Chapter 6 Upper Extremity Peripheral Nerve Blockade
 Upper extremity blockade may be performed for therapeutic, diagnostic, prophylactic, and prognostic indications.
Upper extremity blockade may be performed for therapeutic, diagnostic, prophylactic, and prognostic indications. Ultrasound-based techniques result in faster onset, shorter procedure time, higher success rates, longer block duration, and fewer vascular punctures than alternative techniques.
Ultrasound-based techniques result in faster onset, shorter procedure time, higher success rates, longer block duration, and fewer vascular punctures than alternative techniques. Foreknowledge of brachial plexus anatomy and desired site of action is critical to selection of appropriate location of brachial plexus blockade.
Foreknowledge of brachial plexus anatomy and desired site of action is critical to selection of appropriate location of brachial plexus blockade. In ultrasound-guided techniques, the deepest and most distal structures from the needle insertion site should be blocked first.
In ultrasound-guided techniques, the deepest and most distal structures from the needle insertion site should be blocked first. Failure to evoke a motor response during nerve stimulation may occur despite needle-to-nerve contact.
Failure to evoke a motor response during nerve stimulation may occur despite needle-to-nerve contact.Introduction
Upper extremity peripheral nerve blockade, in one form or another, has been performed since ancient Egypt as evidenced by 5000-year-old pictographs illustrating nerve compression anesthesia for hand surgery.1 Today, the development of image-guidance technology and efficacious injectable drugs have made upper extremity peripheral nerve blockade an increasingly useful tool in pain physicians’ and regional anesthesiologists’ diagnostic and therapeutic arsenal. Peripheral nerve blockade is a growing and dynamic field with diverse approaches, technological equipment, and a variety of local anesthetics and adjuvant therapies.
Brachial Plexus Anatomy
Familiarity with brachial plexus anatomy is critical to optimal and safe performance of peripheral nerve techniques. The most proximal portion of the brachial plexus is located in the posterior triangle of the neck, bordered by the clavicle inferiorly, the trapezius muscle posteriorly, and the sternocleidomastoid muscle anteriorly. There, the plexus is deep to the skin, subcutaneous tissue, deep fascia, and platysma muscle and is formed by the union of the anterior (ventral) primary rami of cervical nerves five through eight (C5-C8) and the greater part of the first thoracic nerve (T1). In some patients, the fourth cervical (C4) and second thoracic (T2) nerves also contribute to the brachial plexus. At its most proximal, the C5-T1 nerve roots conjoin to form the superior (C5-C6), middle (C7), and inferior trunks (C8-T1) (Fig. 6-1).
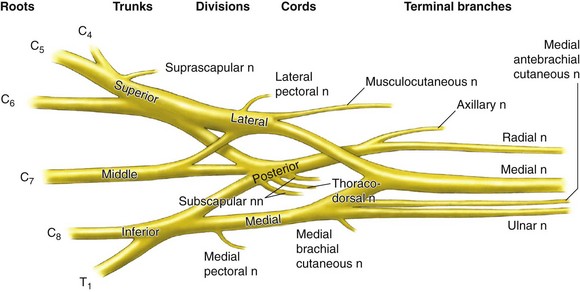
Fig. 6-1 Brachial plexus anatomy.
(Reprinted with permission from Torsher L, Smith H, Jacob A: Interscalene blockade. In Hebl JR, Lennon RL, editors: Mayo Clinic atlas of regional anesthesia and ultrasound-guided nerve blockade, New York, 2010, Oxford University Press, p 192.)
A superficial landmark, the interscalene groove, overlies the trunks and is palpable as an indentation between the anterior and middle scalene muscles. This groove, at the level of the cricoid cartilage, is the needle entry site used most frequently for interscalene brachial plexus blockade. The phrenic nerve, derived from the C3-C5 nerve roots, runs parallel to the vertebral artery at this location as it passes through the neck on the ventral surface of the anterior scalene muscle. Sonographic study has revealed that the phrenic nerve is visible as a hypoechoic structure in 93% of subjects.2 The phrenic nerve is immediately adjacent to the superior trunk at the C6 level, thus explaining the uniform deactivation of this nerve during interscalene blockade.3
As the three trunks descend toward the first rib, the brachial plexus differentiates into anterior and posterior divisions, corresponding to the ventral and dorsal aspects of the upper extremity. Located posterolateral to the subclavian artery, the divisions pass below the middle third of the clavicle and above the first rib before fusing into medial, lateral, and posterior cords. Approaches to the brachial plexus immediately above and below the clavicle are the so-named supraclavicular and infraclavicular blocks. At the lateral border of the pectoralis minor muscle, the axillary artery is surrounded by the lateral, posterior, and medial cords of the brachial plexus. As the cords enter the axilla, they give rise to the sensorimotor branches of the plexus, the radial, median, ulnar, and musculocutaneous nerves. These peripheral nerves consist of individual myelinated nerve fibers embedded within an endoneurial connective tissue layer and grouped into discrete bundles or fascicles. Nerve fascicles are interlaced by connective tissue and surrounded by an outer epineurial membrane.4
Indications and Contraindications
Because several nerves join or diverge from the brachial plexus between its central origins and its most distal peripheral branches, no single location suffices to produce complete blockade of the upper extremity. Thus, proximal block locations are selected based on foreknowledge of the current or future pain distribution. Table 6-1 lists the more common indications and techniques for blockade of various elements of the brachial plexus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree











