Chapter 39 Ventral and Ventrolateral Subaxial Decompression
General Considerations
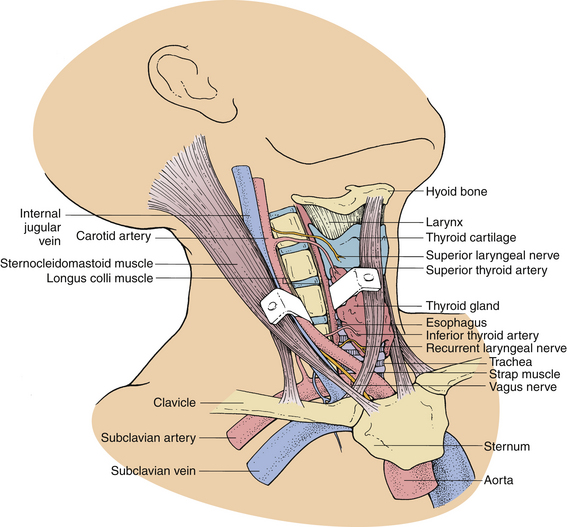
The ventral approach to the cervical spine is performed through a plane between the sternocleidomastoid muscle and the carotid sheath laterally and the strap muscles and tracheoesophageal viscera medially. This approach is appropriate for ventral cervical discectomy, vertebrectomy, fusion, and instrumentation (Fig. 39-1).
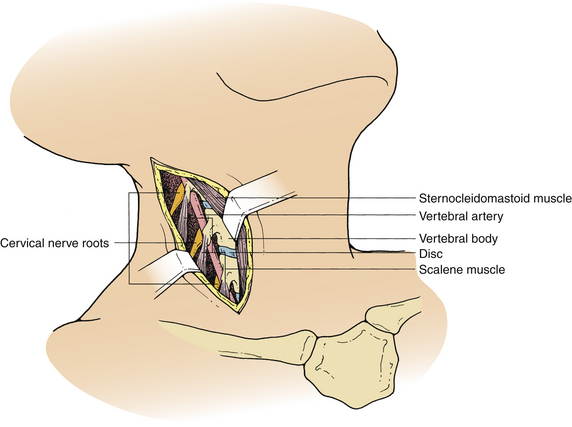
The ventrolateral approach, however, is more suitable for decompression of the vertebral artery in the transverse foramen or between the foramina or spinal nerve roots outside the spinal canal. Two different techniques are described in the literature. Verbiest’s1 technique is performed through the same plane as the ventral approach. However, further exposure is performed lateral to the longus colli muscle on the ipsilateral side. This exposure allows visualization of the costotransverse lamella, which forms the roof of the foramen transversarium covering the vertebral artery. Hodgson,2 on the other hand, approached the cervical spine lateral to the sternocleidomastoid muscle and the carotid sheath. These structures, along with the musculovisceral column, are retracted medially (Fig. 39-2). The remainder of the exposure is similar to that described by Verbiest, with the exception that the longus colli muscles are retracted medially to laterally to gain access to the vertebral artery.
Specific Complications, Avoidance, and Management
Preoperative Period
Intraoperative evoked potential monitoring can be used to identify and avoid dangerous manipulation of the neural tissue during surgery.3 However, there is currently no convincing evidence that the use of this modality improves outcome after decompressive surgery. Somatosensory evoked potentials (SSEP) are most commonly used for this purpose. However, this type of monitoring may be associated with false-positive intraoperative SSEP changes, thus creating significant anxiety for the surgeon and possibly unnecessary anesthetic and surgical maneuvers. Motor evoked potential monitoring reflects the function of the ventral spinal cord tracts more reliably than does SSEP monitoring and may avoid some of the false-positive intraoperative changes observed with SSEP.
Intraoperative Period
The risk is probably balanced by the convenience of the position for right-handed surgeons. A left-sided approach, on the other hand, carries the risk of injury to the thoracic duct during exposure of the lower cervical spine. A recent review of 328 patients who underwent ventral cervical spine fusion procedures showed no association between the side of the approach and the incidence of RLN symptoms.4
Injury to the Esophagus and Pharynx
Dysphagia is a common problem after ventral cervical surgery and is usually secondary to edema from retraction. This symptom usually resolves within a few days without any treatment. In certain cases, however, it may persist as long as several weeks; rarely, it may be permanent. It is more common in elderly patients and in those who had extensive mobilization of the upper esophagus or hypopharynx. In a questionnaire mailed to 497 patients who had undergone ventral cervical fusion procedures, 60% reported some dysphagia after the surgical procedure compared to 23% in the control group.5
Esophageal or pharyngeal lacerations can occur, especially in the upper cervical region where the hypopharynx is thinner, either from sharp dissection or from the teeth of self-retaining retractors. If esophageal perforation is recognized intraoperatively, it should be repaired primarily. The wound should be drained and the patient placed on nasogastric drainage for at least 7 to 10 days. Fusion in these circumstances is contraindicated. Subsequently, a swallow study with a water-soluble contrast agent should be obtained to confirm that the perforation has sealed. In the majority of cases, the injury to the esophagus is not recognized during surgery and shows symptoms later as a local infection, fistula, sepsis, or mediastinitis.6,7 The presence of crepitus or an enlarging mass in the neck or mediastinal air on a chest radiograph usually suggests the strong possibility of an esophageal perforation. Diagnosis can be confirmed with an esophagogram. However, this test may not always be positive when esophageal injury is present. Esophagoscopy or a postesophagogram CT scan may also demonstrate a perforation. Treatment of a delayed perforation consists of nasogastric drainage, antibiotics, and reexploration of the incision. If a defect is found, it should be repaired and a wound drain placed.6 To avoid this complication, the longus colli muscles should be freed enough rostrally, caudally, and laterally so that the sharp teeth of the self-retaining retractors can be placed safely under them without risk of dislodgement during the procedure (Fig. 39-3). In addition, the esophagus and other soft tissue structures should be hidden by the retractors to avoid injury by the high-speed drill during bone removal.
