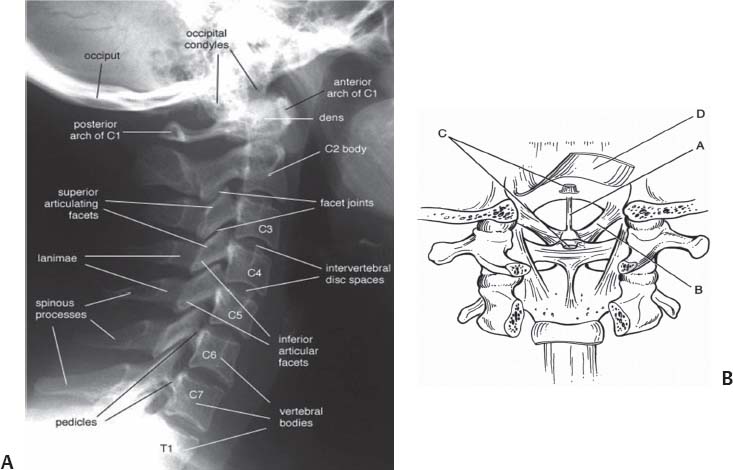
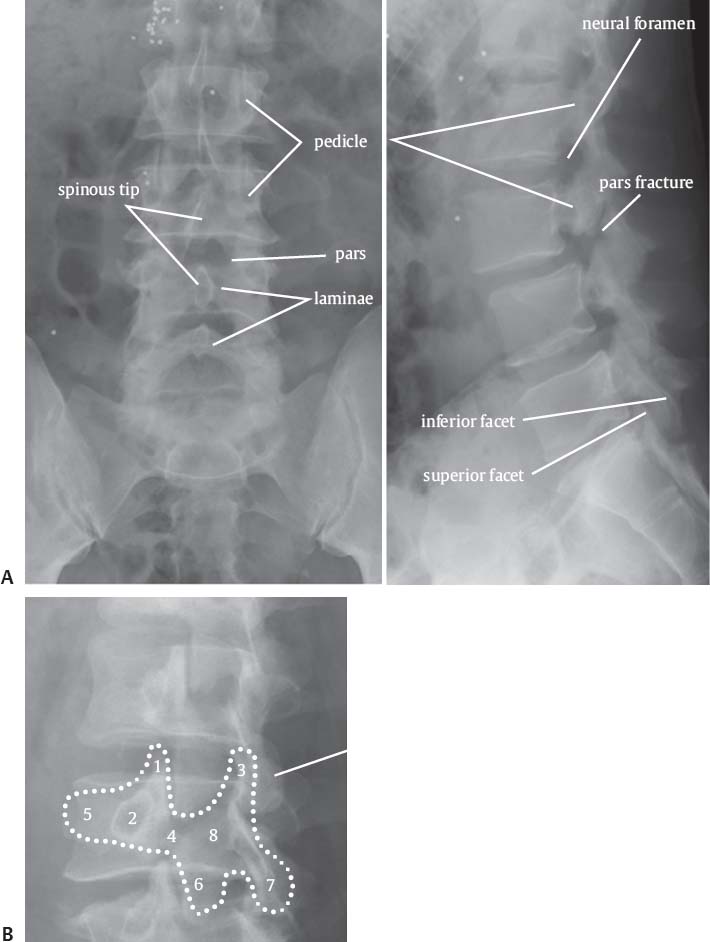
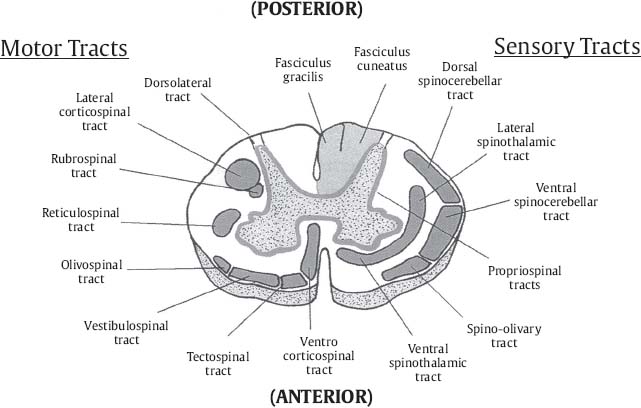
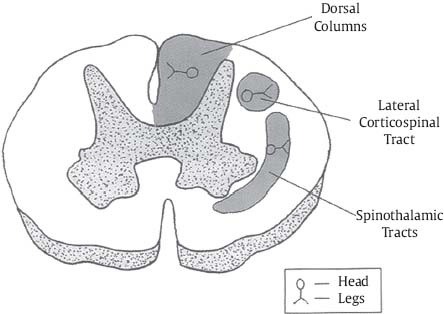
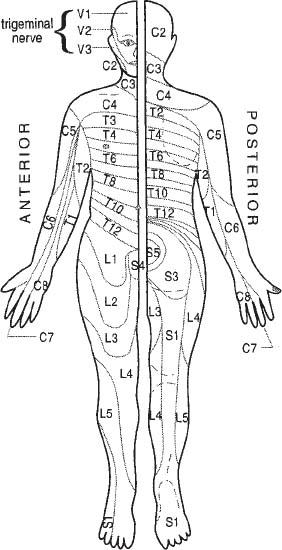
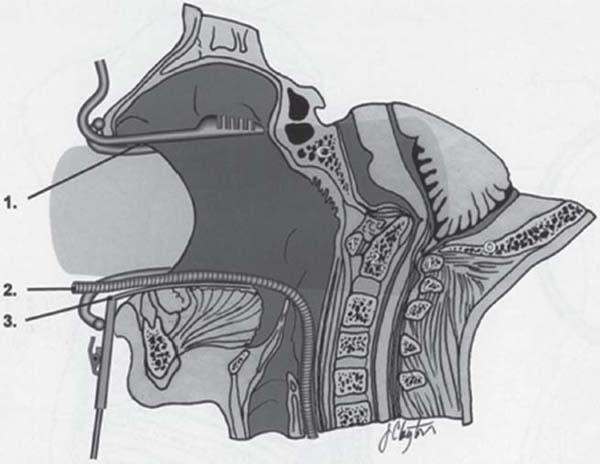
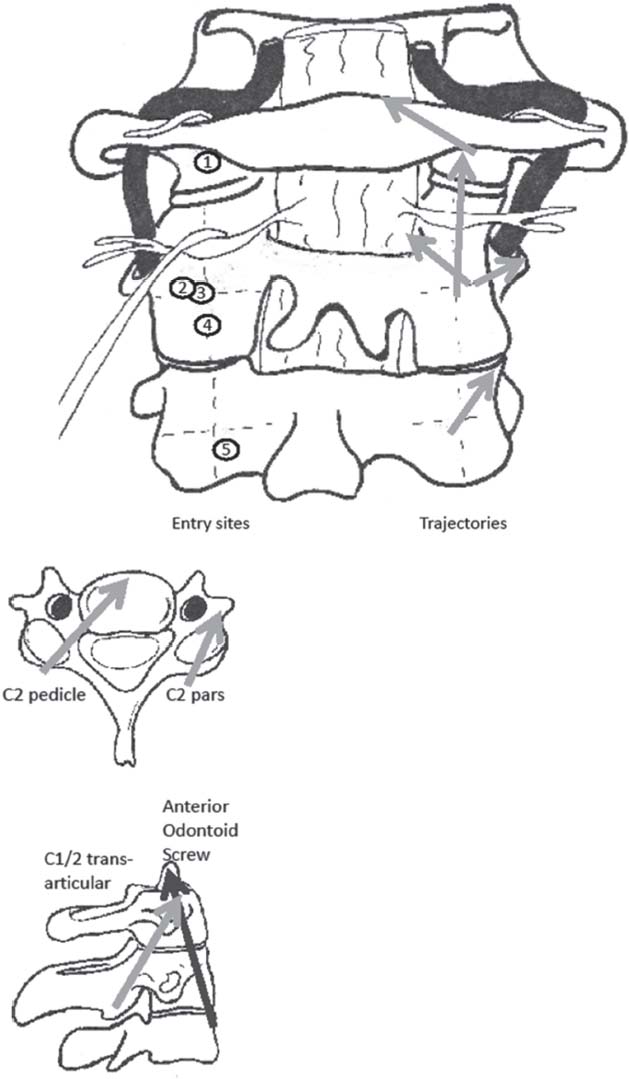
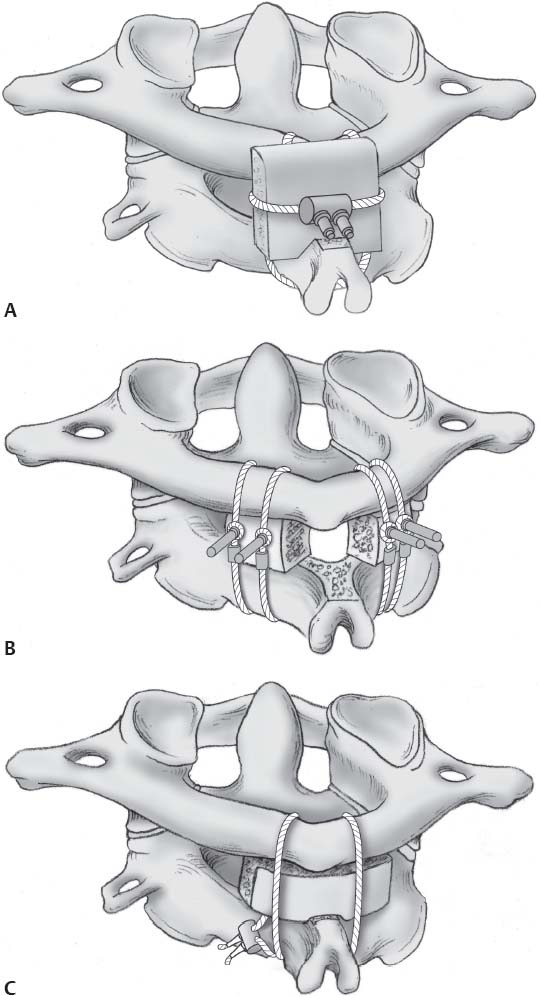
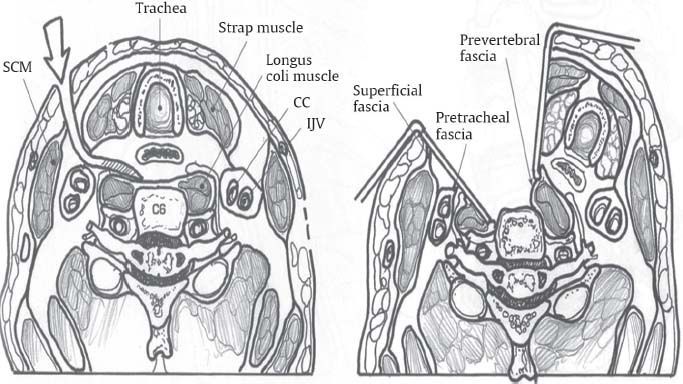
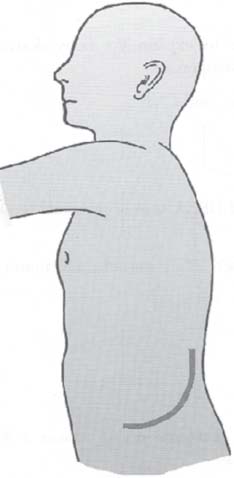
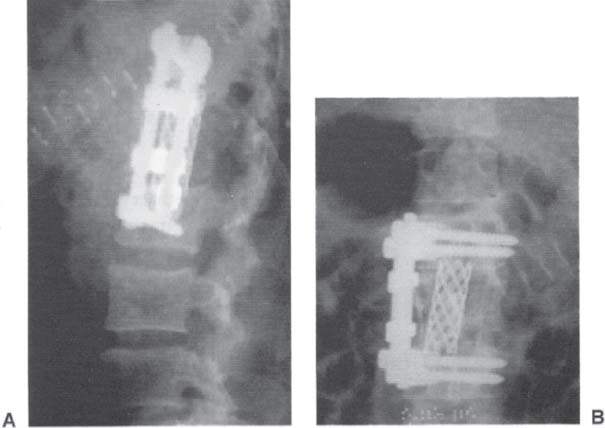
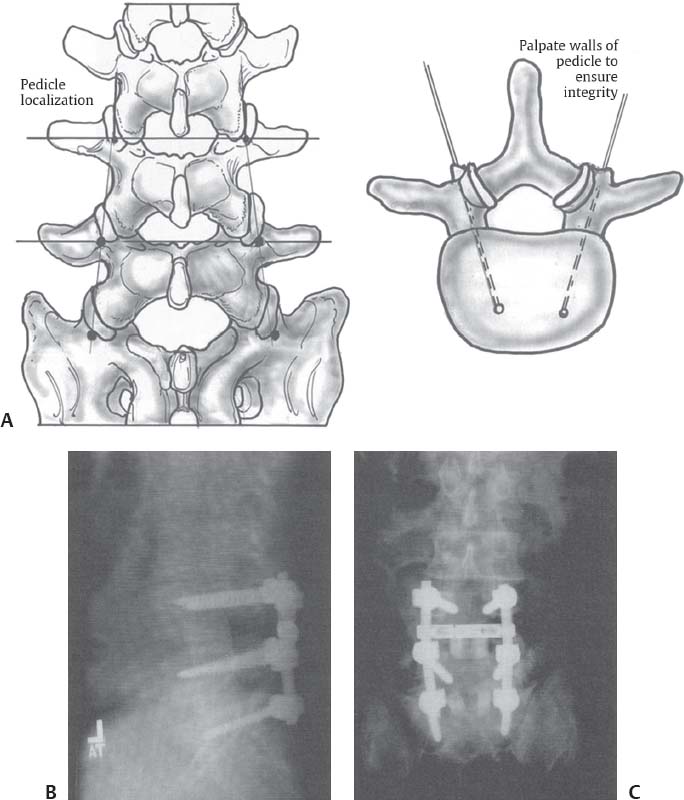
C H A P T E R 1 SPINAL ANATOMY AND APPROACHES I. SPINAL COLUMN ANATOMY A. Cervical—Should see smooth anterior spinous line, posterior spinous line, spinolaminar line, and spinous tip line; atlantooccipital distance should be <10 mm; C1–odontoid distance should be <5 mm; facets should look like shingles. Rule of Spence says C1 (Fig. 1.1) lateral masses should not extend more than a total of 7 mm over C2 (on odontoid view). B. Thoracolumbar (Fig. 1.2) Fig. 1.1 (A) Cervical anatomy. (B) Cervical ligamentous anatomy. A, apical; B, alar; C, cruciform; D, tectorial. Fig. 1.2 Thoracolumbar anatomy. (A) AP view, and (B) oblique view (to look at pars and down the pedicle axis) “Scotty dog” view: 1. Ear–superior articular process of facet (left); 2. Eye–pedicle (left); 3. Tail–superior articular process of facet (right); 4. Neck–pars interarticularis, fractured (left); 5. Snout–transverse process (left); 6. Inferior articular process of facet (left); 7. Hind leg–inferior articular process of facet (right); 8. Body–lamina (left). A. Upper extremities are medial in the corticospinal tracts and spinothalamic tracts. B. Lower extremities are medial in the posterior columns (Figs. 1.3 and 1.4). Fig. 1.3 Spinal cord pathways. (With permission from Citow JS. Comprehensive Neurosurgical Board Review. New York, NY: Thieme Medical Publishers; 2000: 69, Fig. 1.39.) Fig. 1.4 Spinal cord somatotopic organization. (With permission from Citow JS. Comprehensive Neurosurgical Board Review. New York, NY: Thieme Medical Publishers; 2000: 70, Fig. 1.40.) III. ARTERIAL SUPPLY TO SPINAL CORD A. One anterior spinal artery forms from two vertebral arteries. There are two posterior spinal arteries. Anterior and posterior spinal arteries get radicular artery inputs with a watershed zone in midthoracic. B. Artery of Adamkiewicz (a radicular artery) usually enters the spinal canal on the left at T9–12 to supply T8 to the conus. IV. EVALUATION A. Motor exam—deltoid (C5), biceps (C5,6), triceps (C7,8), wrist extension (C6), finger extension (C7), finger flexion (C8), interosseous (T1), hip flexion (L2), knee extension (L4), dorsiflexion (L4), extensor hallucis longus (L5), and plantar flexion (S1) (also see section on footdrop) B. Sensory exam—key levels are C1 (no sensory branch), C2 (posterior head), C6 (thumb), C8 (pinky), T4 (nipples), T10 (umbilicus), L4 (anterior knee), L5 (big toe), and S1 (lateral foot) (Fig. 1.5). Fig. 1.5 Dermatome chart. (With permission from Greenberg MS. Handbook of Neurosurgery. 7th ed. New York, NY: Thieme Medical Publishers; 2010: 94, Fig. 5–13.) V. BASIC SPINE APPROACHES: ACCESSIBLE REGION (FREQUENT INDICATIONS) A. Transoral (Fig. 1.6) 1. Access to lower 2/3 clivus, anterior C1, odontoid 2. Indications: basilar invagination, tumors such as chordoma and chondrosarcoma) 3. Consider anterior neck endoscopic approach only if you are experienced with this technique B. Far lateral transcondylar 1. Access to foramen magnum 2. Indications: intradural lesions such as meningioma Fig. 1.6 Transoral approach and accessible spine regions. C. Suboccipital with midline posterior cervical 1. Access from occiput to C2/3 2. Indications: unstable conditions such as atlantooccipital dislocation 3. May do C2 pedicle or pars screw with C3 pedicle or pars or lateral mass screw based on anatomy (Fig. 1.7) D. Midline high posterior cervical 1. Access to C1–C3 for Brook, Gallie, Sonntag, or C1/2 transarticular screws 2. Indications: hangman fracture, dislocation, displaced or nonhealing odontoid fracture (Fig. 1.8) E. Anterior odontoid screw 1. Skin entry at T2, screw enters between C2 and C3 anterior border guided by K wire 2. Indications: nondisplaced type 2 odontoid fracture (Fig. 1.7) F. Posterior cervical 1. Access to C3–7 for laminectomy or laminoplasty 2. Indications: cervical spondylotic myelopathy with lordosis, tumor, ossified posterior longitudinal ligament (OPLL), add foraminotomy for foraminal stenosis 3. Add lateral mass screws (Fig. 1.7) for traumatic, degenerative, pathologic spondylolisthesis