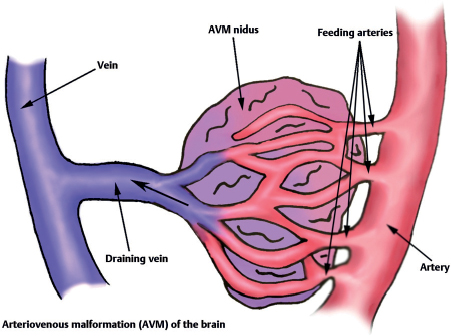
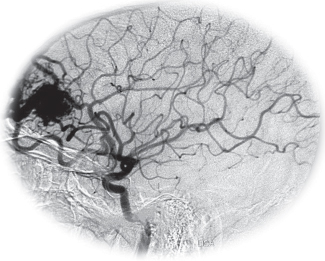
54 What is an arteriovenous malformation (AVM)? A congenital lesion featuring dilated arteries flowing abnormally into dilated veins without intervening capillary beds or neural parenchyma Fig. 54.1 Arteriovenous malformation (AVM) of the brain. What is the risk of AVM hemorrhage per year? What is the risk of AVM bleed ing (at least once) over one’s lifetime? Lifetime risk (%) = 105 – the patient’s age in years (assuming approximately a 2 to 4%/year bleed rate)7 Which AVMs are more likely to bleed? • AVMs with deep venous drainage7 • AVMs with an intranidal aneurysm7,10 • Periventricular AVMs11 • AVMs with impaired venous drainage12 What is the morbidity and mortality associated with AVM hemorrhage? 10% mortality and 30 to 50% morbidity associated with each bleed13 How do AVMs appear on MRI? “Bag of black worms” (due to flow voids) What is the angiographic hallmark? Early draining vein, sometimes (2.7 to 16.7%)14 with an aneurysm on the feeding vessel. Some AVMs may be angiographically occult (known as “cryptic AVMs”) due to occlusion of the feeding vessel. Fig. 54.2 Left carotid injection revealing frontal AVM with arterial supply from ACA and MCA and early filling of sagittal sinus with prominent draining vein. Which syndromes should be considered in patients presenting with multiple AVMs? Wyburn-Mason (aka Bonnet-Dechaume-Blanc) syndrome: a sporadic, congenital syndrome associated with multiple ipsilateral AVMs in the centro- or hemifacial area with oculo-orbital and cerebral involvement, often with AVMs of the retina, maxilla, mandible, midbrain, and anterior visual pathway Rendu-Osler-Weber (ROW) syndrome (aka hereditary hemorrhagic telangiectasia): an autosomal dominant trait resulting in multiple small AVMs of the skin, lungs, mucous membranes, GI and GU tracts, and CNS How are cerebral AVMs classified according to risk of surgical resection? Spetzler-Martin grading system,15 from 1 to 5 points (higher score = worse outcome of surgical resection) Describe the Spetzler-Martin grading system.
Vascular Malformations
Factor | Pattern | Points |
| < 3 cm | 1 |
Size | 3–6 cm | 2 |
| > 6 cm | 3 |
Brain eloquence | Eloquent | 1 |
| Non-eloquent | 0 |
Venous drainage | Superficial only | 0 |
| Deep | 1 |
What tools exist for treatment of AVMs?
• Surgical excision
• Stereotactic radiosurgery
• Endovascular embolization (typically inadequate when used alone; facilitates surgical excision or stereotactic radiosurgery)
How do AVMs typically present?
• Hemorrhage (most common)16,17
• Seizures
• Increased ICP
• Ischemia (steal phenomenon)
• Mass effect and resultant neurological deficit
• Incidental
What is the annual risk of rebleeding for AVMs presenting with hemorrhage?
6% in first year, then 3 to 4% per year3–5
Which factors increase the risk of bleeding?
Pregnancy, hypertension, age 15 to 20 years13,18
What are some of the basic technical principles for surgical excision of AVMs?
• Obtain a wide excision
• Occlude feeding arteries before veins
• Spare vessels uninvolved in the AVM (vessels of passage)
• Clip aneurysms on feeding arteries if possible
• Maintain flow through the draining vein until after the nidus is completely excised
What is the morbidity and mortality associated with surgical excision of AVMs?
Dependent on Spetzler-Martin grade: morbidity 7.8 to 9.7%, mortality 1.3%17,19
What is “normal perfusion pressure breakthrough”?
One of the proposed causes of delayed postoperative deterioration after surgical excision of AVMs. Thought to be due to failure of autoregulation in chronically dilated vessels of ischemic regions of brain. The increase in global perfusion pressure to normal levels after resection of AVMs is thought to result in repressurization of previously hypotensive regions and cerebral hyperemia, swelling, or hemorrhage.20
When is radiosurgery an option?
• Small (<2.5- to 3-cm nidus), deep or inaccessible AVMs
• Between 1 and 3 years are required to obliterate the lesion (during which period the risk of hemorrhage still exists and may be relatively increased)21–24
How effective is radiosurgery in the treatment of AVMs?
80 to 90% of small lesions (<2-cm nidus) and 40 to 60% of larger lesions are occluded within 2 years21
What are the risks associated with endovascular embolization of AVMs?
• Transient or mild neurological deficit (4.8 to 14%)25,26
• Hemorrhage
• Seizure
• Serious neurological deficit or death (1 to 2%)25,27
Which AVMs tend to present with occipital bruit and pulsatile tinnitus?
Dural AVMs. They typically drain to the transversesigmoid sinus junction. The occipital artery is typically the dominant feeder of the AVM.
Dural AVMs are classically seen in what patient population?
Females in their 40s. Female preponderance28 (as opposed to spinal dural AVMs, which show a male preponderance).29 Most patients are in their 40s or 50s at diagnosis30,31 (as opposed to intraparenchymal AVMs, which are most often diagnosed in ages 20 to 40.5
What is the diagnostic test of choice for dural AVMs?
Cerebral angiography (MRI will not typically detect dural AVMs)
Where are dural AVMs most commonly located?
Adjacent to the transverse sinus with the epicenter at the junctions of transverse and sigmoid sinuses (20–60%) or in the cavernous sinus (20–40%).30,32
How are dural AVMs classified?
Cognard et al30 classification system based on angiographic findings:
Type I: normal anterograde flow into sinus (benign lesions)
Type IIa: retrograde flow into sinus
Type IIb: retrograde flow into cortical veins (10% will hemorrhage)
Type IIa+b: retrograde flow into sinus and cortical veins
Type III: direct cortical venous drainage without venous ectasia (40% will hemorrhage)
Type IV: direct cortical venous drainage with venous ectasia (65% will hemorrhage)
Type V: Types I to IV with the addition of spinal venous drainage
Borden classification system based on venous drainage33:
Type I: dural arterial supply drains anterograde into venous sinus
Type II: similar to type I, but high pressure within the sinus results in additional retrograde drainage into subarachnoid veins
Type III: dural arterial supply drains retrograde into subarachnoid veins
What factor associated with dural AVMs is critical in predicting the risk of future hemorrhage and need for treatment?
Cortical venous drainage
How are spinal AVMs classified?31,34–37
Type I: dural spinal AVM, low-flow (most common type, fed by radicular arteries)
Type II (aka spinal glomus AVM): intraparenchymal, high flow (fed by medullary arteries)
Type III (aka juvenile spinal AVM): intraparenchymal, high flow (an enlarged form of type II that invades the entire cross section of the cord as well as the vertebral body)
Type IV (aka spinal AV fistula): perimedullary (often fed by the artery of Adamkiewicz and the anterior spinal artery)
What are some of the common presentations for spinal AVMs?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






