Traumatic Spinal Column and Spinal Cord Injury: Special Considerations in Ankylosing Spondylitis
Bradley W. Jacobs
Michael G. Fehlings
Ankylosing spondylitis (AS) is a chronic inflammatory enthesopathy that primarily affects the axial skeleton. The AS pathologic process promotes extensive remodeling and weakening of the vertebral column. Accordingly, individuals with AS are at an increased risk of spinal column and spinal cord injury (SCI). Given the unique pathophysiologic repercussions of this disease entity, there are multiple special clinical considerations that, if recognized, can maximize successful clinical outcomes following spinal column and/or cord injury in this complex patient population.
OVERVIEW OF ANKYLOSING SPONDYLITIS
AS preferentially affects the vertebral column and sacroiliac joints and is the major subtype of a group of seronegative rheumatic spondyloarthritides that also includes psoriatic spondyloarthritis, reactive spondyloarthritis, spondyloarthritis associated with inflammatory bowel disease, and undifferentiated spondyloarthritis (1). The seronegative spondyloarthropathies have a genetic predisposition related to the major histocompatibility complex class I molecule HLA-B27. Ninety percent to ninety-five percent of AS patients are HLA-B27 positive, but only 5% of HLA-B27 positive individuals develop AS (2,3). This suggests that other, as yet unidentified, genetic and environmental factors also play a significant role in the pathogenesis of AS.
The incidence of AS is between 0.5 and 14 per 100,000 people per year, while the disease prevalence is between 0.1% and 1.4% (4). The majority of AS patients are male, with male to female ratios varying among different populations from 2:1 to upwards of 10:1 (5,6). The age of onset is less than 30 years in 80% of sufferers (5). AS is a chronic, lifelong condition in which disease progression is most frequently one of slow but continuous symptomatic worsening. Due to this temporal pattern, significant complications, such as spinal fractures, are not usually manifested until much later in life.
The diagnosis of AS is made on the basis of both radiographic and clinical criteria known as the Modified New York criteria (7) (Table 49.1). Central to the diagnosis is the presence of sacroiliitis, as defined by radiography or MRI. The degree of sacroiliitis is graded from 0 to 4, with the grade corresponding to radiographically normal joints, suspicious changes, minor changes, moderate changes, and ankylosis, respectively. The major clinical feature of AS is the presence of inflammatory back pain, as defined by Rudwaleit et al. (8). Using a controlled study, this group developed diagnostic criteria to help delineate inflammatory back pain, as found in AS and other spondyloarthritides, from other types of back pain. Ultimately, Rudwaleit et al. found that fulfillment of any two of the four criteria—(a) morning stiffness greater than 30 minutes, (b) improvement of back pain with activity but not with rest, (c) awakening due to back pain during the second half of the night, and (d) alternating buttock pain— suggested a diagnosis of inflammatory back pain with a sensitivity of 70% and a specificity of 81%.
In addition to inflammation in the axial skeleton, AS can also result in peripheral arthritis and enthesitis, as well as anterior uveitis. Manifestations in other organ systems, such as the pulmonary, cardiovascular, or renal systems, are rare, but do occur, and when present can have significant repercussions on the baseline health status of the AS patient and significantly complicate their care in the setting of traumatic spinal column and/or SCI.
VERTEBRAL COLUMN REMODELING IN ANKYLOSING SPONDYLITIS
The two central features of AS that promote the pathologic remodeling of the vertebral column are inflammation and new bone formation. The inflammation of AS is
characterized by an enthesopathy, or inflammation of ligamentous insertion points, throughout the axial skeleton. This inflammatory process promotes ectopic bone formation, or syndesmophytes, within the affected ligaments. The widespread enthesopathy of chronic AS thus results in ossification of the ligaments of the spinal column, as well as within the intervertebral disks, end plates, and apophyseal structures. These extensive syndesmophytes ultimately span the ossified nucleus pulposus at each intervertebral disk level. In addition to this extensive syndesmophytosis, significant vertebral body remodeling also occurs through the disease process. Square vertebral bodies form as a result of chronic spondylitis with destruction and rebuilding of their cortex and spongiosa (9). Accordingly, advanced AS, through the combination of universal syndesmophytosis and chronic spondylitis, results in the formation of the characteristic hyperkyphotic “bamboo spine.”
characterized by an enthesopathy, or inflammation of ligamentous insertion points, throughout the axial skeleton. This inflammatory process promotes ectopic bone formation, or syndesmophytes, within the affected ligaments. The widespread enthesopathy of chronic AS thus results in ossification of the ligaments of the spinal column, as well as within the intervertebral disks, end plates, and apophyseal structures. These extensive syndesmophytes ultimately span the ossified nucleus pulposus at each intervertebral disk level. In addition to this extensive syndesmophytosis, significant vertebral body remodeling also occurs through the disease process. Square vertebral bodies form as a result of chronic spondylitis with destruction and rebuilding of their cortex and spongiosa (9). Accordingly, advanced AS, through the combination of universal syndesmophytosis and chronic spondylitis, results in the formation of the characteristic hyperkyphotic “bamboo spine.”
TABLE 49.1 Modified New York Criteria for AS | |||||
|---|---|---|---|---|---|
|
While new bone formation is central to the pathogenesis of AS, AS patients also have osteoporosis and low bone mineral density (10, 11 and 12). This seemingly paradoxical finding is attributed to an uncoupling of the bone formation and bone resorption processes. Therefore, while ectopic bone formation occurs within the inflamed vertebral enthesis, bone resorption, through increased osteoclast activity, also occurs at a significantly increased and unregulated rate within the vertebra. This process promotes the weakening of the spinal column (11), and thus sets the stage for an increased risk of spinal column injury (Fig. 49.1).
ANKYLOSING SPONDYLITIS INCREASES VERTEBRAL FRACTURE RISK
As the spine of the AS patient fuses through ligamentous ossification and syndesmophytosis, a rigid hyperkyphotic deformity develops. Biomechanically, the fused and rigid spine is more akin to a long bone and thus acts as a rigid lever arm that is incapable of appropriately dissipating the energy of a traumatic event. These aberrant spinal biomechanics, combined with the brittle quality of the osteoporotic bone in AS patients, greatly increases the susceptible to vertebral column fractures, even following minor, often trivial, trauma (13, 14, 15 and 16).
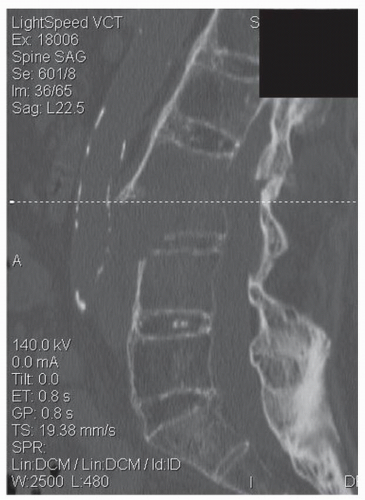 Figure 49.1. Sagittal CT reformat of a lumbar spine fracture sustained in a patient with AS following a fall from standing height. Note the severe vertebral osteoporosis. |
To further increase their susceptibility to spinal fractures, the majority of AS patients have significantly impaired mobility directly related to their rigid, kyphotic spinal deformity, combined with a variable degree of peripheral joint arthritis. These factors increase gait unsteadiness and thus increase susceptibility to falls. Westerveld et al. (17), in their extensive review of spinal fractures in the setting of AS, noted that 66% of injuries occurred following lowenergy traumatic events such as a fall from sitting or standing. This is further supported in multiple other case series of AS vertebral fractures, where falls are almost invariably the most common mechanism (13, 14, 15 and 16,18,19).
Multiple studies have investigated the risk factors that are associated with vertebral fractures in the AS population (reviewed by Geusens et al. (11)). Identified factors include gender (men more than women), age, low body mass index, osteoporosis, disease duration, degree of syndesmophyte formation, peripheral joint involvement, increased spinal movement restriction, and increased occiput-to-wall distance (as a surrogate measure of kyphosis). Cooper et al. (16), in a population-based analysis of vertebral fractures in AS patients found an odds ratio of 7.7 for clinically significant vertebral column fractures in direct comparison to the general population. They
further noted that the cumulative incidence of vertebral fractures appears to peak at 17% in the third decade after diagnosis (16).
further noted that the cumulative incidence of vertebral fractures appears to peak at 17% in the third decade after diagnosis (16).
VERTEBRAL FRACTURE PATTERNS IN AS
The majority of AS fractures are located in the cervical spine, with a proportion approaching 80% in one large review (17). In direct comparison, a detailed populationbased analysis has previously shown that, in general, cervical spine fractures account for only about 20% of all spinal column fractures (20). Hyperextension is the most frequently observed mechanism of injury in series of AS vertebral fractures (14,21, 22, 23 and 24), although one series did note that flexion momentum arms predominated in their cohort (13). This prevalence of hyperextension injuries likely reflects the vulnerability of AS patients to forward falls secondary to their progressive kyphotic angulation, and an inability to properly visualize the ground ahead while walking.
Specific vertebral fracture patterns are also altered in AS patients. Because of the extensive ankylosis, fractures often extend through the disk space and involve both the anterior and posterior elements of the vertebra. In addition, the extensively ossified ligaments of the AS spine also fracture as part of the injury pattern, further decreasing the structural support available for the spinal column and dramatically increasing the instability of vertebral fractures in the setting of AS. This lack of ligamentous support often leads to osseous injuries with a high degree of distraction across the fracture fragment (Fig. 49.2), increasing risks to adjacent neural elements as well as increasing the attendant difficulty of fracture reduction.
As discussed previously, secondary to extensive ankylosis, the fractured spine of an individual with AS takes on biomechanical properties more akin to that of a long bone. Thus, given the long lever arm that exists on either side of the AS vertebral fracture, multiple segments of fixation (often three segments) are mandatory both above and below the fracture to ensure the necessary postarthrodesis stability that is required to promote fracture healing and eventual fusion (Fig. 49.3).
ANKYLOSING SPONDYLITIS AND SPINAL CORD INJURY: INCIDENCE AND ETIOLOGY
Retrospective case series of SCI in AS patients suggest that 1.5% to 2.0% of SCI patients have AS (13,14,24), a prevalence that is much higher than the prevalence of AS in the general population. Alaranta et al. (14), using Finnish national prevalence data, more recently determined that the incidence of SCI in AS patients was 11.4 times greater than for the population at large. In line with the higher proportion of cervical fractures in the AS population, a higher incidence of cervical SCI is also noted in the AS population, accounting for up to 84% of all cord injuries (14), in comparison to a 55% incidence of cervical SCI in the general population (25). The incidence of complete SCI also appears to be higher in patients with AS (14,21,23,24,26) than in the general population. Furthermore, AS patients who sustain an SCI are older than the general population of SCI patients, with a mean age from 55 to 61 years in various series (13,14,24,27) compared with a mean age of 37 for the SCI population at large (28).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







