17 Trauma
I. Key Points
– The thoracolumbar spine (T11–L1) is the most common site of spinal injury.
– Surgical treatment is indicated for progressive neurologic impairment, patient mobilization, mechanical instability, and intractable pain.
– Recognition is key to management and prevention of secondary injury.
II. General Principles
– Field management
• A, airway; B, breathing; C, circulation
• Spinal immobilization
 Rigid cervical collar, lateral bolsters, rigid backboard
Rigid cervical collar, lateral bolsters, rigid backboard
 Pediatric patients require recessed head board or pediatric board.
Pediatric patients require recessed head board or pediatric board.
– Emergency room management
• Repeat ABCs; add disability and exposure
• Standard imaging
• Neurogenic shock
 Hypotension in the presence of bradycardia
Hypotension in the presence of bradycardia
 Management with vasopressors and modest fluid resuscitation
Management with vasopressors and modest fluid resuscitation
– Classification
• American Spinal Injury Association (ASIA) scoring scale (Table 17.1)
 Complete: no motor or sensory function below zone of injury
Complete: no motor or sensory function below zone of injury
 Incomplete: partial motor or sensory function below zone of injury (Table 17.2)
Incomplete: partial motor or sensory function below zone of injury (Table 17.2)
• Ten to 15% of patients have noncontiguous spinal fractures.
• Orthogonal radiographs (anteroposterior [AP]/lateral C, T, and LS spine)
• Computed tomography (CT)
 Useful for visualizing occipital-cervical and cervicothoracic junctions
Useful for visualizing occipital-cervical and cervicothoracic junctions
 Must include sagittal and coronal reconstructions if plain x-ray not utilized
Must include sagittal and coronal reconstructions if plain x-ray not utilized
 Not as useful for ligamentous injury assessment
Not as useful for ligamentous injury assessment
• Magnetic resonance imaging (MRI)
 Required in all cases with neurologic impairment or deficit.
Required in all cases with neurologic impairment or deficit.
 Ligamentous structures visualized on T1.
Ligamentous structures visualized on T1.
 Edema visualized on T2 with short tau inversion recovery (STIR).
Edema visualized on T2 with short tau inversion recovery (STIR).
– Steroid management
• Controversial, should be based on institutional protocol (see Chapter 10).
– Surgical timing1
• Early decompression (<72 h) may improve neurologic outcomes.
• Early decompression (<24 h) may result in better clinical outcomes.
Table 17.1 ASIA Neurological Scoring System
| Grade | Description | |
| A | Complete: No motor or sensory function is preserved in the sacral segments | |
| B | Incomplete: Sensory but not motor function is preserved below the neurologic level and includes the sacral segments | |
| C | Incomplete: Motor function is preserved below the neurologic level, and more than half of the key muscles below the level have a muscle grade <3 | |
| D | Incomplete: Motor function is preserved below the neurologic level, and at least half of the key muscle groups below the level have a muscle grade >3 | |
| E | Normal |
Note: The caudal-most normal level is the neurologic level.
Table 17.2 Incomplete Spinal Cord Injury Patterns
| Syndrome | Prognosis | Description | ||
| Central cord | Fair | Due usually to hyperextension injury with greater upper extremity involvement and more proximal than distal muscle groups | ||
| Anterior cord | Poor | Due to injury of anterior spinal artery; loss of pain, temperature, and motor | ||
| Brown-Sequard | Best | Due to hemi-transection of cord or lateral injury; ipsilateral motor loss, vibration, and position sense and contralateral pain and temperature | ||
| Posterior cord | Fair | Loss of vibration and position sense |
III. Cervical Trauma
Atlanto-occipital Dissociation (Fig. 17.1)
– Background
• Clinical suspicion paramount
• Mechanism: high-energy rotational or flexion-extension force
– Signs, symptoms, and physical exam
• Often fatal; neurologic presentation can range from no deficits to quadraparesis2
• Derangements in cardiorespiratory parameters common
– Neuroimaging
• Powers ratio: ratio of distance from basion to C1 lamina divided by distance from opisthion to anterior ring of C1
 Identifies anterior subluxation if ratio >1
Identifies anterior subluxation if ratio >1
 May miss posterior subluxation
May miss posterior subluxation
• Wackenheim line
 Line from posterior surface of clivus—normally its inferior extension should barely touch posterior aspect of odontoid tip
Line from posterior surface of clivus—normally its inferior extension should barely touch posterior aspect of odontoid tip
 If line runs behind odontoid, there is posterior dissociation.
If line runs behind odontoid, there is posterior dissociation.
 If line runs in front, there is anterior dissociation.
If line runs in front, there is anterior dissociation.
• Atlanto-occipital condyle distance
 Should be less than 5 mm
Should be less than 5 mm
– Treatment
• Closed reduction with halo-vest application or occipitocervical fusion
• Traction should generally be avoided (10% risk of neurologic deterioration).
– Surgical pearls
• Obtain a CT angiogram (CTA) or MR angiogram (MRA) to assess vertebral artery integrity as part of the preoperative planning.
• Use of MRI for assessing integrity of ligaments may help with decision to fuse occiput to C1, C2, or a more caudal spot.
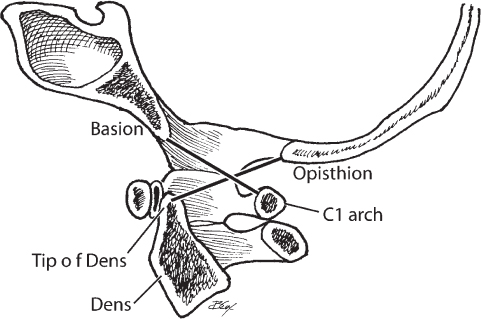
Fig. 17.1 Powers ratio for assessing craniovertebral stability.
Atlas (C1) Fracture
– Background
• Neurologic injury is rare due to large space available for the spinal cord.
• Can occur anterior, posterior, or combined (Jefferson)
• Status of transverse atlantal ligament (TAL) is critical to surgical decision making.
• Mechanism is axial loading.
– Signs, symptoms, and physical exam
• Typically does not lead to neurologic deficits
• With severe fractures, complete and incomplete injuries are possible, including medullary dysfunction.
– Neuroimaging
• Open-mouth odontoid view to assess the relationship of lateral mass of C1 on C2
• Spence rule (>7 mm composite overhang is unstable)
• CT scan with coronal and sagittal reconstruction
• CTA to rule out vertebral artery dissection/occlusion
• MRI to assess TAL integrity
– Treatment
• Rigid cervical orthosis or halo for 3 months if TAL intact
• C1-C2 fusion if nonunion or TAL incompetent
– Surgical pearls
• Obtain a CTA or MRA to assess vertebral artery integrity as part of the preoperative planning.
Axis (C2) Fracture and Traumatic Spondylolithesis of C2 (Hangman’s Fracture)
– Background
• Associated with high-velocity trauma
• C2 fractures among the most common spinal fractures in the elderly
• Mechanism is a combination of hyperextension, compression, and rebound flexion (Fig. 17.2).
– Signs, symptoms, and physical exam
• Patients are typically asymptomatic with nonangulated, non-displaced fractures.
• Complete or incomplete injuries are possible with severe fractures.
• Cerebellar findings (nausea/vomiting, asymmetric exam, ataxia) may suggest vertebral artery injury.
– Neuroimaging
• CT scan with reconstructions
• CTA to rule out vertebral artery dissection/occlusion
– Classification/treatment
• Type I: minimal displacement (<3 mm) and halo for 12 weeks
• Type II: significant displacement (>3 mm) and angulation >11 degrees
 Cervical traction to reduce and halo for 10 to 12 weeks
Cervical traction to reduce and halo for 10 to 12 weeks
• Type IIa: minimal displacement (<3 mm) but angulation >11 degrees
 Reduction in extension followed by halo; avoid traction
Reduction in extension followed by halo; avoid traction
• Type III: associated facet dislocation—anterior C2-C3 or posterior C1-C3 fusion
– Surgical pearls
• Obtain a CTA or MRA to assess vertebral artery integrity as part of the preoperative planning
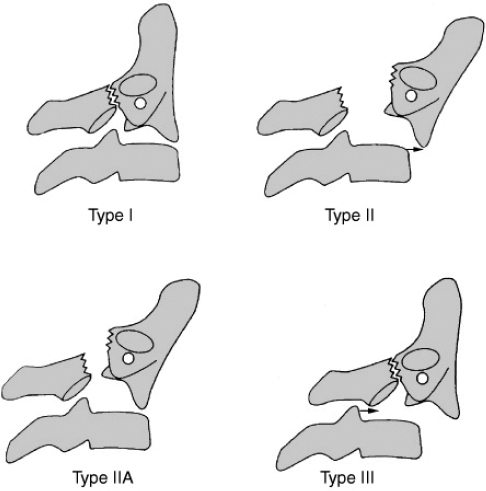
Fig. 17.2 The Levine and Edwards classification of traumatic spondylolistheseis of the axis (hangman’s fracture). (From Feliciano DV, Mattox KL, Moore EE. Trauma, 6th Edition; http://www.access-surgery.com.) Copyright © The McGraw-Hill Companies, Inc. All rights reserved.
Dens Fracture (C2)
– Background
• Among the most common spinal fracture injuries in the elderly after falls
• Sometimes associated with simultaneous C1 fractures
• Mechanism: hyperflexion or hyperextension (Fig. 17.3)
– Signs, symptoms, and physical exam
• Neck pain and tenderness on palpation typical
• Usually does not cause neurologic deficits (due to the width of the canal in this region)
• Severe angulated fractures may cause complete or incomplete injuries
– Neuroimaging
• CT scan with reconstructions recommended even if fracture is evident on plain radiograph
• MRI may be helpful for assessing integrity of cruciate ligament (surgical implications)
– Treatment3
• Type 1: avulsion fracture at tip—rigid collar
• Type II: at the waist/base (Fig. 17.1)—rigid collar versus halo versus early fixation
 Anterior odontoid screw or posterior C1-C2 instrumented fusion
Anterior odontoid screw or posterior C1-C2 instrumented fusion
• Type III: within the body—halo or rigid collar, based on displacement
• Posterior fixation options include wiring, transarticular, pedicle/pars, intralaminar
– Surgical pearls
• Ensure that the anterior cruciate ligament is intact before attempting an anterior odontoid screw fixation.
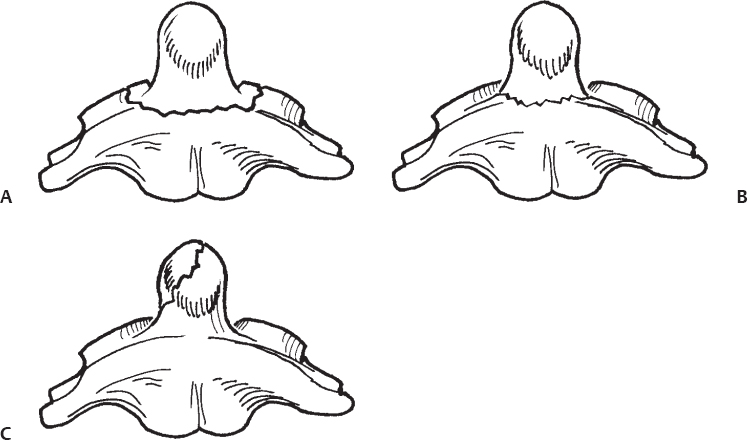
Fig. 17.3 (A–C) Anderson D’Alonzo classification of dens fractures. (A) Type III fracture, (B) Type II fracture, (C) Type I fracture.
Subaxial Spine (C3-C7)
– Background
• Particularly common in high-speed motor crashes and diving accidents
• Allen-Ferguson classification system, based on mechanism
 Flexion compression: blunting at anterosuperior margin → loss of anterior height → teardrop fragment → <3 mm of displacement of posterior body into canal → more severe displacement of posterior body into canal
Flexion compression: blunting at anterosuperior margin → loss of anterior height → teardrop fragment → <3 mm of displacement of posterior body into canal → more severe displacement of posterior body into canal
 Vertical compression: central cupping of one end plate → disruption of both end plates
Vertical compression: central cupping of one end plate → disruption of both end plates
 Flexion distraction: failure of posterior ligamentous complex with facet subluxation only in flexion → unilateral facet dislocation → bilateral facet dislocation → bilateral facet dislocation with at least 100% vertebral body displacement
Flexion distraction: failure of posterior ligamentous complex with facet subluxation only in flexion → unilateral facet dislocation → bilateral facet dislocation → bilateral facet dislocation with at least 100% vertebral body displacement
 Extension compression: unilateral posterior arch fracture → bilaminar fractures → circumferential disruption
Extension compression: unilateral posterior arch fracture → bilaminar fractures → circumferential disruption
 Extension distraction: failure of anterior ligamentous complex → involves posterior ligamentous complex
Extension distraction: failure of anterior ligamentous complex → involves posterior ligamentous complex
• Lateral flexion: ipsilateral fractures of the centrum and posterior arch → fracture of body with contralateral bony or ligamentous failure in tension
– Signs, symptoms, and physical exam
• Mild compression fractures or nondisplaced facet fractures may not cause deficits.
• Significant fractures (either in anterior or posterior columns) may cause devastating deficits and/or radiculopathies.
– Neuroimaging
• CT and MRI typically necessary to appreciate the extent of injury.
• CTA recommended if any fracture involves the transverse foramen.
– Treatment
• Based on stability and neurologic injury
• Considerations
 Is there mechanical instability?
Is there mechanical instability?
 Is there neurologic compromise necessitating direct or indirect decompression?
Is there neurologic compromise necessitating direct or indirect decompression?
 Are there patient factors (e.g., multitrauma)?
Are there patient factors (e.g., multitrauma)?
• Stable: nonoperative, rigid cervical orthosis
• Unstable: surgical fusion via anterior versus posterior versus combined approach
– Surgical pearls
• Ending a fixation construct at C7 posteriorly may lead to delayed cervical-thoracic junction kyphosis.
• Ensure the posterior elements are intact when an anterior cervical vertebral body fracture is present. Posterior element involvement may indicate a highly unstable, three-column injury.
Thoracolumbar Fractures
– Background
• Most common region is the thoracolumbar junction (T11–L2).
• Due to transition from fixed thoracic spine to mobile lumbar spine
• Thoracolumbar injury classification and severity score (TLICSS) proposes that operative treatment be based upon three factors4,5:
 Morphology of fracture
Morphology of fracture
 Posterior ligamentous complex
Posterior ligamentous complex
 Neurologic status
Neurologic status
• Compressive flexion (Fig. 17.4)
 Instability factors: >50% height loss, >30 degrees angulation, >30 degrees of focal kyphosis
Instability factors: >50% height loss, >30 degrees angulation, >30 degrees of focal kyphosis
• Flexion-distraction injury (Chance fracture/seatbelt injury)
 Bony fracture without subluxation or dislocation
Bony fracture without subluxation or dislocation
 Treat with hyperextension body brace or cast
Treat with hyperextension body brace or cast
 Ligamentous injury
Ligamentous injury
 Posterior instrumented fusion to restore tension band
Posterior instrumented fusion to restore tension band
• Torsional flexion (fracture-dislocation)
• Vertical compression (burst fractures)
 Anterior approach allows better decompression of retropulsed fragment.
Anterior approach allows better decompression of retropulsed fragment.
 Posterior approach allows restoration of the tension band and reduction.
Posterior approach allows restoration of the tension band and reduction.
 Combined approach allows for optimal decompression and reconstruction.
Combined approach allows for optimal decompression and reconstruction.
– Signs, symptoms, and physical exam
• Significant fractures at the level of the conus may cause bowel/bladder dysfunction as well as significant lower extremity weakness.
• Tenderness on palpation with or without neurologic deficits after high-velocity accidents should raise suspicion of a spinal fracture.
– Neuroimaging
• CT with coronal and sagittal reconstructions best for evaluation of middle column
• MRI best for spinal cord and disc evaluation
– Treatment
• Stable: nonoperative management—brace
• Unstable: operative reconstruction ± decompression
 Neurologic injury considered unstable injury
Neurologic injury considered unstable injury
• Approach
 Anterior approach optimal for decompression
Anterior approach optimal for decompression
 Posterior ligamentous complex injury requires tension band reconstruction.
Posterior ligamentous complex injury requires tension band reconstruction.
 Urgent medical/critical care stabilization/optimization
Urgent medical/critical care stabilization/optimization
 Surgical intervention when medically optimized
Surgical intervention when medically optimized
 Early treatment may provide better outcomes and fewer complications.
Early treatment may provide better outcomes and fewer complications.
 Definition of “early” is controversial.
Definition of “early” is controversial.
– Surgical pearls
• Progressive neurologic deficits (due to expanding hematoma, for example) are atypical but require urgent surgical intervention.
• Short-segment and long-segment posterior fixation, as well as anterior reconstruction, have all been shown to be effective biomechanically. Choice of approach must be tailored to type, location, and severity of fracture.
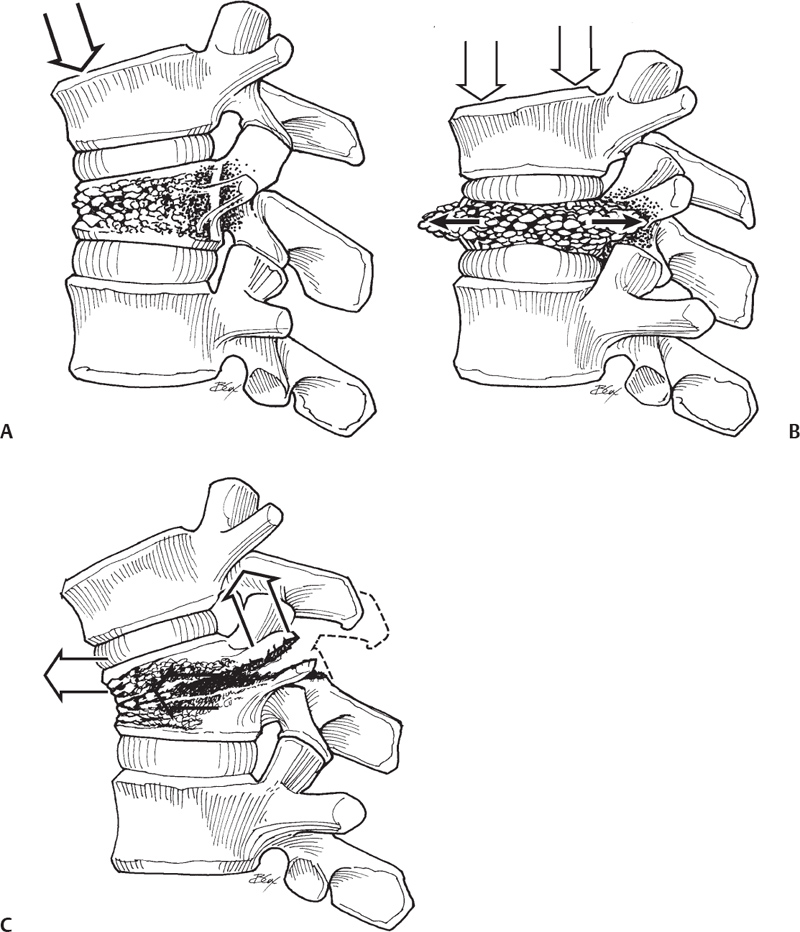
Fig. 17.4 (A–C) Compression. (A) compression fracture, (B) burst fracture, (C) chance-type fracture.
Sacral Fractures
– Background
• Classification (Fig. 17.5)
 Zone 1: across the ala and can affect L5 nerve root
Zone 1: across the ala and can affect L5 nerve root
 <10% have neurological injury
<10% have neurological injury
 Zone 2: through the neuroforamina, causing unilateral symptoms
Zone 2: through the neuroforamina, causing unilateral symptoms
 Zone 3: through the body and highest incidence (~56% with neurologic injury)
Zone 3: through the body and highest incidence (~56% with neurologic injury)
 Others
Others
 Transverse (may miss on plain radiograph)
Transverse (may miss on plain radiograph)
 U-shaped fractures
U-shaped fractures
 Results from axial load
Results from axial load
• Central fractures (zone 3) have the highest incidence of neurologic injury.
• L5 most common nerve root affected
• Mechanism: fall from height or associated pelvic ring fracture
– Signs, symptoms, and physical exam
• Depending on zone involved, sacral fractures can result in significant deficits from L5 root to lower sacral roots.
• Ankle dorsiflexion/plantar flexion affected with L5/S1 involvement
• Bowel/bladder function affected with sacral root involvement
– Neuroimaging
• Transverse fractures may be missed on pelvic CT and AP radiographs.
• Best seen on lateral radiograph of the sacrum or CT reconstructions
– Treatment
• Minimally displaced impacted fractures are stable and may be treated nonoperatively.
• Displaced fractures require reduction and fixation.
• Iliopelvic reconstruction/fusion may be required to restore weight-bearing biomechanics.
– Surgical pearls
• Fully threaded screws should be used to avoid overcompression for sacral fractures.
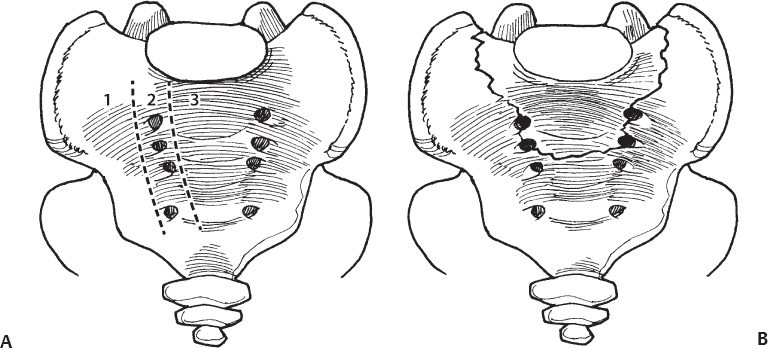
Fig. 17.5 (A–B) Sacral fractures. (A) Zones 1, 2, and 3. (B) U-shaped fracture.
Common Clinical Questions
1. List these incomplete spinal cord injuries in the order of best prognosis to worst.
A. Brown-Sequard, anterior cord, central cord
B. Central cord, Brown-Sequard, anterior cord
C. Brown-Sequard, central cord, anterior cord
D. Anterior cord, central cord, Brown-Sequard
2. A patient presents with a ligamentous flexion distraction injury of the thoracolumbar junction. The patient has focal 40 degrees of kyphosis and a normal neurologic examination. Patient management should include:
A. Hyperextension brace
B. Posterior tension band reconstruction
C. Anterior spinal fusion
D. Physical therapy
3. A polytrauma patient is intubated with an unknown neurologic injury. What is the best modality for assessing acute spinal cord injury?
A. CT scan
B. T1-weighted MRI
C. T2-weighted MRI
D. Flexion and extension cervical radiographs
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






