Traumatic Brain Injuries and Dural Hemorrhages
Juan C. Troncoso
Olga Pletnikova
Trauma of the head and brain accounts for significant mortality and morbidity in contemporary society. Traumatic brain injury (TBI) occurs most frequently as the consequence of road traffic and motor vehicle accidents, falls, blows, and gunshot wounds to the head. Each of these modalities results in fairly specific patterns of macroscopic and microscopic lesions. Examination of these primary traumatic brain lesions, however, is complicated by the development of secondary changes, such as brain swelling and herniations, as well as vascular lesions, hypoxia, and ischemia. In many instances of TBI-motor vehicle accidents in particular-substantial injuries to abdominal and thoracic organs are also present, which can contribute to reduced oxygenation and perfusion of the brain. Also, TBI is frequently accompanied by spinal cord injury (see Chapter 12). For these reasons, the interpretation of lesions in TBI is challenging and cannot be based only on the examination of the brain, but requires a thorough examination of the scalp, skull, and galea, the findings of the general autopsy, and the information gathered at the scene investigation (see Chapters 1 and 3). If the decedent was hospitalized, clinical records and neuroimaging studies could be critical for the interpretation of the lesions and establishing a timeline for events.
The brain is wrapped by the dura mater, skull, and scalp, which constitute a natural helmet that protects the brain from trauma. Moreover, the brain is also floating in cerebrospinal fluid, which works as a shock absorber and provides additional protection (see Chapter 2). The rigid nature of the skull, however, is a limit to the expansion of the brain parenchyma in the event of edema and leads to herniations, that is, the extrusion of brain tissues through natural openings (see Chapter 8). Bone structures may also become the source of injury, and we will discuss the mechanisms of fracture/contusions and the role of the topography of the anterior fossa of the skull in contrecoup injuries of frontal and temporal lobes.
Although it is possible for the neuropathologist to establish precise associations among patterns of brain lesions and some types of trauma, the pathogenesis of neural injury in trauma is complex and, to a large extent, remains to be elucidated. For the purpose of research and experimental study, the pathogenesis of TBI can be artificially divided into a biomechanical component that focuses on the immediate effects of force and mechanical stress on the brain and its covers, followed by downstream cellular and molecular changes. Research into these two components requires different experimental paradigms, with their own advantages and limitations.1, 2 The biomechanical aspects of head and TBI are best examined in large animals and probably the most valuable information in this domain has been gained from studies in nonhuman primates.3, 4, 5 Cellular and molecular changes in TBI are best examined in various experimental models in rodents.6, 7, 8
EPIDEMIOLOGY
The annual number of TBIs in the United States is approximately 1.5 million; of these, 235, 000 require hospitalization, 80, 000 result in severe long-term disability, and 50, 000 cause death. Currently, 5.3 million Americans live with a disability because of head trauma. The leading causes of TBI are falls (28%) and motor vehicle accidents (20%). Although gunshot wounds of the head represent approximately 9% of the causes of TBI, they are fatal in 90% of the cases.9, 10, 11, 12
TOPOGRAPHIC DESCRIPTION OF LESIONS
Lesions of the Scalp
Lesions of the scalp consist of abrasions, contusions, lacerations, and hematomas. A thorough examination of the scalp is important because it allows the physician to locate the site of impact. An important caveat, however, is that severe brain injury may occur in the absence of impact and thus without scalp lesions. Examples of this situation include automobile accident victims and “shaken babies.” For a detailed description of external and scalp lesions, see Chapters 3 and 4.
Fractures of the Skull
Nondepressed fractures that involve the calvaria are common in falls and may have a linear or more complex pattern. In cases of severe trauma, these fractures of the calvaria often extend downward to involve the base of the skull. Depressed fractures are more commonly seen in cases of blunt trauma to the head. As would be expected, depressed skull fractures are frequently the cause of brain contusions and lacerations. Nevertheless, linear fractures may also cause similar lesions, although the magnitude of the parenchymal lesions is milder. At the time of impact, edges of the fracture may actually become depressed, with an internal bevel, for a fraction of a second, before becoming realigned. Fractures of the base of the skull are usually the consequence of severe trauma. These types of fracture are a challenge to clinical detection, because of the complexity of the radiologic images of the base of the skull. Blood in
the ear canal, hemorrhagic discoloration over the mastoid (Battle sign, Fig 3.24), or leak of cerebrospinal fluid through the nose are useful clinical indications of basal skull fracture. A fracture that traverses the entire width of the base of the skull is known as a “hinge fracture” (Fig. 4.26). For additional description of skull fractures, see Chapter 4.
the ear canal, hemorrhagic discoloration over the mastoid (Battle sign, Fig 3.24), or leak of cerebrospinal fluid through the nose are useful clinical indications of basal skull fracture. A fracture that traverses the entire width of the base of the skull is known as a “hinge fracture” (Fig. 4.26). For additional description of skull fractures, see Chapter 4.
