Fig. 44.1
(a, b) Anatomical facet replacement (ACADIA™)
44.2 Indication and Surgical Technique
Indications for facet replacement are painful degenerated vertebral joints. Spinal stenosis, namely, lateral recess and foraminal stenosis caused by hypertrophic and deformed facets, is another good indication. Degenerative segmental spondylolisthesis, which is not uncommon in destructive spondylarthrosis (Fig. 44.2), is no contraindication. As segmental motion preservation or restoration is the underlying idea of this procedure, some remaining disk function is required. Therefore, severe discopathy with collapsed disk space is a contraindication. Until today, we do not know what degree of disk degeneration can be tolerated. For our study, we have postulated a minimum of 5 mm disk height and the absence of bridging osteophytes. We also have assessed the preoperative segmental motion by flexion-extension x-rays for postoperative comparison.
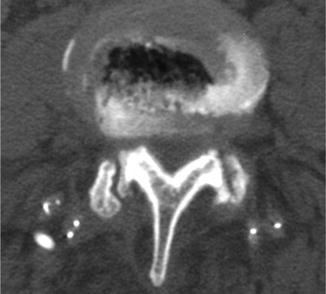
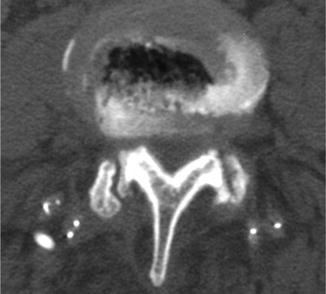
Fig. 44.2
Erosion and sagittalization of superior facet with resulting subluxation
Preoperative radiological work-up included a-p, lateral and flexion-extension x-rays. Lumbar MRI (Fig. 44.3) and thin-slice CT were performed. CT-guided facet blocks have been employed to identify facets as pain generators. Bone mineral density (BMD) has been used to exclude osteoporotic conditions. Preoperative computerized planning for optimal screw positioning was done with a CT-based semi-robotic navigation system (SpineAssist™, Mazor Robotics).
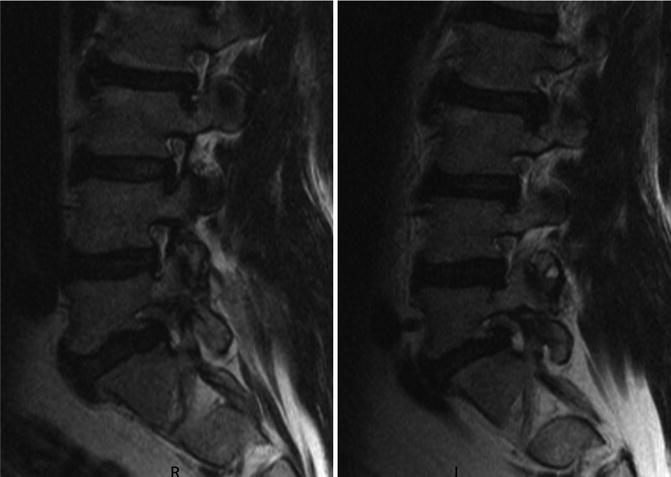
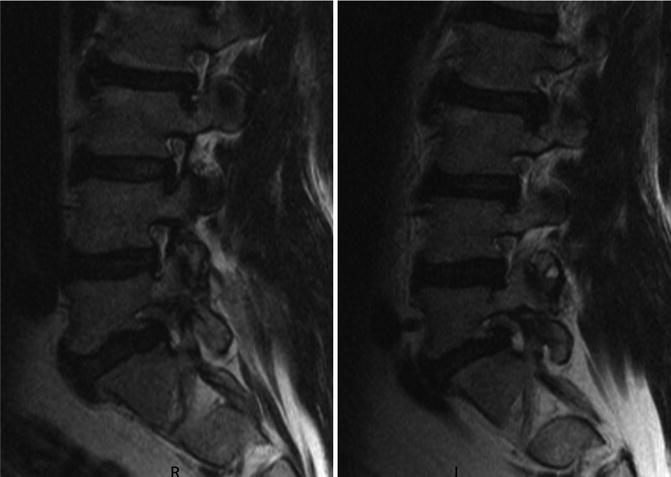
Fig. 44.3
Pat. No. 3: Foraminal stenosis with bilateral L5 nerve root compression
Surgery was performed in general anesthesia without muscle relaxation. Patients were positioned prone on a special radiolucent frame and lumbar spine in neutral position. Intraoperative biplanar and 3-D C-arm fluoroscopy were employed.
Skin incisions were placed according to preoperative planning bilaterally exactly according to the navigated plane for screw insertion. After incision of subcutaneous tissue and fascia, blunt dissection of muscles is done until the target facets are reached. In order to avoid anatomical alterations interfering with the navigation plan, with assistance of the semi-robotic system, all four screws are placed with K-wire guidance. Then the lower and upper articulate processes are completely removed on both sides, using chisels and/or high-speed drills.
At this time, exposed nerve roots and thecal sac have been freed from compressing ligaments and bony spurs. With the screws in place, the other device components were mounted. First, the hydroxyapatite (HA)-coated bases for the upper facets (UF) of the lower vertebra (e.g., L5) were anchored over the lower screws bilaterally. Then the bases for the lower facets (LF) of the upper vertebra (e.g., L4) were implanted into the bone. At this moment, it is important to avoid violation of the adjacent facet joint of the upper vertebra. Now the assembled artificial joints, the UF and LF together, were attached and fixed to the bases. During this procedure, the metal facets were strongly fixed together by an insertion tool in neutral position. For an optimal individual fit, there are implants of various sizes and designs available. The insertion tool is removed, and then a transverse connecting cross-link is fixed for further stabilization. The bilateral wounds were closed, usually leaving drains for 24–48 h.
Postoperative mobilization is encouraged the same day or day after surgery; we impose no restrictions as far as sitting, standing, or walking is concerned. We advise, however, against lifting or carrying loads for 3 months. Physiotherapy is started the day after surgery; most patients undergo postoperative physiotherapy at specialized centers for another 4–6 weeks after discharge from hospital.
Postoperatively, clinical examination was performed, and a-p, lateral and flexion-extension x-rays were done for radiological evaluation (Figs. 44.4 and 44.5). In selected cases, a postoperative CT scan was done (Fig. 44.6).
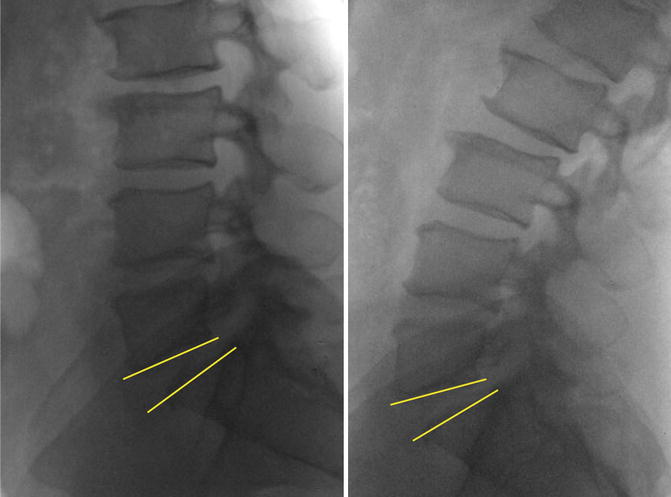
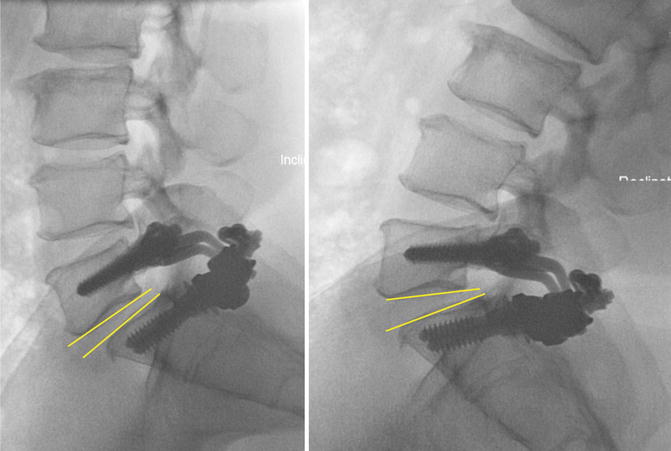
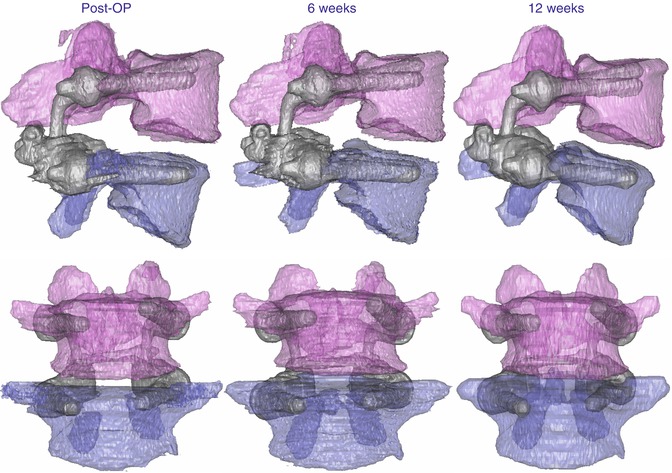
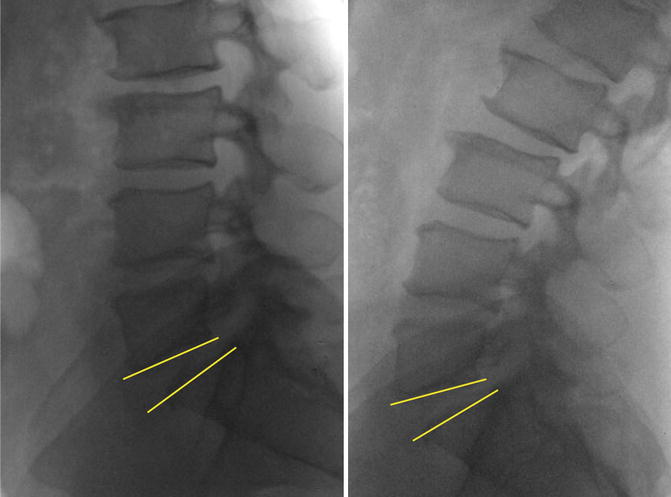
Fig. 44.4
Pat. No. 3: Preoperative flexion-extension x-rays. Yellow lines illustrate the range of motion
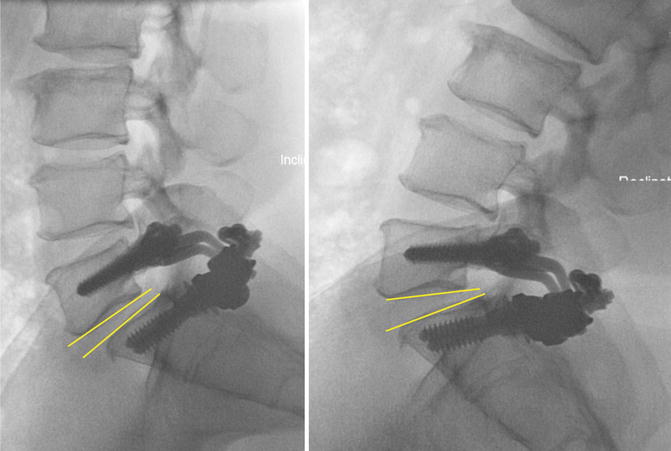
Fig. 44.5
Pat. No. 3: Flexion-extension x-rays at 24-month follow-up. Yellow lines illustrate the range of motion
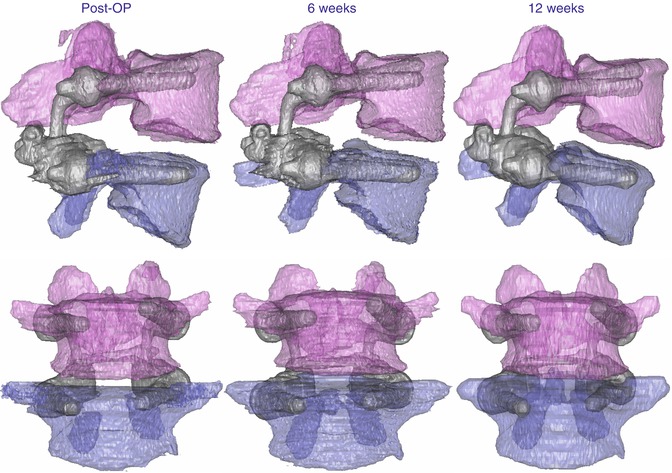
Fig. 44.6
Patient data: CT reconstruction immediate post-op and at 6- and 12-week follow-up
Follow-up examinations have been scheduled 6 weeks and 3, 6, 12, and 24 months postoperatively. A final examination (N = 4) or telephone follow-up (N = 6) was done 3 (N = 3) or 4 (N = 7) years after surgery.
44.3 Results
Between December 2008 and April 2010, 10 patients with symptomatic severely degenerated facet joints have been operated on. Indications were as follows: spinal stenosis with degenerative spondylolisthesis 8, foraminal stenosis due to spondylolisthesis 1, and arthrogenic spinal stenosis 1. Mean age was 62 years (49–76). Implanted levels were L4/L5: 7, L3/L4: 2, and L5/S1: 1. Mean duration of surgery was 159 min (106–215), and mean blood loss 580 ml (300–1,000). Mean duration of hospital stay was 6 days (5–8). Mean preoperative ODI (Fig.44.7) was 56.5 % (34–64 %), and at 3- or 4-year follow-up 1,3 % (0–4 %). Mean preoperative VAS back pain (Fig. 44.8) was 60 (5–85), at 3-year follow-up 5 (0–15), and at 4 years 3 (0–15). Mean preoperative VAS leg pain (affected side, Fig. 44.9) was 78 (44–96), at 2-year follow-up 3 (0–15), and at 3 and 4 years 0. Mean preoperative VAS contralateral leg pain was 28 (2–69), at 2-year follow-up 3 (0–15), and at 3 and 4 years 0. Mean Zurich claudication score (ZCQ) for symptom severity (best score 1, worst 4,7, Fig. 44.10) dropped from 3,21 preoperatively to 1,24 at 36 and 48 months. Mean ZCQ for physical function (range 1–4, Fig. 44.11) dropped from 2,72 to 1,00 at 3 and 4 years. Mean ZCQ for patient satisfaction (best score 1, worst 4, Fig. 44.12) at 3 years postoperatively was 1,00 and at 4 years 1,18. Patient satisfaction score was 98,1 % (87,5–100 %). There have been no surgical complications, in particular any implant-related complications.
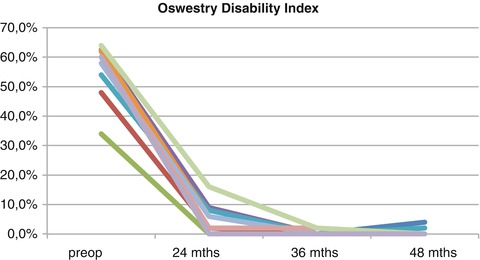
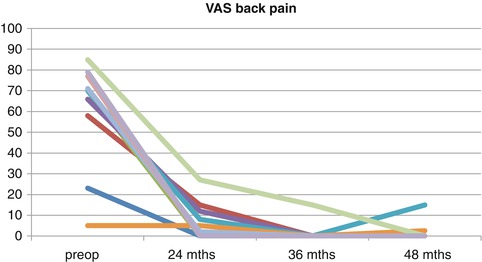
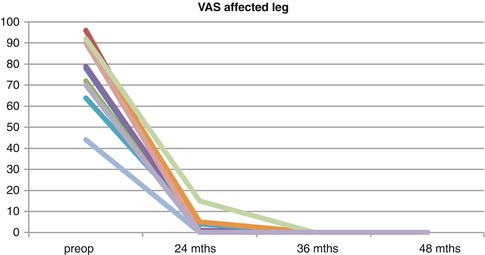
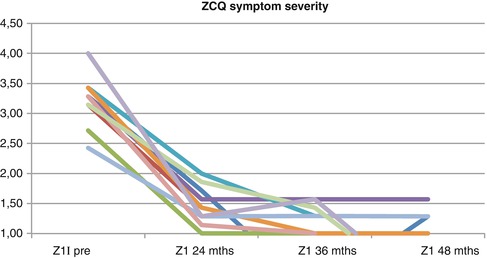
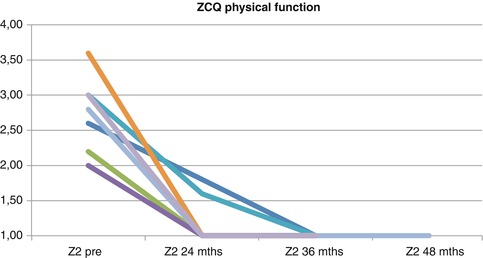
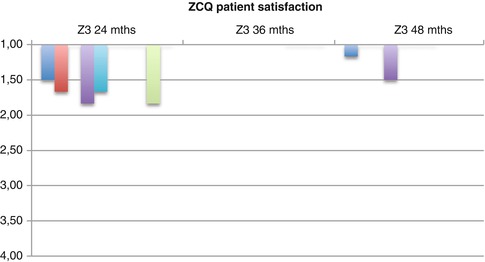
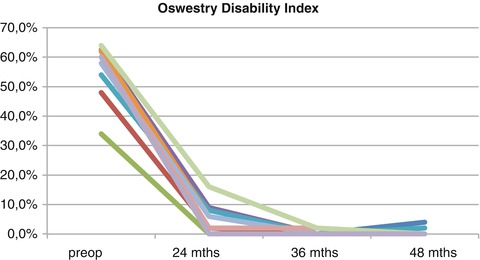
Fig. 44.7
Oswestry Disability Index after 36 and 48 months
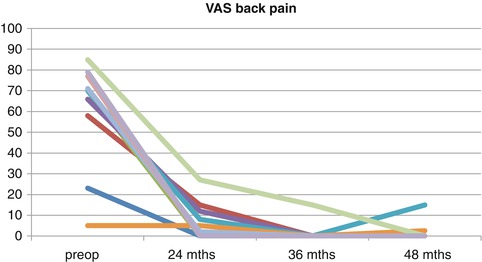
Fig. 44.8
VAS back pain after 36 and 48 months
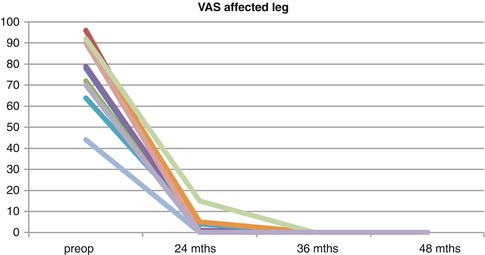
Fig. 44.9
VAS pain of the affected leg after 36 and 48 months
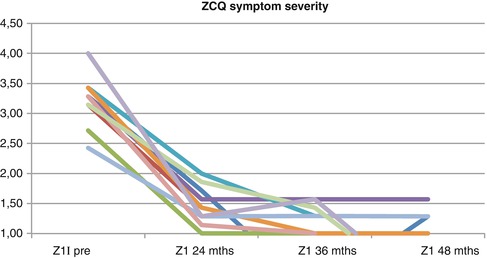
Fig. 44.10
Zurich Claudication Questionnaire 1 (range 1–4,7) at 36 and 48 months
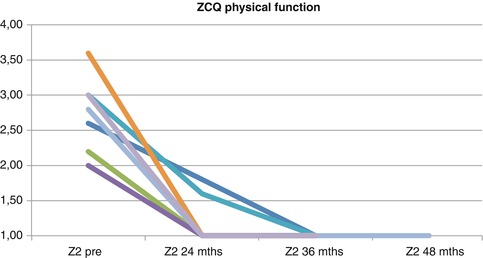
Fig. 44.11
Zurich Claudication Questionnaire 2 (best 1, worst 4) at 36 and 48 months
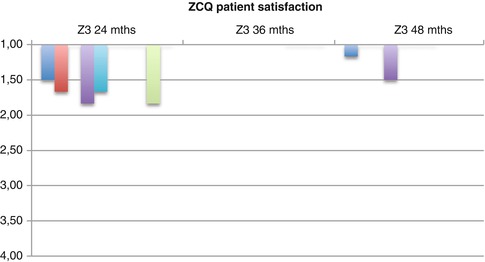
Fig. 44.12
Zurich Claudication Questionnaire 3 (best 1, worst 4) at 36 and 48 months
44.4 Discussion
Facet degeneration is a leading cause of discomfort, pain, neurogenic dysfunction, and spine motion impairment. It limits locomotion and mobility not only in the elderly but also in younger persons, but regularly compromises life quality with increasing age. Motion, particularly after a resting period or during physical work, generates pain or functional deficits such as sensory disturbances or muscle weakness. In the past, surgical treatment consisted mainly in segmental immobilization by spondylodesis (fusion), performed in various techniques [18, 24]. Decompressive surgeries alone provide satisfying effects mainly on neurogenic dysfunction and neurogenic (radicular) pain [32]. Load- and motion-dependent back pain, however, usually is insufficiently addressed by decompressive measures alone. Fusion, on the other hand, may bring about improvement, but not complete relief of complaints in many and no improvement at all in some patients [3, 7, 19]. In addition, inevitable biomechanical side effects such as load shift may induce negative consequences in adjacent segments [2, 14, 16, 20]. In order to preserve or restore motion in surgically treated spine segments, various techniques have been developed. Motion preservation by total disk replacements has undergone some disillusion over the years [11]. Especially major facet pathologies have shown adverse effects on disk replacement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