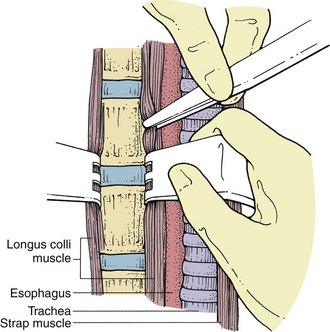
FIGURE 39-3 Placement of self-retaining retractors under the longus colli muscle to prevent dislodgement during surgery.
Occasionally, perforation of the esophagus can result from a displaced graft.8 To avoid this problem, some surgeons recommend reapproximation of the longus colli muscles over the graft. When a displaced graft perforates the esophagus, reexploration is required. Either replacement or removal of the graft may be indicated, depending on the need for the graft to maintain stability. The esophageal perforation should be repaired, if possible, and the patient treated with antibiotics and nasogastric drainage.
Injury to the Laryngeal Nerves
The superior laryngeal nerve is a branch of the inferior ganglion of the vagus nerve and innervates the cricothyroid muscle. The superior thyroid artery, encountered above C4, is an important anatomic landmark for the superior laryngeal nerve. Damage to this nerve may result in hoarseness, but it often produces symptoms such as easy voice fatigue.9 To avoid injury to this nerve, one should be aware of its anatomic location.
On the left side, the inferior (recurrent) laryngeal nerve loops under the arch of the aorta and is protected in the left tracheoesophageal groove. On the right side, however, the RLN travels around the subclavian artery, passing dorsomedially to the side of the trachea and esophagus. It is vulnerable as it passes from the subclavian artery to the right tracheoesophageal groove. The inferior thyroid artery on the right side is an anatomic marker for the RLN. The nerve usually enters the tracheoesophageal groove, the point at which the inferior thyroid artery enters the lower pole of the thyroid. Damage to the RLN may result in hoarseness, vocal breathiness or fatigue, weak cough, dysphagia, or aspiration.10
Preoperative insertion of a nasogastric tube not only allows easier identification of the esophagus for protection against an esophageal injury, but also allows localization of the tracheoesophageal groove and the avoidance of the plane. Endotracheal tube-related RLN injury has also been cited. Monitoring of the endotracheal cuff pressure and its release after retractor placement decreased the rate of RLN temporary paralysis from 6.4% to 1.7% in one series.11
One should also be aware of the anatomic variations, especially on the right side, where the RLN may be nonrecurrent. However, the frequency of this aberration is well below 1%.12 In this situation, the RLN travels directly from the vagus nerve and the carotid sheath to the larynx. If a suspected nonrecurrent nerve is encountered, it may be identified with a nerve stimulator and laryngoscopic examination of the vocal cords. If it cannot be retracted safely, it is best to abandon the procedure and use a left-sided approach.
The true incidence of RLN injury is difficult to determine but is probably about 1% to 2%.4,13 Beutler et al.4 reported that the incidence of RLN symptoms was 2.1% with anterior cervical discectomy, 3.5% with corpectomy, 3% with instrumentation, and 9.5% with reoperative anterior surgery.
Because many patients have some degree of voice change after ventral cervical operations, a thorough investigation is not required in most cases. However, a laryngoscopic examination should be performed in persistent cases. If RLN palsy is present, the vocal cord will be faced in the paramedian position. Immediate treatment is not usually required for a paralyzed vocal cord because, in most instances, the nerve has not been severed, and the condition will resolve with time.13 In some patients, hoarseness or voice dysfunction may be minimal, not requiring treatment. However, patients with persistent hoarseness after several months can be treated with injections of hemostatic gelatin (Gelfoam) or Teflon into the vocal cord. Gelfoam produces a temporary improvement and may be used as an interim measure pending spontaneous return of function. Teflon injection is a permanent treatment modality that is used in patients in whom no recovery is expected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree