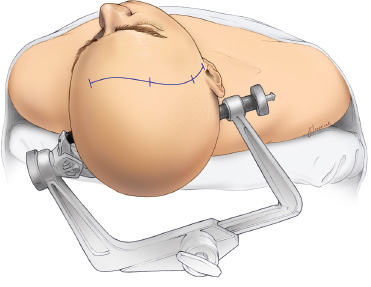
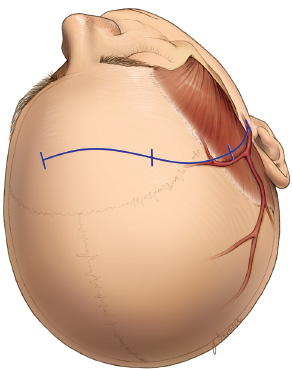
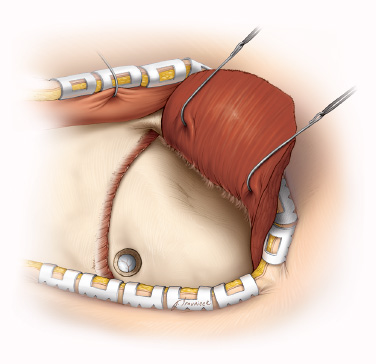
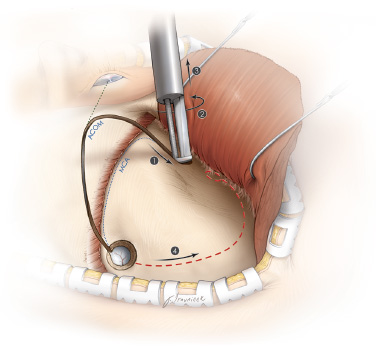
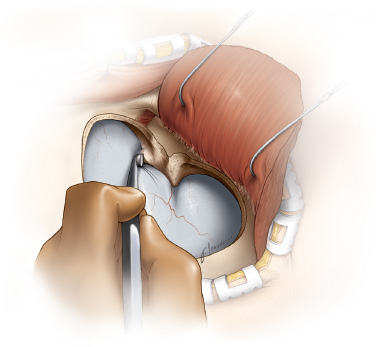
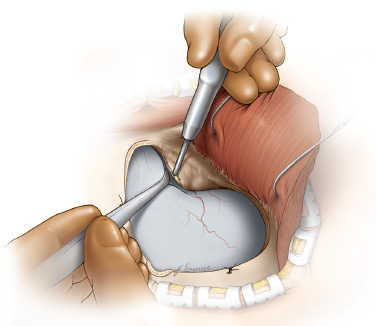
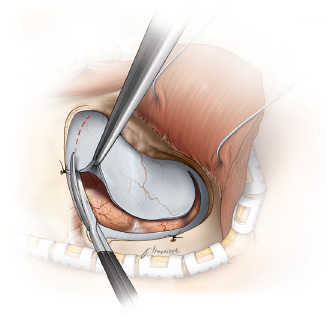
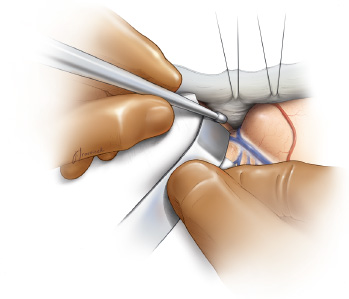
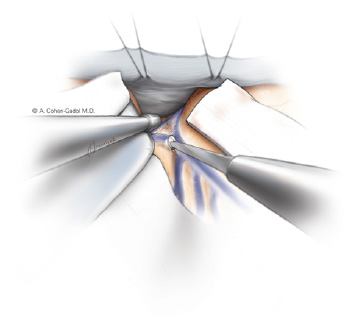
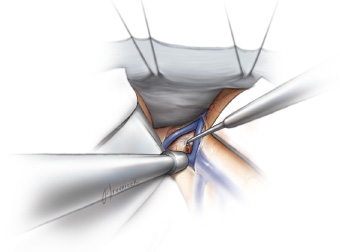
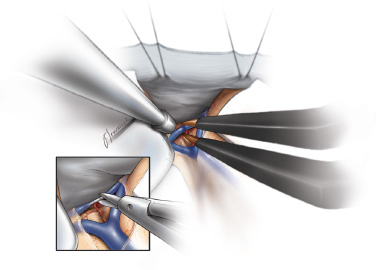
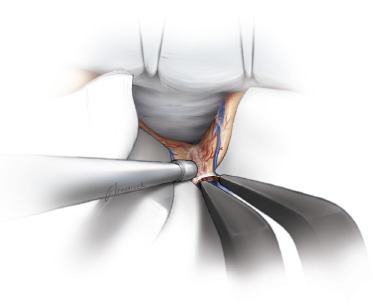
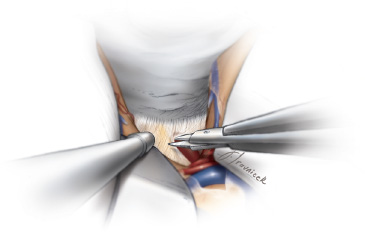
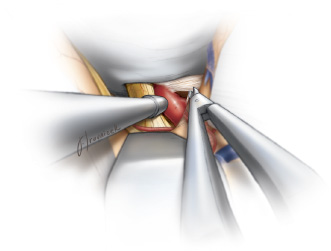
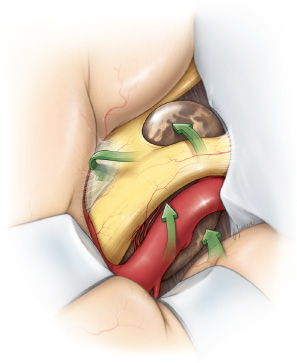
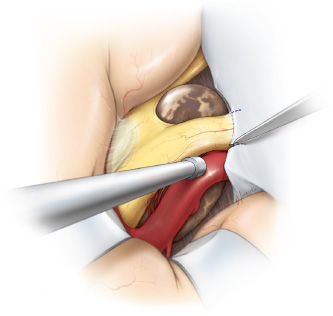
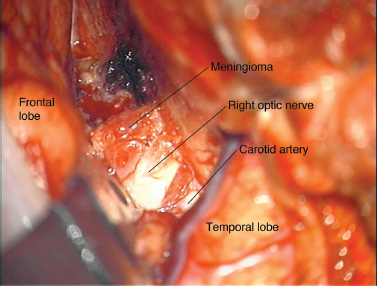
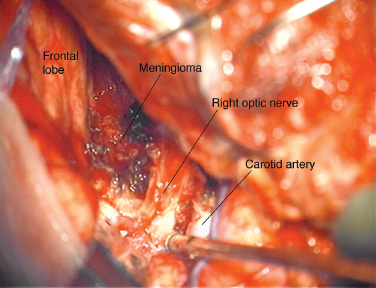
12 Transcranial Approaches to the Sellar and Parasellar Area The differential diagnosis of a mass within the parasellar space is vast. Common lesions include neoplastic extra-axial masses such as pituitary adenomas, craniopharyngio-mas, and meningiomas, or rarely vascular lesions such as an aneurysm. An intra-axial tumor such as an astrocytoma may also be found in this region. Other lesions may be encountered, including Rathke cleft cyst, arachnoid cyst, germinoma, lymphoma, metastasis, abscess, sarcoidosis, histiocytosis, hypophysitis, infundibuloma, and neurocysticercosis, to name a few.1 An in-depth understanding and familiarity with various transcranial approaches is necessary for neurosurgeons who are willing to tackle lesions within the parasellar region. Although the transsphenoidal route is the preferred route for most patients with a pituitary adenoma, ~1 to 4% of pituitary tumors require surgical resection via a transcranial route.2,3 Pituitary adenomas with a large suprasellar extension may be inaccessible through a purely transsphenoidal-transsellar route. Parasellar lesions extending into the cavernous sinus and dumbbell-shaped sellar lesions with a narrow neck across the diaphragma sellae may be approached through a transcranial route. Other contraindications to the transsphenoidal approach include active sinus infection, lesions that coexist with an adjacent aneurysm, and ectatic “kissing” carotid arteries or fibrous tumors with suprasellar extension. Some neurosurgeons have considered the uncertainty regarding the pathology of these lesions (ie, meningioma vs. adenoma) to be an indication for the transcranial route.4 The most often cited reason for using the transcranial approach is a previously failed transsphenoidal exploration, which commonly results from a combination of the above-listed reasons. In addition, a lack of descent of the suprasellar component of a large pituitary macroadenoma after a transsphenoidal resection may lead the clinician to consider a transcranial approach from above. As a general rule, parasellar lesions that do not enlarge the sella, such as meningiomas and craniopharyngiomas, typically require a greater field of view than that provided through the transsphenoidal route and may be best approached through a transcranial corridor to ensure gross total resection with preservation of neighboring neurovascular structures. Transcranial approaches provide a more panoramic view of critical neurovascular structures such as the carotid artery and optic nerves early in the dissection process, further protecting them from unsafe surgical manipulations. Conversely, transcranial approaches may pose increased surgical risks associated with a craniotomy, including frontal lobe injury due to retraction. When an approach to the sellar and parasellar regions is considered, the benefits of each approach should be carefully weighed against its inherent risks. When the neurosurgeon decides on a particular transcranial approach, he or she must take into account the specific features of the neuroanatomy of the lesion, including its size, location, relationship to the critical neurovascular structures, and predicted pathology. Before the incision is made for any of the approaches listed below, the patient is given an intravenous dose of an antibiotic (continued for 24 hours postoperatively) and an anticonvulsant (continued for 7 days postoperatively, unless a seizure disorder develops). The arterial PCO2 is maintained at ~30 mm Hg throughout the case. The patient is also given 10 mg of dexamethasone and 1 g of mannitol per kilogram intravenously at the time of the incision. A lumbar drain or external ventricular drain is generally not required. However, an external ventricular drain may be placed when the patient has hydrocephalus or when peritumoral edema is significant enough to cause intracranial hypertension. For all approaches, the head is held in position via a 3-pin Mayfield head holder or another fixation device. The head is positioned above the heart to encourage venous drainage, turned 20 to 30 degrees contralaterally, and slightly extended to keep the zygomatic arch as the highest point in the surgical field (Fig. 12.1). A minimal amount of hair is shaved, and the planned skin incision is infiltrated with lidocaine-epinephrine solution. The pterional craniotomy has been one of the workhorse approaches in neurosurgery for many years. Yasargil et al refined and described the intricacies of this approach.5 Fig. 12.1 For all approaches, the head is held in position via a three-pin Mayfield head holder. The head is positioned above the heart to encourage venous drainage, turned 20 to 30 degrees contralaterally, and slightly extended to keep the zygomatic arch as the highest point in the surgical field. Although commonly used for anterior circulation aneurysms, the pterional craniotomy also provides an excellent working corridor for resection of suprasellar and parasellar tumors. Of the transcranial approaches, it commonly affords one of the shortest operating distances to the lesion.6 This approach displays familiar anatomy, provides efficient access to the sellar and parasellar regions, and is easily mastered. The senior author (ACG) most commonly uses this approach among the other transcranial routes for reaching parasellar lesions. Once the decision has been made to use the pterional approach, laterality must be addressed. If the tumor extends significantly to one side, the tumor should be approached from that side. When lateral extension is not an issue, the approach is from the same side as the eye with the poorer vision. If the patient’s vision is symmetrically affected, the approach is from the side of the nondominant hemisphere. A small area of hair is shaved along a standard pterional skin incision. The incision is begun at the zygomatic arch, 1 cm anterior to the tragus to avoid the superficial temporal artery, and is continued 1 to 2 cm behind the hairline to the contralateral midpupillary line (Fig. 12.2). When reflecting the skin flap forward, the neurosurgeon should keep the plane of dissection below the plane of the superficial fat pad that rests above the temporal muscle and fascia. The frontal branch of the facial nerve travels through the superficial fascia of the fat pad and should be protected. The temporalis muscle is elevated from the bone with Bovie electrocautery and reflected with the scalp flap anteriorly in one musculocutaneous layer (Fig. 12.3). A burr hole is placed just inferior to the posterior aspect of the superior temporal line, abutting the skin incision, and a standard pterional craniotomy flap is elevated and extended just lateral to the midpupillary line (Fig. 12.4). If the frontal sinus is violated, it is exenterated by thoroughly stripping its mucosa away to avoid formation of a mucocele, and the sinus ostium is plugged with pieces of temporalis muscle to avoid postoperative cerebrospinal fluid (CSF) rhinorrhea. To maximize exposure and minimize frontal lobe retraction, the lateral aspect of the sphenoid ridge is drilled away as far as the superior orbital fissure. Furthermore, the edge of frontal bone over the lateral aspect of the roof of the orbit is drilled flush with the roof of the orbit by using a high-speed drill (Figs. 12.5 and 12.6). A Leksell rongeur is then used to remove additional temporal bone to expose the floor of the middle cranial fossa. The dura is incised with a C-shaped durotomy (Fig. 12.7), reflected anteriorly, and tacked up with stitches to the galea of the retracted scalp flap. With an operating microscope, a retractor blade is gently placed subfrontally just anterior to the sphenoid ridge and lateral to the olfactory tract (Fig. 12.8). The olfactory tract is followed posteriorly until the arachnoid over the optic nerve and the internal carotid artery cisterns are identified. CSF can then be drained by opening these cisterns to further increase brain relaxation. When a large tumor completely fills these cisterns, preoperative placement of a lumbar drain or intraoperative placement of an external ventricular drain should be done through a frontal burr hole to increase brain relaxation and decrease the need for frontal lobe retraction for tumor exposure. Retraction of the frontal and temporal lobes can be facilitated by opening the anterior limb of the sylvian fissure (Fig. 12.9). This maneuver will aid in reducing the retraction forces needed to obtain tumor exposure. The arachnoid of the sylvian fissure is dissected in a superficial to deep manner along its anterior limb (Figs. 12.10 and 12.11). The opening of the arachnoid nearest the lesion is of key importance for optimal exposure7 (Fig. 12.12). The arachnoid is dissected by using a blunt fine-tip probe to separate the arachnoid from the entangled vessels and then sharply cut. Microscissors can be used to continue to open the arachnoid. Bleeding can generally be controlled with irrigation; however, the small bridging veins along the anterior limb of the sylvian fissure can be taken with little ill effect. The sylvian arteries should be preserved with their corresponding lobe as much as possible. The extent to which the fissure is split depends on and is tailored to the size of the lesion to be resected. The thicker arachnoid layers over the carotid artery and optic nerve are sharply cut (Figs. 12.13 and 12.14). Fig. 12.3 The temporalis muscle is elevated from the bone with Bovie electrocautery and reflected with the scalp flap anteriorly in one musculocutaneous layer. Fig. 12.7 The dura is incised by using a C-shaped durotomy. At this point, the neurosurgeon can work in several different corridors to access and resect the tumor, including the opticocarotid, prechiasmatic, and retrocarotid windows (Fig. 12.15). The lamina terminalis provides access to the third ventricular component of the lesion when necessary. Initially, only the ipsilateral optic nerve may be in view, but as tumor resection proceeds, identification of the contralateral carotid artery and optic nerve early in the dissection process is imperative to prevent their injury. Opening the falciform ligament will partly release the optic nerve and allow safer mobilization of the nerve to manipulate the tumor (Fig. 12.16). Tumor resection should begin with devascularization (especially for meningiomas) and as much intracapsular debulking as possible and then careful dissection of the tumor capsule away from the critical surrounding tissues (Figs. 12.17, 12.18, 12.19, and 12.20). Further details concerning the treatment of individual pathologies can be found in Chapters 6 through 10. The major disadvantage of the pterional approach becomes apparent in cases in which the optic chiasm is prefixed, allowing a very limited working channel. In addition, resection may become more difficult if the lesion extends far superiorly or posteriorly because of limited exposure through this basal frontal route. Complications associated with the pterional approach include infection, hematoma, CSF leakage, postoperative seizures, and frontal lobe edema from excessive retraction. Optic nerve damage may occur during surgery as a result of aggressive tumor resection or bipolar cauterization of the nearby perforating vessels. The perforating arteries supplying the optic apparatus arise from the anterior communicating artery and from underneath the chiasm and should be preserved. Hypothalamic and/or pituitary damage can also occur as the result of manipulation of these structures or their vascular supply. Pituitary dysfunction may manifest postoperatively as diabetes insipidus and should be treated accordingly. Fig. 12.10 The arachnoid of the sylvian fissure is dissected in a superficial to deep manner along its anterior limb. Fig. 12.11 Bridging veins are coagulated and cut. Fig. 12.13 The thicker arachnoid layers over the carotid artery and optic nerve are sharply cut. Fig. 12.14 Further arachnoid opening is completed. Fig. 12.16 Opening the falciform ligament will partly release the optic nerve and allow safer mobilization of the nerve to manipulate the tumor. Fig. 12.19 Further tumor debulking is completed. Fig. 12.20 Dissection around the posterior part of the tumor reveals the contralateral optic nerve at the level of the chiasm. The orbitozygomatic (OZ) approach takes the pterional craniotomy one step further in terms of increasing visualization of the surgical corridor and decreasing the working distance of the operator by removing more of the skull base bone. The modified OZ craniotomy has been adequate for reaching parasellar lesions and is the preferred approach when additional bony removal is necessary for the resection of large lesions with superior and posterior extensions. This modified OZ approach is actually an extended frontotemporal craniotomy that includes a supraorbital osteotomy. The frontal and temporal bone flap, usually removed for a traditional pterional craniotomy, in this case also includes the orbital rim from just lateral to the supraorbital foramen/notch to as far as just inferior to the frontozygomatic suture. OZ craniotomy provides an expanded corridor in which to reach lesions involving the circle of Willis, including the orbit, paraclinoid and parasellar locations, cavernous sinus, and especially the more cranially located basilar apex region. For the one-piece modified OZ osteotomy approach, the patient’s head position is similar to the one used during the pterional approach, with the head rotated contralaterally ~15 degrees. An incision is begun at the inferior edge of the zygomatic bone 1 cm anterior to the tragus and carried to the contralateral midpupillary line just behind the hairline. The periosteum and superficial layer of the temporalis fascia (including the fat pad) are carried up in one layer with the skin flap by using an interfascial method. Care must be taken when working near the supraorbital notch to avoid cutting the supraorbital nerve and, instead, to release this nerve from its notch. Occasionally, a foramen (20–25%) may house this nerve, in which case the bone around the nerve should be drilled away. The nerve can then be reflected anteriorly along with the scalp flap. Dissection is continued along the orbital rim to the zygomatic process, allowing the scalp to be fully mobilized and reflected anteriorly along these bony edges. The superior and lateral periorbita is then carefully dissected away to a depth of ~1.5 to 2 cm. Care must be taken to keep the periorbita intact to lessen the chance of postoperative periorbital ecchymosis. The details of this modified OZ craniotomy have been previously described by Balasingam el al.8 Two burr holes are placed: one above the root of the zygoma and one at the keyhole. A craniotome is used to complete a frontotemporal craniotomy from the first burr hole above the zygoma toward the orbital rim just lateral to the supraorbital foramen/notch. However, further progress of the craniotome with the foot plate is stopped at the orbital roof (Fig. 12.21). The foot plate is then “turned around on itself” to expand the last few millimeters of bony cut to create enough space for removing the foot plate. Alternatively, the drill may be backed out along the calvarial bony cut back to the original burr hole and removed. A spatula may be used to protect the orbital contents during orbital osteotomy. Next, the foot plate is removed and a straight side-cutting B1 drill bit (Midas Rex, Fort Worth, TX) is mounted on the drill to complete the first orbital osteotomy over the orbital rim (Fig. 12.21). Next, using a craniotome, the neurosurgeon will create a bony cut from the first burr hole at the root of the zygoma toward the keyhole (the cut is bordered inferiorly by the temporalis muscle), and another cut from the keyhole backward toward the first burr hole (these latter two cuts are limited by the bone over the pterion, which may be thinned with the B1 bit). Fig. 12.22 The second orbital osteotomy involves making a cut (with the B1 drill bit) from the keyhole extending inferiorly and then anteriorly below the frontozygomatic suture to disconnect the frontal process of the zygomatic bone. (Used with permission from Clarian Health.) The second orbital osteotomy involves making a cut (with the B1 drill bit) from the keyhole extending inferiorly and then anteriorly below the frontozygomatic suture to disconnect the frontal process of the zygomatic bone (Fig. 12.22). The orbital contents are again protected by a spatula, and the angle of the drill remains perpendicular to the plane of the bone at all times. The final and third orbital osteotomy will require the use of a thin, small osteotome to disconnect the orbital roof from the keyhole toward the first orbital osteotomy cut just lateral to the supraorbital foramen/notch. Two cotton patties may be used to protect the frontal dura superiorly and the periorbita inferiorly from the osteotome (Fig. 12.23). These three osteotomy cuts will disconnect the superior and lateral orbital attachments, allowing completion of a supraorbital osteotomy. The craniotomy bone flap is now reflected anteroinferiorly, and additional bony removal posteriorly along the roof of the orbit can be accomplished. The pterion is dilled away, and the dura is opened in a curvilinear fashion centered over the pterion. Inferior traction along the frontal dura over the orbit with tack-up sutures will gently depress the orbital contents inferiorly and allow an unobstructed view along the inferior frontal lobe toward the optic chiasm. Dissection, retraction, and tumor removal may proceed as in the pterional approach. A transsylvian approach can be performed similarly to a pterional approach but can afford a shorter working distance with access to the parasellar region.9 Complications of the OZ approach are similar to those of the pterional route, although the risk for entry into the frontal sinus and cosmetic deformity is slightly higher. Removal of the lateral wall risks injury to the globe, and removal of the orbital roof risks injury to the optic nerve. Although providing superior visualization of the parasellar region and reducing frontal lobe retraction, this approach is also more time-intensive and is not performed as commonly as the pterional craniotomy. Most of the lesions in the parasellar space are approached through the pterional or OZ approaches. Large lesions with significant bilateral extension along the optic apparatus may be exposed by using the bifrontal approach. The potential advantage of this approach is the operative wide bilateral window it provides and the direct visualization of the anterior optic pathway and lamina terminalis.6 The presence of a postfixed chiasm is another reasonable indication for this approach. However, we have rarely employed this route because the classic pterional approach is adequate to remove larger tumors. As tumor removal proceeds, the working corridor expands and additional exposure is not usually necessary. After induction of general anesthesia and endotracheal intubation, the patient’s head is fixed in a Mayfield head holder with the head extended 15 to 20 degrees to allow gravitational retraction of the frontal lobes. Lateral rotation of the head is not needed for this midline approach. A lumbar drain is generally placed before the surgery is begun. The surgeon incises the scalp beginning 1 cm anterior to the tragus and continuing to 1 cm anterior to the opposite tragus, staying behind the hairline. The incision should be sinusoidal in shape and kept behind the hairline for cosmesis. An incision is made through the galea, which is then elevated from the pericranium with sharp dissection. It is necessary to maintain the periosteal layer intact because it will be used later to cover the frontal sinus. An attempt is also made to preserve the main trunk of the superficial temporal arteries bilaterally by dissecting through the superficial and subcutaneous layers of the skin within the first and last 3 cm of the incision. As separation of the galea and periosteum progresses anteriorly, the supraorbital nerves are carefully preserved and elevated as described above. An incision in the pericranium is made 5 cm superior to the supraorbital rim. A subperiosteal dissection is performed down over the frontal bone and laterally to the superior temporal lines, and a periosteal flap is reflected anteriorly while the supraorbital nerves are preserved. This creates a vascularized periosteal flap for covering the frontal sinus at the end of the procedure. Two burr holes are placed in the region of the keyholes as well as one burr hole over the superior sagittal sinus ~3 cm anterior to the coronal suture (the superior extent of the craniotomy depends on the size of the lesion). Using a craniotome, the surgeon elevates a craniotomy as low and close to the orbital roof as possible. If the frontal sinus is large, a B1 bit without a foot plate may be used to complete the osteotomy over the anterior and posterior walls of the frontal sinus. The bone is removed in one piece, with the dura left intact. Attention is then turned to the frontal sinus. The sinus is exenterated from its mucosa, packed with muscle or fat, and covered with Tisseel (Baxter, Deerfield, IL). The dura is incised in a U-shape with the base along the orbital floor. The anterior part of the sagittal sinus is ligated and coagulated along the superior edge of the craniotomy. The falx cerebri is cut, and the dura is retracted anteriorly with stay sutures. A Greenberg retractor is affixed to the Mayfield head holder, and gentle retraction is placed on each frontal lobe as it is elevated. CSF may be drained in increments of 10 to 20 mL up to a total of 60 mL from the lumbar drain to afford more brain relaxation. The arachnoidal cistern surrounding the olfactory bulb and tracts can be opened to allow further drainage of CSF. Sharp dissection is then performed to release the olfactory nerves from the orbital surface of the frontal lobes to the level of the olfactory trigone. During this dissection, the olfactory artery arising lateral to the anterior cerebral artery or collateral branches distal to the anterior communicating artery should be preserved.10 At the terminus of the olfactory nerve dissection, the basal interhemispheric fissure will demonstrate overhanging distal A2 segments of the anterior cerebral arteries. The chiasmatic and lamina terminalis cisterns can be exposed with sharp dissection. The anterior communicating artery and the optic chiasm will then come into view. Incision of the lamina terminalis will provide access to the tumor behind the optic chiasm and within the third ventricle. With the tumor now in view, careful dissection from the surrounding structures with incremental debulking may be conducted until adequate tumor resection is obtained. Further details concerning the treatment of individual lesions can be found in preceding chapters of this book. Following resection of the tumor, meticulous hemostasis is obtained. Copious irrigation is performed to remove any residual blood. The dura is closed in a “watertight” fashion. A Gelfoam (Braun AG, Melsungen, Germany) sponge is placed extradurally. The frontal sinus is again inspected, packed with more muscle and bone, and covered with the pericranial flap. The bone is fixed with titanium Cranio-Fix plates (Aesculap AG, Tuttlingen, Germany). Finally, the galea is closed with interrupted sutures, and the skin is closed with staples. An optional subgaleal drain may be left in for 24 hours. This approach may be modified to gain further visualization of more superiorly located tumors while minimizing frontal lobe retraction. The orbital roof just medial to the supraorbital notch may be osteotomized bilaterally with a craniotome. The orbital contents should be stripped from the bone to the depth of the posterior ethmoidal artery before this osteotomy. A vertical cut between the crista galli and the supraorbital bar defines the posterior edge of the extended bone flap. The inferior cut is through or just superior to the frontonasal suture. At the end of the procedure, the bone can be replaced with two 2-hole, low-profile titanium plates and titanium screws along the supraorbital bar. The subfrontal approach also carries specific risks and challenges. The frontal sinus may be entered via this approach and should be exenterated as described above. The subfrontal approach also increases the risk for olfactory nerve injury, with the patient permanently anosmic postoperatively. The sacrifice of the superior sagittal sinus, although anterior to the coronal suture, may be associated with frontal lobe venous infarction. Retraction of both frontal lobes increases the risk for frontal lobe injury. The unilateral subfrontal route has the advantages of requiring less surgical time to complete than the bilateral subfrontal approach and providing an anterior and nearly panoramic view of the sellar and parasellar lesions. This approach may be more appropriate for lesions that extend anteriorly or laterally on one side and is typically used for lesions located more anteriorly in the parasellar region, just above the pituitary gland and around the optic nerves. The unilateral subfrontal approach may provide adequate visualization of the anterior midline lesions, as does the bilateral subfrontal approach, without the need for ligation of the superior sagittal sinus or bilateral dissection of the olfactory bulb and tract.7 After induction of general anesthesia and intubation, the patient is positioned supine with the head in a Mayfield head holder and rotated between 10 and 30 degrees contralaterally. The head is extended ~30 degrees, with the zygoma elevated to the highest point. The skin incision starts 1 cm anterior to the tragus and 1 cm above the zygomaticarch and extends behind the hairline to the contralateral midpupillary line. The scalp flap is elevated with sharp dissection between the galea and periosteum. The superficial fat pad is elevated with the skin flap as in the pterional approach to preserve the temporal branch of the facial nerve. Dissection is continued to the supraorbital rim and the frontozygomatic suture. The temporalis muscle is separated from the anterior aspect of the superior temporal line and the frontozygomatic process. This muscle is then retracted posteriorly11 and the pericranium is sharply removed from the bone, with its pedicle preserved anteriorly. This pericranium is preserved for potential use if the frontal sinus is violated. A single burr hole is placed at the pterional keyhole. A craniotome is then used to cut along the supraorbital margin; the cut is stopped just lateral to the supraorbital notch and then extended as far superiorly as dictated by preoperative imaging. The inferior edge of the craniotomy is then completed close to the level of the orbital roof. If the frontal sinus is entered, exenteration as described above is performed. A U-shaped dural flap is cut so that the base is positioned inferiorly. The dura is then tacked up with stitches. With the operating microscope, gentle elevation of the frontal lobe allows identification of the arachnoid attachments over the olfactory cistern, which is opened. The olfactory nerve is followed posteriorly until the anatomic windows of the subchiasmatic, opticocarotid, and retrocarotid cisterns are found. In the case of a prominent tuberculum sellae that limits visualization in the subchiasmatic space, a diamond burr drill can be used to drill down this bony structure to the level of the anterior intercavernous sinus. If necessary, the sphenoid sinus can be opened and the anterior wall of the sella turcica removed. With the tumor now in view, meticulous dissection from the surrounding structures with incremental debulking of the tumor will allow tumor removal. Once the tumor resection is complete and hemostasis achieved, the dura is closed in a “watertight” fashion, and a Gelfoam sponge is placed extradurally. The frontal sinus is again inspected and, if violated, covered with the pericranial flap. Next, the bone flap is fixated with titanium CranioFix plates. The temporalis muscle is tacked back to the superior temporal line where a cuff of fascia was left intact. The scalp is closed with galeal sutures and the skin stapled. A subgaleal drain may also be placed before closure. The complications associated with the unilateral subfrontal route are very similar to those described for the pterional craniotomy. As with the subfrontal approach, the chance of entering the frontal sinus and postoperative anosmia is greater than with the typical pterional approach The supraorbital keyhole approach, developed most recently and similar to the unilateral subfrontal approach, is indicated for lesions superior to the pituitary gland and around the optic nerve. The advantages of this approach include minimal bone removal and a much smaller skin incision. However, the intracranial exposure afforded by this approach is more restrictive. After induction of general anesthesia, intubation, and supine positioning of the patient, a Mayfield head holder is used to turn the head 15 to 60 degrees contralaterally, depending on the anatomy of the lesion according to preoperative imaging.12 The head is extended slightly to place the zygoma at the highest point, thereby facilitating gravitational retraction of the frontal lobe. The eye is lubricated and taped shut, and the skin is prepared. The eyebrow should not be shaved because of its slow regrowth. An incision is made within the eyebrow just lateral to the supraorbital notch and follows the orbital rim laterally and inferiorly to the end of the eyebrow. Medially, the incision is kept more superficial to avoid injury to the supraorbital nerve and artery. Careful dissection down through the layers of the galea to the periosteum is performed medially to identify and preserve the supraorbital nerve while maximizing the use and extent of the incision. Fish hooks are used to retract the superior skin flap and frontalis muscle, which has been sharply removed from the periosteum in a transverse direction. The orbicularis oculi muscle can be gently retracted inferiorly toward the orbit with retraction sutures. The pericranium is incised in a half moon shape with a base toward the orbit for later use if the frontal sinus is violated.13 A short anterior segment of the temporalis fascia and muscle is released at the superior temporal line. Muscle and fascia are retracted inferolaterally to fully expose the frontozygomatic process and the keyhole. A burr hole inferior to the superior temporal line and posterior to the keyhole is created with a high-speed drill. A half-moon–shaped craniotomy flap similar to that used in the unilateral subfrontal approach is then fashioned and may or may not include the lateral aspect of the orbital rim. An approximate size for this craniotomy is 10 to 15 mm by 15 to 25 mm. For further exposure, the orbital rim can be drilled down to better visualize the floor of the anterior cranial fossa.13 The bony ridges over the anterior cranial fossa floor can also be drilled down to improve exposure. The dura is opened in a U-shaped manner, with the base located inferiorly. With gentle elevation of the frontal lobe, the arachnoid cistern around the olfactory tract is visualized with the operating microscope and opened to allow adequate CSF drainage. The frontal lobe is gently elevated, and the olfactory tract is then traced back to the chiasmatic and carotid cisterns. After these arachnoid cisterns have been opened, the parasellar/suprasellar lesion should be within the field of view, and meticulous dissection from the surrounding structures with incremental debulking of the tumor can be conducted. Following resection of the tumor, hemostasis is obtained, copious irrigation of the cisterns is performed, and the dura is closed with sutures. If the frontal sinus is violated, it can be addressed at this time, as described in previous sections of this chapter. A plate of Gelfoam is placed extradurally. The craniotomy is replaced and fixated with a burr hole cover plate and other combinations of low-profile titanium plates for cosmesis. The temporalis muscle and fascia are returned to their original positions and sewn to their corresponding fascial cuffs. If the pericranial flap was not used to close the frontal sinus, it is placed back over the bone. The scalp flap is closed with galeal and subcutaneous sutures, and a topical skin glue is placed on the skin. The subtemporal approach is infrequently used for suprasellar and parasellar lesions but may be especially useful for those lesions that extend into the infratentorial space, are retrochiasmatic, or extend into the temporal fossa.14 This route offers the most direct approach to remove the lesions in the often “difficult to reach” retrochiasmatic space. Preoperative MR venography may be useful to ensure that the vein of Labbè is not tethered anteriorly and therefore not vulnerable during elevation of the temporal lobe. After induction of general anesthesia and intubation, a lumbar drain can be placed for CSF drainage and brain relaxation to minimize temporal lobe retraction. With the patient in a supine position and use of a Mayfield head holder, the patient’s head is rotated 60 degrees away from the lesion and extended 30 degrees for optimal visualization of the sella and parasellar regions.15 A linear incision 1 cm anterior to the tragus is started 1 cm below the zygomatic arch and extended 1 cm above the superior temporal line. Preservation of the superficial temporal artery is attempted as dissection down to the zygomatic arch and the temporalis fascia is performed. The periosteum is incised over the zygomatic arch and exposed subperiosteally. Anterior and posterior osteotomies at the limits of the arch are then completed, and the arch is plated for later reattachment. Following this, the temporalis muscle is dissected parallel to the line of skin incision and retracted anteriorly and posteriorly with a cerebellar retractor. A small temporal craniotomy is made with an anterior burr hole so that the inferior bony cut is flush with the floor of the middle cranial fossa. The middle meningeal artery can be coagulated and divided where it enters the middle cranial fossa through the foramen spinosum. A U-shaped dural flap is made with an inferior base and tacked out of the way with silk sutures. A wide, self-retaining retractor can then be inserted to gently retract the temporal lobe superiorly and provide exposure to the posterior parasellar area through the middle cranial fossa. Opening the basal cisterns along the third nerve will allow further CSF drainage and further brain relaxation. With the lesion now in view, dissection from the surrounding structures and incremental debulking of the tumor can proceed. Following resection of the tumor, hemostasis is obtained, copious irrigation of the cisterns is performed, and the retractors are removed. The dura is closed with sutures, and a plate of Gelfoam is placed extradurally. The bone flap is fixated with titanium CranioFix plates, and the zygomatic arch is reattached with low-profile titanium plates. The muscle and scalp are closed in anatomic layers with interrupted sutures and staples. Although the subtemporal approach offers a unique corridor to the retrochiasmatic tumor, it is limited by the restricted access it provides to the superior and anterior parasellar space. Postoperative difficulty in mandibular movement due to masseter and temporalis muscle dissection is frequent. In addition to the common risks of craniotomies mentioned in the section on the pterional approach, injury to the branches of the facial nerve just below the zygomatic arch is of unique concern with this approach. The significant temporal lobe retraction necessary during this surgery places the lobe at risk, and retraction injury can be especially symptomatic in the dominant hemisphere. The transcranial removal of parasellar lesions requires proficiency in microsurgical techniques. The neurosurgeon should not focus too much on the “exposure,” but more on “what to do when we get there” in terms of handling the tumor and surrounding cerebrovascular structures. The classic pterional approach is a versatile route that allows safe exposure and removal of most parasellar lesions. One must at all times look out for the optic nerve and other adjacent cerebrovascular structures and remain patient while handling the tumor. “Pulling” the tumor indiscriminately and cutting without scrutinizing the tips of the microscissors can be regretted later. It is acceptable and preferable to say “here it is” and be wrong than to say “there it was” and be right.
 Preoperative Preparation
Preoperative Preparation
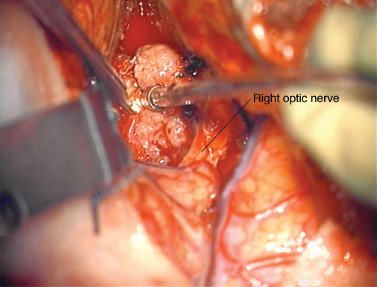
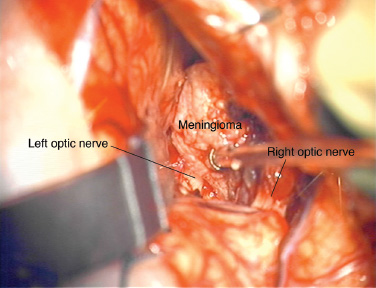
 Pterional Approach
Pterional Approach
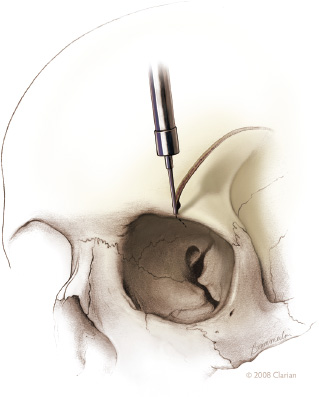
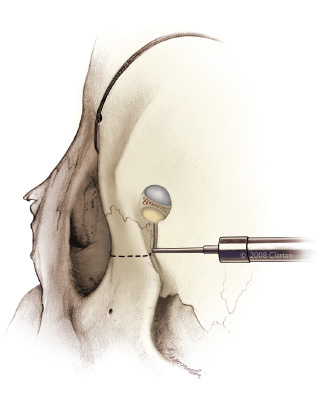
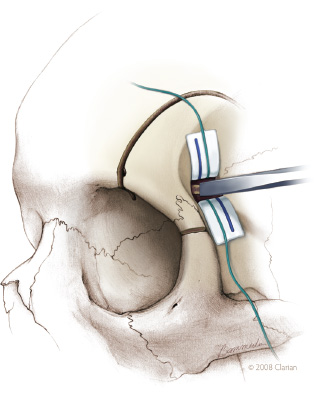
 Orbitozygomatic Approach
Orbitozygomatic Approach
 Bifrontal Approach
Bifrontal Approach
 Unilateral Subfrontal Approach
Unilateral Subfrontal Approach
 Supraorbital Keyhole Approach
Supraorbital Keyhole Approach
 Subtemporal Approach
Subtemporal Approach
 Conclusion
Conclusion
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



