23 Femoral Neuropathy
Anatomy
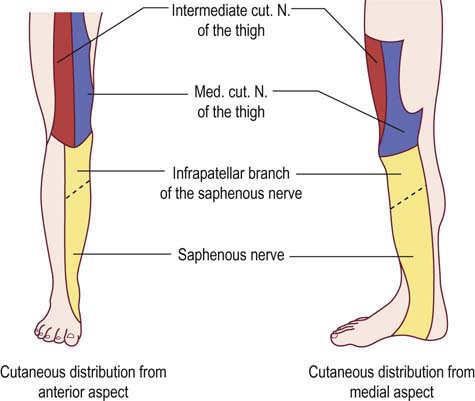
The femoral nerve is derived from the lumbar plexus and receives innervation from the L2, L3, and L4 nerve roots (Figure 23–1). In the pelvis, the nerve emerges from behind the psoas muscle to run laterally, deep to the iliac fascia above the iliacus muscle. Muscular branches are first given off to the psoas and then to the iliacus muscles (sometimes known together as the iliopsoas muscle) before the nerve runs beneath the inguinal ligament. It enters the thigh lateral to the femoral artery, behind the inguinal ligament, dividing approximately 4 cm below the inguinal ligament into anterior and posterior divisions. The anterior division gives rise to the medial and intermediate cutaneous nerves of the thigh and muscular branches to the sartorius and pectineus muscles. The posterior division supplies the quadriceps femoris muscles and then continues along the medial border of the calf as the saphenous nerve (Figure 23–2). The lateral thigh is not supplied by the femoral nerve but is innervated by the lateral femoral cutaneous nerve, which is derived directly from the lumbar plexus, receiving innervation from the L2–L3 nerve roots.
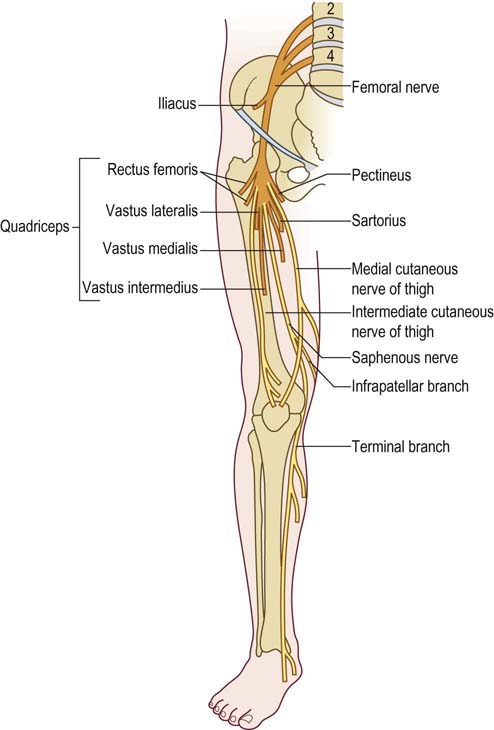
Figure 23–1 Anatomy of the femoral nerve.
(Reprinted with permission from Haymaker, W., Woodhall, B., 1953. Peripheral nerve injuries. WB Saunders, Philadelphia.)
Etiology
There are many reported etiologies of femoral neuropathy, although most cases result from positioning or compression during abdominal or pelvic surgery (Box 23–1). Most often implicated are self-retaining surgical retractors that are used in many pelvic and abdominal operations that compress the femoral nerve against the pelvis. In addition, there are increasing reports of femoral neuropathy occurring as a complication of total hip arthroplasty (THA), especially in THA revision surgery. While sciatic neuropathy remains the most common perioperative neuropathy associated with THA, it is now followed by femoral neuropathy. The mechanism of injury to the femoral nerve during THA is not always clear. In some cases, it may be due to a retraction injury, especially with an anterior or anterior lateral approach. In other cases, it may be due to compression arising posteriorly to the femoral nerve from the hip prosthesis itself. In other cases, similar to those reported for the sciatic nerve, excessive cement used to fix the prosthesis may damage the femoral nerve.
Box 23–1
Etiology of Femoral Neuropathy
Otherwise, isolated femoral neuropathies are uncommon. Iatrogenic femoral neuropathy can occur in the inguinal region as a consequence of hematoma formation from misguided femoral catheterizations. Femoral neuropathy may also occur in patients with diabetes mellitus, presumably from nerve infarction. However, this usually occurs in the setting of a more widespread polyradiculoplexopathy (i.e., diabetic amyotrophy). Likewise, retroperitoneal hemorrhage, often from excessive anticoagulation, may result in a lumbar plexopathy with prominent femoral involvement (see Chapter 32). Rare cases of tumor or other mass lesions may affect the femoral nerve as well.
Differential Diagnosis
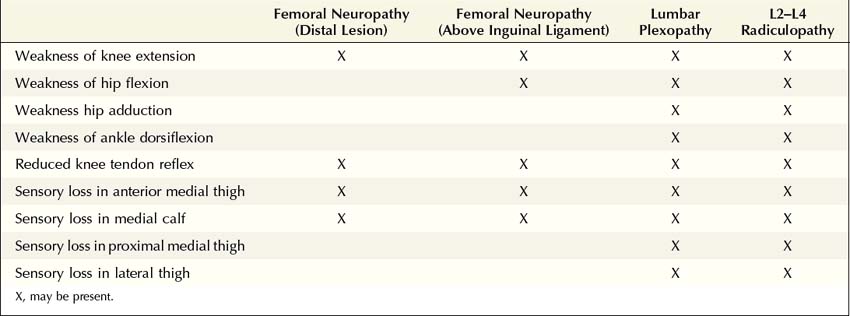
The differential diagnosis of femoral neuropathy includes lumbar plexopathy and L2–L4 radiculopathy (Table 23–1). Superficially, these three entities may appear very similar. All three may involve weakness of the quadriceps muscle and a depressed or absent quadriceps reflex. In an isolated femoral neuropathy, however, non-femoral-innervated L2–L4 muscles are normal. Specifically, the adductor muscles innervated by the obturator nerve and the ankle dorsiflexors (tibialis anterior) innervated by the peroneal nerve (L4–L5) are spared. By contrast, however, these muscles may be weak in lesions of the lumbar plexus or lumbar nerve roots. If pain is a major component, demonstrating slight weakness of the adductor muscles may be difficult. Pain radiating from the back or exacerbated with back motion suggests radiculopathy. The area of sensory abnormalities may be quite similar in femoral neuropathy, lumbar plexopathy, and L2–L4 radiculopathy. However, abnormal sensation over the lateral thigh (lateral femoral cutaneous nerve territory) or the very proximal medial thigh (obturator nerve territory) does not occur in isolated femoral neuropathy; either of these findings suggests a plexus or root lesion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree