56 What is the leading cause of morbidity and mortality in Americans between 1 and 45 years of age?1 Traumatic brain injury (TBI) According to the Traumatic Coma Data Bank (TCDB) what is the outcome for severe TBI?2,3 • Death: 30 to 36% • Persistent vegetative state: <5% • Severe disability: 15% • Moderate disability: 14 to 20% • Good outcome: 25% What are the three components of the Glasgow Coma Scale (GCS)? • Eyes (scores of 1–4) • Motor (scores of 1–6) • Verbal (scores of 1–5) Categorize the head trauma severity based on the GCS. Mild: GCS 14 or GCS 15 and LOC and impaired alertness or memory Moderate: GCS 9–13 Severe: GCS 5–8 Critical: GCS 3–4 What are the two main reasons for the increase in brain injuries in the elderly? 1. The growing ranks of the elderly. 2. The concurrent growth in the number of elderly patients taking anticoagulation or antiplatelet drugs. What are the two types of forces in brain injury? Contact: produces focal injuries (fractures, contusions, hematomas) Inertial: the brain undergoes acceleration and deceleration (translational, rotational, or both), which can occur without head impact: • Translational: leads to focal injuries • Rotational: common with high-speed motor vehicle accidents, causes diffuse injuries What is concussion? A mild TBI, with or without LOC. Alteration of consciousness as a result of closed head injury. Negative finding on computed tomography (CT). Is there evidence of microscopic changes in concussion? No, but there is a transient disturbance in neuronal function. Levels of glutamate increase and the brain enters a hyperglycolytic/hypermetabolic state up to 7 to 10 days after injury. What is a cerebral contusion? Intraparenchymal lesion due to closed head injury, aka hemorrhagic contusion Where are the most common locations for cerebral contusion? Areas where sudden head deceleration causes the brain to impact on bony prominences (inferior frontal cortex and anterior temporal lobe) What is a contrecoup injury? After TBI, the force imparted to the head may cause the brain to be thrust against the skull directly opposite the blow. What is DAI? Diffuse axonal injury. • Result from the disparate densities of the gray and white matter and the consequent difference in centripetal force associated with a rotational vector of injury • Most often occurs in high-speed motor vehicle accident • Present in 50% of all severe TBIs What lesions can be seen in DAI? Hemorrhagic lesions seen most frequently in corpus callosum and dorsolateral rostral brainstem What are the microscopic findings in DAI? Under microscope, axonal retraction balls, microglial stars, and degeneration of white matter fiber tracts can be seen. Fragmentation of axons and axonal swelling appear 24 to 48 hours after trauma. What is important about the development of DAI? Axotomy may not be complete immediately after trauma. Explain secondary axotomy. Secondary axotomy begins with an impairment of axoplasmic transport, cytoskeletal collapse, and secondary disconnection What are the three levels of severity of DAI? • Mild DAI: coma of 6- to 24-hour duration • Moderate DAI: coma of more than 24 hours without decerebrate posturing • Severe DAI: coma of more than 24 hours with decerebrate posturing and flaccidity What is the mortality of severe DAI? 50% What would you include in the initial general physical exam in the ER in addition to the neurological exam (neuro-oriented assessment)? Evidence of basal skull fracture: • Raccoon’s eyes: periorbital ecchymoses • Battle’s sign: postauricular ecchymoses • CSF rhinorrhea/otorrhea • Check for facial fractures • Physical signs of spine trauma And what would you include in your neuro exam (focused and concise)? • Level of consciousness (on the GCS) • Pupils (size and reaction) • Motor exam: (1) if patient cooperative, check motor strength in all four extremities; (2) if not, check for movement of all four extremities • Sensation exam: (1) if patient cooperative, check pinprick and touch in major dermatomes; (2) if not, check for central response to noxious stimulus • Brainstem reflexes: evaluate corneal, gag, and cough reflexes, and if the patient is breathing over ventilator. • Muscle stretch reflexes • Anal sphincter tone and Babinski reflex • Gait and coordination if conscious and cooperative Describe the Glasgow Coma Scale.
Traumatic Brain Injury (TBI)
56.1 Basic Concepts
56.2 ER Evaluation
Motor | Points |
Follows commands | 6 |
Localizes to pain | 5 |
Withdraws from pain | 4 |
Flexor posturing to pain | 3 |
Extensor posturing to pain | 2 |
None | 1 |
Eyes opening |
|
Spontaneous | 4 |
To verbal stimuli | 3 |
To pain stimuli | 2 |
None | 1 |
Verbal |
|
Alert, conversant | 5 |
Confused, disoriented but conversant | 4 |
Intelligible words | 3 |
Unintelligible words | 2 |
None | 1 |
What is the GCS in a patient who, after TBI, is intubated, localizing to pain on the right side, and opens eyes to pain stimuli?
GCS: 8T = M:5, E:2, V:1T
What is delayed deterioration? Describe its possible etiologies.
Referred as “talk and deterioration” or “talk and die,” seen in 15% of patients who do not initially exhibit signs or symptoms4,5
Possible etiologies:
• 75% exhibit intracranial hematoma
• Diffuse cerebral edema
• Hydrocephalus
• Tension pneumocephalus
• Seizures
• Vascular events (dural sinus thrombosis, major artery dissection, SAH, embolism)
• Meningitis
What is the minimum radiographic evaluation needed in TBI?
Noncontrast CT of head and cervical x-ray series
GCS <14, unresponsiveness, depressed level of consciousness, focal deficit, amnesia for injury, altered mental status, seizures, and those with physical findings with moderate risk for intracranial injury.
Who is at moderate risk for intracranial injury?
• Loss of consciousness (LOC)
• Progressive headache (HA)
• Alcohol (ETOH) or drug intoxication
• Age <2 years or suspected child abuse
• Unreliable history
• Signs of basal or calvarial skull fractures
• Serious facial injury
• Significant subgaleal swelling
Classification of diffuse injury (DI) based on initial CT6
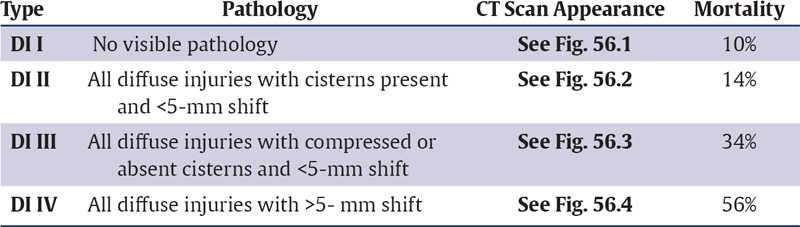
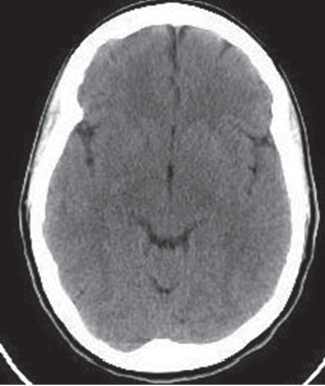
Fig. 56.1 Diffuse injury (DI) type I.
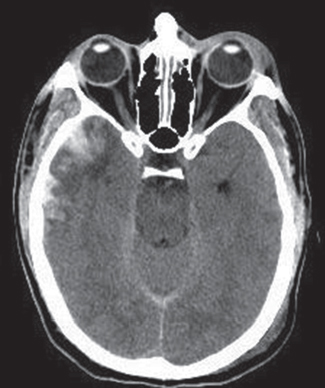
Fig. 56.2 Diffuse injury (DI) type II.
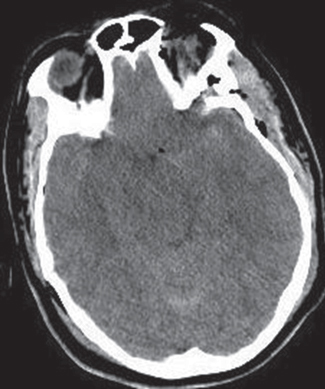
Fig. 56.3 Diffuse injury (DI) type III.

Fig. 56.4 Diffuse injury (DI) type IV.
56.3 Skull Fractures
What is the most common type of skull fracture?
Linear fractures typically over the lateral convexities
What are the criteria to elevate (surgically) depressed skull fracture?7
• >8–10 mm depression (or greater than thickness of skull)
• Deficit related to underlying brain
• CSF leak
• Compound fracture (open)
• Cosmetic region
What is the exception for repairing a depressed skull fracture that meets the above criteria?
Depressed skull fracture overlying and depressing one of the dural sinuses
Alternative: craniotomy technique with proximal and distal venous control
What is the best radiographic study to diagnose a basal skull fracture?8
CT with thin cuts and coronal images
What is the most common location for basilar skull fractures?
Anterior skull base, often involves the cribriform plate, disrupting the olfactory nerve
What structures can be damage in posterior basilar skull fracture?
Posterior basilar skull fractures may extend through petrous bone and internal auditory canal damaging cranial nerves VII and VIII.
Which basal skull fractures may require specific management?
• Persistent CSF rhinorrhea
• When fracture extends into air sinuses and is causing meningitis or brain abscess (may occur years after)
• Cosmetic deformities
• Optic nerve or extraocular muscle entrapment
What are the types of temporal bone fractures?9
Longitudinal fracture and transverse fracture
What is the most common type of temporal bone fracture?
Longitudinal fracture (70–90%): through petrosquamosal suture, usually passes between cochlea and semicircular canals, sparing VII and VIII, but may disrupt ossicular chain
Why does a transverse fracture of the temporal bone have the worst prognosis?
Transverse fracture: perpendicular to external auditory canal (EAC) through cochlea and stretch on geniculate ganglion, damaging VII and VIII
Are steroids indicated for posttraumatic facial palsy?
Often utilized but efficacy unproven. If patient is not improving, then surgical repair may be indicated, but it is not done emergently (40 to 75% will recover).
Do all frontal sinus fractures need to be repaired?
No, only fractures that disrupt the posterior wall with nasofrontal outflow obstructions require surgical repair to prevent intracranial infections.
What is a Ping-Pong ball fracture?
Caving in of a focal area of the skull, seen only in the newborn
What is the treatment for a Ping-Pong ball fracture?
• Observation
• Repair only if the fracture is on the frontal area for cosmesis purposes
What is a growing skull fracture?
It is a fracture line that widens with time, usually asymptomatic. Requires widely separated fracture and dural tear; 90% occur in patients before age 3 years
What is the other name for growing skull fracture?
Posttraumatic leptomeningeal cyst
56.4 Traumatic Intraparenchymal Hemorrhage
What is the most common finding in CT after TBI?10
Subarachnoid hemorrhage, which may be associated with an increased risk of posttraumatic vasospasm
What is the strongest predictor for enlargement of hemorrhagic contusion?11
The presence of traumatic SAH on CT. The second important predictors are the size of the contusion and the presence of SDH.
What are the indications for surgical management in traumatic intracerebral lesions?10
• Signs of progressive neurological deterioration, medically refractory intracranial hypertension, or signs of mass effect on CT
• GCS score of 6 to 8 with frontal or temporal contusions >20 cm3 with midline shift >5 mm and/or cisternal compression
• Any lesion >50 cm3
What are the treatment options for patients with refractory intracranial hypertension (IC-HTN) and diffuse parenchymal injury for impeding transtentorial herniation?
Decompressive procedures:
• Subtemporal decompression
• Temporal lobectomy
• Hemispheric decompressive craniectomy
Bifrontal decompressive craniectomy is a treatment option in which scenario?
Patients with diffuse, medically refractory posttraumatic cerebral edema and IC-HTN
What are the factors that determine outcome in intracerebral hematomas?
• GCS score
• Hematoma volume
• Occurrence of hypoxia
What is a Duret’s hemorrhage?
Hemorrhage into the base of the pons or midbrain, result from disruption of the perforating arteries at the time of uncal herniation; high morbidity and mortality
Delayed traumatic intracerebral hemorrhage12
• Incidence of 1 to 8% in patients with severe TBI
• Occurs most frequently within 72 hours of the trauma in the frontotemporal region as a “countercoup” from parietoccipital trauma.13
• Contributing factors are coagulopathy, hemorrhage into an area of necrotic brain, and loss of tamponade effect after evacuation of extraaxial hematomas.
• Risk factors: diabetes, alcohol use, and advanced age13
• Mortality 50% or higher in most series13
56.5 Epidural Hematoma
In which population is it rare to see epidural hematomas (EDH)?
Before 2 years of age and after age 60; dura is more adherent to the inner table in this group
Is the source of bleeding of the EDH always arterial?
No; 85% arterial bleeding (middle meningeal artery), and the remainder from bleeding from the middle meningeal vein and dural sinus
What is the most common location of EDH?
75% laterally over the hemisphere with the epicenter at the pterion. The rest in the frontal, occipital, and posterior fossae.
What is Kernohan’s phenomenon?
Shift of the brainstem away from a mass (due to mass effect), which may compress the opposite cerebral peduncle on the tentorial edge, causing hemiparesis ipsilateral to the side of the mass lesion (which is a false localizing sign)
What is the classic CT appearance of EDH?
85% of EDHs are hyperdense biconvex (lenticular) adjacent to skull; in 10% the side against the skull is convex and the side along the brain is straight; in 5% it is crescent shaped.
What are the indications for surgical evacuation of an EDH?14
• Any symptomatic EDH
• Asymptomatic but >1 cm in its thickest measurement (difficult for the brain to reabsorb)
• In pediatrics, threshold for surgery should be very low
What are the risk factors of a delayed EDH?
• Lowering ICP medically or surgically (evacuating contralateral hematoma)
• Coagulopathies
• Rapidly correcting shock
What is important about posterior fossa EDH?15
85% have an occipital fracture, most commonly from a dural sinus tear, and surgeon should have low threshold for surgical evacuation.
What is important about hematomas that compress the temporal lobe?
They can rapidly cause uncal herniation with minimal enlargement and with no elevation in ICP. Surgeon must have a low threshold for evacuation.
56.6 Subdural Hematoma
Why is a subdural hematoma (SDH) more lethal than an EDH?
The magnitude of impact damage is much higher; there is always associated injury to underlying brain parenchyma and cerebral edema.
How often is an underlying cerebral contusion seen in SDH?16
Up to 67% of patients with SDH have an underlying contusion.
What are the biochemical findings on the brain tissue underlying an evacuated SDH, and what do they indicate?16
The biochemical pattern of increased lactate and pyruvate and decreased partial pressure of oxygen in brain tissue (PbtO2) may indicate evolving injury in the brain tissue that was previously compressed by the SDH.
What is the classic CT appearance of acute SDH?
Hyperdense crescentic mass of increased attenuation adjacent to inner table; usually on convexity but may be interhemispheric, along tentorium, or in posterior fossa
Why can acute SDH be hypodense on CT?
Because of the low hemoglobin content, seen in up to 10%
What is different between SDH and EDH on CT?
SDH is more diffuse, concave over brain surface, and often less dense (mixed with CSF)
What are the SDH density changes on CT with time?
Hyperdense | 1–3 days | Acute |
Isodense | 4 days to 2–3 weeks | Subacute |
Hypodense | >3 weeks | Chronic |
What are the indications for surgery in SDH?17,18
• Any symptomatic SDH
• SDH greater than 1 cm at the thickest point (5 mm in pediatrics) with >5 mm of midline shift
What is the mortality of patients with surgically evacuated acute subdural hematomas?
• 40 to 60% depending on the series19,20; if initial GCS score is 3, mortality approaches 100%.
• Functional recovery occurs in approximately 38%.
What factors may increase hospital mortality following traumatic SDH in the elderly?21
• Initial GCS ≤7
• Age >80
• Acute subdural hematoma
• Patient who required craniotomy
What actions may improve outcome in traumatic subdural hematoma?
• Early management of ICP
• Early surgical evacuation in those patients who meet criteria
What are the CT findings predictive of outcome?
• Hematoma thickness
• Midline shift
• Presence of underlying brain swelling or contusion
Is the source of bleeding of the SDH always venous?
No, SDH can result from arterial ruptures (usually cortical arteries).
How can we differentiate an SDH resulting from arterial rupture from those resulting from venous rupture?22
SDH resulting from arterial rupture are generally located in the temporoparietal region, and those caused by bridging vein rupture are in the frontoparietal parasagittal region.
Is the shape of the hematoma the same between arterial and venous SDH?
No, venous SDH tends to have a homogeneous width, whereas arterial SDH tends to have a more pronounced thickening in the middle third.
What is the positive displacement factor?
When the midline shift exceeds the hematoma thickness; the prognosis has been found to be poorer. Also termed shift out of proportion.
What is the definition of “early” vs. “late” surgery?
• Early: within 4 hours of injury
• Late: after 4 hours of injury
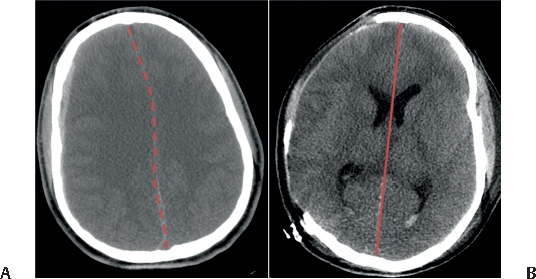
Fig. 56.5 (A) Example of midline shift from small right subdural hematoma. Basal cisterns were also compressed. (B) Correction of edema and midline shift after decompressive craniectomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