LESIONS OF THE COVERS OF THE BRAIN
Hemorrhages of the Dura Mater
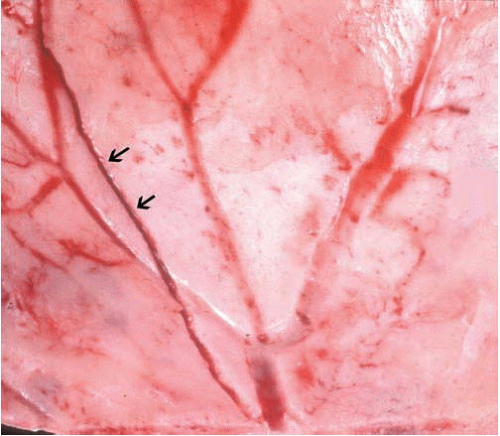
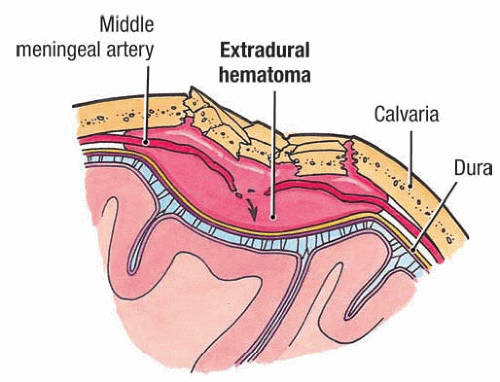
Epidural hemorrhages (EDHs), also known as extradural hemorrhages or hematomas, are located between the dura and the skull, usually under an impact lesion of the scalp and a linear fracture of the skull that lacerates a major meningeal artery. The majority of EDHs are the consequence of traffic accidents (56%); other causes include falls (30%) and blows to the head (10%).13 Large clinical series cite fractures of the skull in 74% to 95% of patients admitted to the hospital with traumatic EDH.13, 14 The most frequent scenario is a fracture of the squamous portion of the temporal bone and laceration of the middle meningeal artery (Fig. 6.1). Less frequently, EDHs occur in the posterior fossa as a consequence of laceration of the posterior meningeal artery.15 Other less common sources of epidural hemorrhages are tears of dural venous sinuses.16, 17 EDHs extend by dissecting the dura from the skull and stop at places where the dura is firmly attached to the inner surface of the skull (i.e., at skull sutures and the insertion of the falx cerebri and tentorium). Thus EDHs are circumscribed and tend to be lens-shaped (Figs. 6.2 and 6.3).
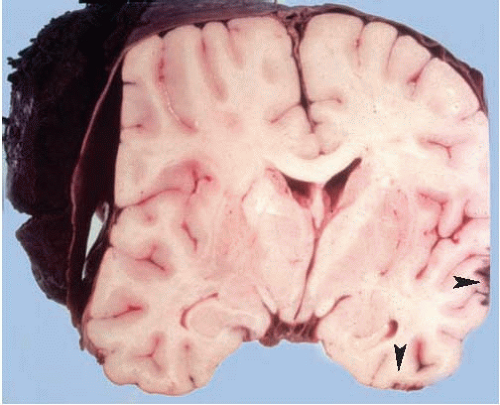
The volume of EDHs is variable, but fatal ones are usually 100 mL or larger.18, 19 EDHs generally represent life-threatening lesions because of their mass effect, leading to increased intracranial pressure and herniations (see Figs. 8.3 and 8.4). This explains why EDHs only exceptionally become chronic, in sharp contrast with subdural hemorrhages.20, 21 Notably, EDHs frequently (75%) occur in the absence of significant parenchymal brain injuries, and therefore, the timely evacuation of the hematoma can result in full functional recovery. Among the remaining 25%, lesions include cerebral contusions, hematomas, and diffuse axonal injury.22 The low incidence of brain contusions is attributed to the absorption of mechanical energy by the fracturing of the skull. This lack of parenchymal brain injury explains also the “lucid interval, ” a clinical scenario commonly associated with this type of hemorrhage.
A subject suffers a fall and hits his/her head, but suffers no or very transient loss of consciousness (which belies the absence of a significant brain lesion), remaining lucid for a while. Then, as hours pass and the epidural hematoma grows, its mass effect causes a deviation of midline, diencephalon, and brainstem, structures resulting in functional impairment of the reticular activating systemand loss of consciousness.
Of note, despite the entrenched notion of the “lucid interval” in EDH, in some series this clinical scenario is present only in 21% of cases.14 Obviously, the “lucid interval” scenario does not apply to subjects who, in addition to the EDH, have parenchymal brain injuries, severe systemic injuries with significant blood loss, or are under the effects of alcohol or other depressant drugs.
EDHs represent neurosurgical emergencies. With prompt evacuation of the hemorrhage, the overall survival of patients with epidural hemorrhages is in the 90% to 95% range, 13, 14 but overall survival is almost 100% in those patients coming to surgery with Glasgow Coma Scale scores of 8 or better.
The use of computed tomography of the head has improved the diagnosis and assessment of EDH. For example, serial computed tomography has demonstrated that delayed onset of EDH is not rare, but may occur in approximately 30% of cases.23
EDH may develop after trivial trauma in individuals with increased bone fragility, such as those with osteogenesis imperfecta.24 Nontraumatic EDH is extremely rare and most commonly associated with infection. Other causes include coagulopathies and tumors of the skull.25 Rapid decompression of chronic hydrocephalus may also result in EDH.26
The forensic pathologist should also be aware that in fire-related deaths, the intense heat can produce fractures of the skull and EDH. In these cases, the blood is clotted, with a granular appearance, and associated thermal injury of the dura and the surface of the brain is present (Fig. 6.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree