Vertebral Artery Injury
Alan H. Daniels
Daniel K. Riew
Robert A. Hart
Iatrogenic vertebral artery (VA) injury is an uncommon but potentially serious complication of cervical spine surgery. When VA injury occurs, consequences such as pseudoaneurysm, arteriovenous fistula, hemorrhage, thrombosis, embolic stroke, and even death may arise. A thorough knowledge of the neurovascular and bony anatomy of the cervical spine is fundamental in preventing this complication and managing VA injury when it does occur.
VERTEBRAL ARTERY ANATOMY AND ANATOMIC VARIABILITY
The VAs are the first branches arising from the subclavian arteries. They are classically divided into four segments, V1-V4. The first segment (V1) typically extends from its origin at the subclavian artery to the C6 foramen transversarium, running ventral to the C7 transverse process. The second segment (V2) extends within the foramen transversaria from C6 to C1. The third segment (V3) extends from the atlas to the foramen magnum. The fourth segment (V4) extends intradurally from the foramen magnum, providing flow to the posterior inferior cerebellar artery (PICA). It then joins the contralateral VA to form the basilar artery, which provides flow to the posterior circulation of the brain (1).
The foramen transversaria are formed by vestigial costal elements that fuse to the vertebral body, enclosing the VA, venous plexus, and a sympathetic nervous plexus (2). The left foramina are generally larger than the corresponding right foramina (1). In some individuals, the foramina are duplicate (1.3%), triplicate, or absent (<1%) (2).
Relative to the medial margin of the longus colli muscle and the ventral margin of the vertebral body, the VA is more lateral and ventral at C6 and more medial and dorsal at C3 (3). The distance between the medial margins of the foramen transversaria ranges from 31.2 to 25 mm from C7 to C3, respectively (4). The distance from the medial margin of the uncovertebral joint to the transverse foramen averages 5.5 mm in the subaxial vertebrae, although anatomic variants are common. Curylo et al. (5) reported a 2.7% incidence of unilateral VA location of less than 1.5 mm lateral to the uncovertebral joint. In some cases, transverse foramen enlargement can extend as far medial as the midvertebral body level, with a tortuous VA causing erosion of the vertebral body or pedicle (5).
There is also significant anatomic variability of the course and anatomy of the VAs at the atlantoaxial level. Tokuda et al. (6) reported atlantoaxial arterial anomalies in 2.3% of 300 patients, including duplication of the VA as well as the VA running in the spinal canal below C1. Occasionally, the VA may not pass through the C1 foramen transversarium, but ventral to it.
Madawi et al. (7) reported a 20% incidence of positioning of the VA at the atlantoaxial level in a groove in the inferior surface of the C2 lateral mass, preventing safe passage of a transarticular screw. Similarly, Paramore et al. (8) reported that 18% to 23% of patients may not be candidates for dorsal C1-C2 transarticular screw fixation on at least one side due to a high-riding C2 transverse foramen.
At the level of C1, the VA curves dorsomedially, traveling dorsal to the lateral mass and cranial to the dorsal arch of C1. On the upper surface of the C1 lamina is a groove for the VA. In up to 15% of patients, an ossific structure known as the ponticulus posticus (“little bridge”) overlies this groove for the VA, creating an arcuate foramen (Fig. 112.1).
In patients with rheumatoid arthritis, vertebral subluxation and destruction of the articular surfaces can alter the anatomical relationships in the cervical spine, resulting in increased risk of injury to the VA (7). Tumor, trauma, infection, and prior surgery can also significantly alter the bony and arterial anatomy in the cervical spine. Close inspection of preoperative imaging and consideration of obtaining injection or magnetic resonance angiography (MRA) should be undertaken in such cases.
CLINICAL IMPACT OF VERTEBRAL ARTERY INJURY
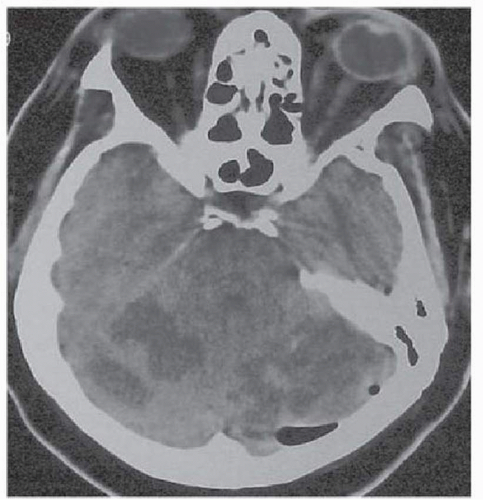
Complications of VA injury can occur intraoperatively, in the immediate postoperative period, or even years after the initial injury. Intraoperative complications include VA laceration and blood loss, as well as arterial thrombotic or embolic event, which can cause intracranial ischemia. Postoperative complications include pseudoaneurysm, embolic stroke, arteriovenous fistula, and the possibility of delayed hemorrhage if definitive control of the injury has not been obtained (10, 11, 12 and 13). Death can occur secondarily to VA injury in the intraoperative, immediate postoperative, or late postoperative periods (Fig. 112.2).
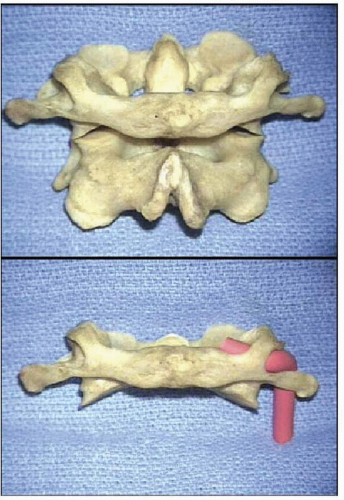 Figure 112.1. Anteroposterior views of osseous specimens of C1 and C2 demonstrating a ponticulus posticus bilaterally (top) and revealing the VA coursing medially within the arcuate foramen and deep to the ponticulus posticus (bottom). Ref. (9). (From Young JP, Young PH, Ackermann MJ, et al. The ponticulus posticus: implications for screw insertion into the first cervical lateral mass. J Bone Joint Surg Am 2005;87:2495-2498.) |
When a unilateral VA injury occurs, the hindbrain is at risk of ischemia if the contralateral VA is hypoplastic or terminates in the PICA. Loss of blood flow in the PICA distribution not compensated by the contralateral VA will lead to development of a lateral medullary infarction (2). In this case, Wallenberg’s syndrome may ensue, consisting of a constellation of some or all of the following symptoms: decreased sensation of the ipsilateral face and contralateral limb, ipsilateral limb ataxia, facial pain, swallowing problems, slurred speech, nystagmus, autonomic and respiratory dysfunction, and ipsilateral Horner’s syndrome consisting of ptosis, miosis, and anhidrosis due to lesions in the descending sympathetic nervous system (2).
VERTEBRAL ARTERY INJURY IN VENTRAL CERVICAL SPINE SURGERY
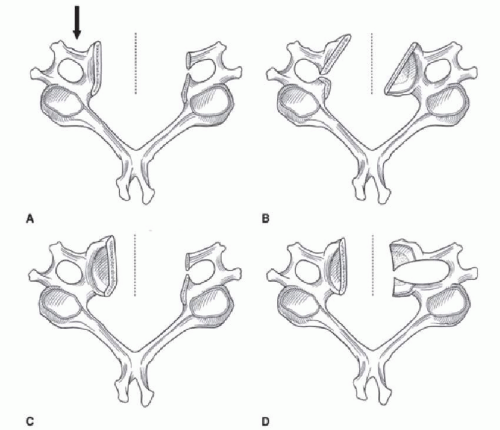
The reported incidence of intraoperative VA injury during ventral cervical spine surgery ranges from 0.2% to 0.5% (10,14,15). Surgical factors that can contribute to VA injury include performance of an excessively wide corpectomy, loss of the vertebral midline or orientation leading to an off-center or oblique corpectomy, unrecognized VA tortuosity or other anomalies such as a VA located ventral to the transverse process, and abnormal softening of the lateral bone due to infection or tumor (Fig. 112.3) (11).
The longus colli muscle is a valuable anatomic landmark in identifying intraoperative midline orientation (Fig. 112.4) (4,16). As the diskectomy or corpectomy progresses, the uncovertebral joint becomes the anatomic landmark to guide the limit of the lateral decompression. Lateral decompression as far as to the medial uncovertebral joint is generally safe, although the relation of the foramina transversaria to the uncovertebral joint should always be verified on preoperative imaging. In patients with foraminal stenosis, the surgeon may undercut the uncovertebral joint with a 1- or 2-mm Kerrison rongeur but should not exceed 3 to 4 mm laterally and should not be performed with the burr.
Greater attention to the lateral extent of decompression in more cranial vertebra is warranted due to the reduced distance between the foramina transversaria compared to caudal levels. Another consideration caudally is the vertebral arteries’ path between the transverse process of C7 and the transverse foramen of C6; thus, avoidance of superficial lateral dissection at the C6-C7 level is advised (12).
AVOIDANCE OF VERTEBRAL ARTERY INJURY IN VENTRAL PROCEDURES
Preoperative computed tomography (CT) and/or magnetic resonance imaging (MRI) should be obtained and carefully reviewed prior to surgery, noting the VAs’ and transverse foramina’s relationship to the vertebral body
and central canal of the cervical spine. If abnormalities are noted, additional imaging studies such as CT angiography (CTA) or MRA may be appropriate, and the operative plan may be changed if arterial anatomy is prohibitive (Fig. 112.5) (5). In some cases, intraoperative measures such as VA exposure and retraction with vessel loops may be performed to decrease risk of intraoperative injury (12).
and central canal of the cervical spine. If abnormalities are noted, additional imaging studies such as CT angiography (CTA) or MRA may be appropriate, and the operative plan may be changed if arterial anatomy is prohibitive (Fig. 112.5) (5). In some cases, intraoperative measures such as VA exposure and retraction with vessel loops may be performed to decrease risk of intraoperative injury (12).
After surgical exposure, proper identification and retention of midline orientation is critical. During surgical exposure of the vertebrae, the longus colli muscle insertion sites provide midline orientation, although elevation and lateral retraction reduces their utility. Prior to retraction of the longus colli muscles, the surgeon can mark the ventral midline on the vertebral body with a marking pen or electrocautery to aid with orientation throughout the remainder of the procedure (2).
MANAGEMENT OF VERTEBRAL ARTERY INJURY DURING VENTRAL PROCEDURES
The principal goals in treating VA injury are the same whether they occur during a ventral or dorsal approach: to gain control of hemorrhage, to prevent acute central nervous system ischemia, and to prevent postoperative complications such as pseudoaneurysm, late-onset hemorrhage, and embolic events.
Intraoperatively, a VA injury should be suspected when pulsatile bright red blood flow is noted, although brisk dark blood flow may be encountered due to concurrent vertebral venous plexus injury. Intraoperative management of VA injury varies depending on the nature of the injury, the patient’s anatomy, and available resources. Options available for management include direct tamponade, microvascular repair or bypass, endovascular stenting or embolization, and artery ligation.
In the event of VA injury, the anesthesiologist should be informed of the need for fluid resuscitation and directed to maintain cerebral perfusion pressure to reduce the risk of dorsal circulation ischemia (12). Bleeding is initially controlled with direct tamponade while developing a plan and surgical team to accomplish more definitive control (14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree