21 Radial Neuropathy
Anatomy
The radial nerve receives innervation from all three trunks of the brachial plexus and, correspondingly, a contribution from each of the C5–T1 nerve roots (Figures 21–1 and 21–2). After each trunk divides into an anterior and posterior division, the posterior divisions from all three trunks unite to form the posterior cord. The posterior cord gives off the axillary, thoracodorsal, and subscapular nerves before becoming the radial nerve. In the high arm, the radial nerve first gives off the posterior cutaneous nerve of the arm, the lower lateral cutaneous nerve of the arm, and the posterior cutaneous nerve of the forearm (Figure 21–3), followed by muscular branches to the three heads of the triceps brachii (medial, long, and lateral) and the anconeus. The anconeus is a small muscle in the proximal forearm that effectively is an extension of the medial head of the triceps brachii. After giving off these muscular branches, the radial nerve wraps around the posterior humerus in the spiral groove. Descending into the region of the elbow, muscular branches are then given off to the brachioradialis and the long head of the extensor carpi radialis. Next, three to four cm distal to the lateral epicondyle, the radial nerve bifurcates into two separate nerves: one superficial and the other deep. The superficial branch, known as the superficial radial sensory nerve, descends distally into the forearm over the radial bone to supply sensation over the lateral dorsum of the hand as well as part of the thumb and the dorsal proximal phalanges of the index, middle, and ring fingers (Figure 21–4). Distally, the nerve is quite superficial, running over the extensor tendons to the thumb, where it can easily be palpated (Figure 21–5).

FIGURE 21–1 Anatomy of the radial nerve.
(Adapted with permission from Haymaker, W., Woodhall, B., 1953. Peripheral nerve injuries. WB Saunders, Philadelphia.)
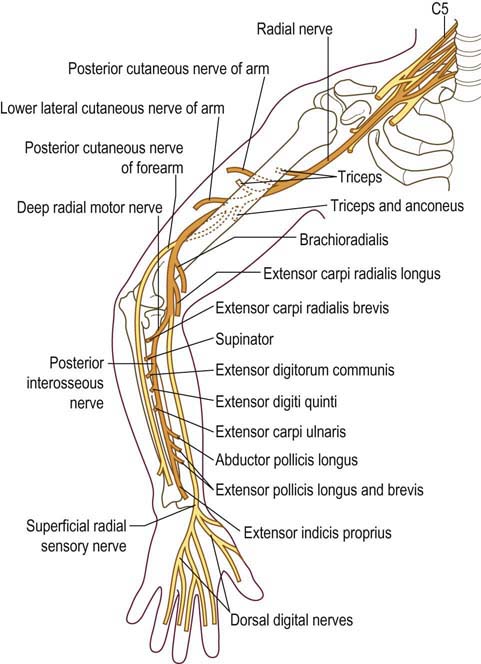
FIGURE 21–2 Anatomy of the radial nerve.
(Adapted with permission from Haymaker, W., Woodhall, B., 1953. Peripheral nerve injuries. WB Saunders, Philadelphia.)

FIGURE 21–3 Sensory territories supplied by the radial nerve.
(Adapted with permission from Haymaker, W., Woodhall, B., 1953. Peripheral nerve injuries. WB Saunders, Philadelphia.)
The deep branch, known as the deep radial motor branch, first supplies the extensor carpi radialis brevis and the supinator muscles before it enters the supinator muscle under the Arcade of Frohse (Figure 21–6). The Arcade of Frohse is the proximal border of the supinator and in some individuals is quite tendinous. After the nerve enters the supinator, it is known as the posterior interosseous nerve, which then supplies the remaining extensors of the wrist, thumb, and fingers (extensor digitorum communis, extensor carpi ulnaris, abductor pollicis longus, extensor indicis proprius [EIP], extensor pollicis longus, and extensor pollicis brevis). Although the posterior interosseous nerve is thought of as a pure motor nerve (supplying no cutaneous sensation), it does contain sensory fibers that supply deep sensation to the interosseous membrane and joints between the radial and ulna bones.

FIGURE 21–6 Anatomy of the radial nerve at the elbow.
(Adapted with permission from Wilbourn, A.J., 1992. Electrodiagnosis with entrapment neuropathies. AAEM plenary session I: entrapment neuropathies. Charleston, South Carolina.)
Nomenclature of the Branches of the Radial Nerve near the Elbow
One of the more confusing aspects of radial nerve anatomy is the inconsistency regarding the nomenclature of the branches of the radial nerve near the elbow used in various anatomic texts and clinical reports (Figure 21–7). The following points should help the electromyographer when dealing with potential lesions of the radial nerve in this area:

FIGURE 21–7 Anatomy and nomenclature of the radial nerve around the elbow.
(Adapted with permission from Thomas, S.J., Yakin, D.E., Parry, B.R., et al., 2000. The anatomical relationship between the posterior interosseous nerve and the supinator muscle. J Hand Surg Am 25 (5), 936–941.)
Radial Nerve between the Spiral Groove and the Bifurcation near the Elbow
• Distal to the spiral groove but before the elbow, the main radial nerve always supplies two muscles: the brachioradialis and the extensor carpi radialis longus (also known as the long head of the extensor carpi radialis).
• In some individuals, the main radial nerve will also supply a third muscle, the extensor carpi radialis brevis muscle*.
Deep Branch
• The deep radial motor branch first supplies the extensor carpi radialis brevis muscle in some individuals*.
• It then supplies one or more branches to the supinator muscle before entering the supinator muscle proper.
• The deep radial motor branch then runs under the Arcade of Frohse (the proximal border of the supinator) and through the supinator muscle.
• After leaving the supinator muscle, branches are given off that supply the extensor muscles to the thumb and fingers as well as the abductor pollicis longus and extensor carpi ulnaris. The inconsistency in the nomenclature regarding these nerve branches involves where the posterior interosseous nerve begins, and whether the posterior interosseous nerve and the deep radial motor branch are one and the same nerve:
Clinical
Radial Neuropathy at the Spiral Groove
The most common radial neuropathy occurs at the spiral groove. Here, the nerve lies juxtaposed to the humerus and is quite susceptible to compression, especially following prolonged immobilization (Figure 21–8). One of the times this characteristically occurs is when a person has draped an arm over a chair or bench during a deep sleep or while intoxicated (‘Saturday night palsy’). The subsequent prolonged immobility results in compression and demyelination of the radial nerve. Other cases may occur after strenuous muscular effort, fracture of the humerus, or infarction from vasculitis. Clinically, marked wrist drop and finger drop develop (due to weakness of the EIP, extensor digitorum communis, extensor carpi ulnaris, and long head of the extensor carpi radialis), along with mild weakness of supination (due to weakness of the supinator muscle) and elbow flexion (due to weakness of the brachioradialis). Notably, elbow extension (triceps brachii) is spared. Sensory disturbance is present in the distribution of the superficial radial sensory nerve, consisting of altered sensation over the lateral dorsum of the hand, part of the thumb, and the dorsal proximal phalanges of the index, middle, and ring fingers.
Differential Diagnosis
The differential diagnosis of wrist drop, aside from a radial neuropathy at the spiral groove, axilla, and PIN, includes unusual presentations of C7–C8 radiculopathy, brachial plexus lesions, and central causes (Box 21–1). Because most muscles that extend the wrist and fingers are innervated by the C7 nerve root, C7 radiculopathy may rarely present solely with a wrist drop and finger drop, with relative sparing of non-radial C7-innervated muscles. However, several key clinical features help differentiate a C7 radiculopathy from a radial neuropathy, PIN, brachial plexopathy, or central lesion (Table 21–1). Radial neuropathy at the spiral groove or axilla should result in weakness of the brachioradialis, a C5–C6-innervated muscle, which should not be weak in a lesion of the C7 nerve root. On the other hand, radial neuropathy at the spiral groove and PIN should spare the triceps, which would be expected to be weak in a C7 radiculopathy. If a C7 radiculopathy is severe enough to cause muscle weakness, other non-radial C7-innervated muscles also should be weak (e.g., pronator teres, flexor carpi radialis), leading to weakness of arm pronation and wrist flexion. However, in rare situations, non-radial C7-innervated muscles may be relatively spared, making the clinical differentiation quite difficult.












