These point to a primary “packing” problem that would make a compartment syndrome the most likely “culprit.”
CLINICAL PRESENTATION
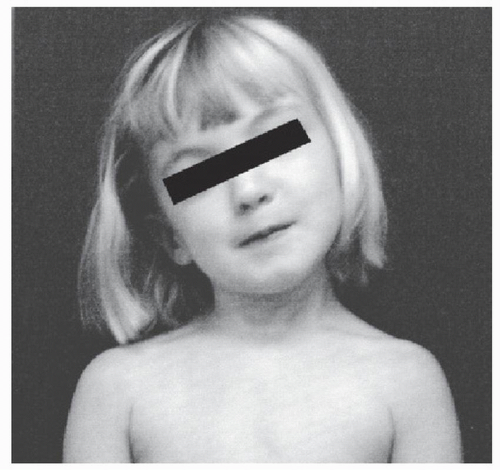
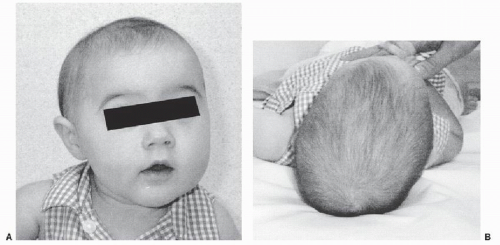
The clinical presentation of congenital muscular torticollis can be variable. Often, patients have only a mild deformity with a simple head tilt and slight rotation and minimal restriction of neck motion. In others, the deformity is severe with marked restriction of neck motion and associated deformity of the skull and facial bones or plagiocephaly (
Fig. 36.4). The torticollis usually is detected in the first 2 months of life. A mass or “tumor” may be palpable in the neck during the first 2 to 6 weeks of life. MacDonald (
17) reported this tumor in 50 (33%) of 152 patients, while Coventry and Harris (
21) reported that a sternocleidomastoid tumor was found in only 20% of patients with torticollis.
If an infant with congenital muscular torticollis sleeps prone, the affected side is the down side, which leads to asymmetric pressure on the growing cranium, causing progressive deformity of the skull and facial bones. Recession of the ipsilateral zygoma and forehead and reduction of vertical facial height may occur (
22). If an infant sleeps supine,
then molding occurs on the contralateral side of the skull, which is known as plagiocephaly. In older children, a thick fibrous band often can be palpated along the sternocleidomastoid muscle (
Fig. 36.5). The level of the eyes and ears over time may become unequal, and apparent elevation of the ipsilateral shoulder may occur. Patients with congenital muscular torticollis have an increased incidence of associated musculoskeletal disorders such as metatarsus adductus, developmental hip dysplasia, and talipes equinovarus (
3,
19,
20 and
21). The rate of associated hip dysplasia has been quoted to be as high as 20%, but more recent studies have reported the incidence to be about 8% (
18,
19 and
20,
23).
CLASSIFICATION
Congenital muscular torticollis can be classified into three clinical groups.
1. Sternomastoid tumor (patients with a clinically palpable sternomastoid tumor)
2. Muscular torticollis (patients with clinical thickening and tightness of the sternocleidomastoid muscle)
3. Postural torticollis (patients with postural head tilt and clinical features of torticollis but without tightness or tumor of the sternocleidomastoid muscle) (
26)
The severity of the torticollis can be graded based on the decreased passive range of rotation of the neck on the side of the torticollis compared with that on the normal side. In grade I torticollis range of motion is symmetrical, in grade II the motion deficit is 1 to 15 degrees, in grade
III it is 15 to 30 degrees, and in grade IV it is more than 30 degrees (
26,
27 and
28).