G. Anterior cervical 1. Access to C3–T1 2. Indications: corpectomies for trauma, tumor, infection, deformity, OPLL, diskectomy, and fusion for disk bulge (Fig. 1.9) 3. Avoid if posterior compression, > three levels, prior extensive neck surgery, severe osteoporosis H. Median sternotomy (trapdoor approach) with cardiothoracic (CT) surgeon Fig. 1.7 High posterior cervical fusion screw entry sites and trajectories. Use preoperative computed tomography (CT)/CT angiography to check anatomy, vertebral artery, and calculate screw sizes. 1. C1 lateral mass screw: hold down C2 nerve root, drill notch in inferior C1 arch, palpate medial wall of lateral mass, enter in midline or 5 mm lateral to medial wall of lateral mass, lean your hand 20 degrees lateral and 10 degrees caudal to aim for C1 anterior tubercle, use ~4 × 35 mm screw. 2. C2 pars screw: enter 3 mm rostral and 3 mm lateral to midpoint, lean your hand 10 degrees medial and 10 degrees caudal, use ~ 4 × 16 mm screw. 3. C2 pedicle screw: enter 3 mm rostral and 2 mm lateral to midpoint, lean your hand 15 degrees lateral and 20 degrees caudal, use ~4 × 35 mm screw. 4. C1/2 transarticular screw, enter 3 mm rostral and 3 mm lateral to inferomedial edge of C2/3 facet joint, use K wire as guide, lean hand 5 degrees medial and 45 degrees caudal to aim through joint and into C1 arch, use ~ 4 × 40 mm screw. 5. C3 through C7 lateral mass screw, enter 1 mm medial and 1 mm caudal to midpoint, lean hand 20 degrees medial and 20 degrees caudal to aim for superolateral corner of lateral mass, use 4 ×16 mm screw. Fig. 1.8 (A) Brook, (B) Gallie, and (C) Sonntag posterior cervical fusion techniques. (With permission from Fessler RG, Sekhar L. Atlas of Neurosurgical Techniques: Spine and Peripheral Nerves. New York, NY: Thieme Medical Publishers; 2006:135–136, Figs. 16-8 and 16-9.) Fig. 1.9 Anteromedial cervical approach and anatomy. 1. Access to T1–4 (stay on right side to avoid heart; use double lumen endotracheal [ET] tube to deflate one lung) 2. Indications: corpectomies for trauma, tumor, infection, deformity, and OPLL; diskectomy and foraminotomy for disk bulge I. Lower thoracotomy with CT surgeon. 1. Access to T5–L2 (stay on left side to avoid great vessels, incise two levels above pathology) 2. Indications: anterior pathology such as trauma, infection, fracture, disks J. Posterior thoracic 1. Access to posterior T1–12 (only posterior pathology) 2. Indications: laminectomy for trauma, tumor, OPLL 3. Add transpedicular, costotransversectomy, or lateral extracavitary for lateral pathology 4. Add pedicle screws for instability (Fig. 1.10A–D) a. Pedicular or extrapedicular (between pedicle and rib head) b. Palpate pedicle with Penfield #4 to define its location Fig. 1.10 (A–D) Thoracic pedicle screw placement. c. Enter 2 mm caudal to superior facet edge and even with superior facet lateral edge d. Lean hand laterally 30 degrees at T1 and only 10 degrees at T12 K. Retroperitoneal approach 1. Access to anterior L1–5 (left side to avoid liver and vena cava) 2. Incision above umbilicus gets you to L1–4 and below umbilicus for L4–S1 3. Divide left anterior abdominal muscles down to preperitoneal fat and dissect laterally cutting latissimus dorsi to expose quadratus lumborum and iliopsoas medially 4. Sweep sympathetic chain laterally and ureter medially 5. Clip aortic radicular arteries as needed 6. Remove pathology leaving contralateral cortex intact 7. Distract intervertebral space with pins 8. Place cage filled with bone graft, and secure with anterolateral plates (i.e., Kaneda) (Figs. 1.11 and 1.12) Fig. 1.11 Retroperitoneal approach. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 139, Fig. 12.13.) Fig. 1.12 (A) Lateral x-ray of Kaneda plate fusion. (B) Anteroposterior x-ray of Kaneda plate fusion. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 139, Fig. 12.14.) 9. Indications: tumor, infection, spondylosis, anterior lumbar interbody fusion (ALIF), arthroplasty, trauma L. Transabdominal 1. Access to direct anterior L5–S1 for ALIF or arthroplasty M. Posterior lumbosacral 1. Access to L1–sacrum for laminectomy 2. Add transforaminal lumbar interbody fusion (TLIF; complete foraminotomy for nerve root decompression) or posterior lumbar interbody fusion (PLIF) if familiar with them 3. Add pedicle screws for instability a. Drill off lateral facet, enter at midpoint of transverse process at facet/TP junction, lean hand laterally 30 degrees (Fig. 1.13) 4. Indications: neurogenic claudication from lumbar stenosis, trauma, tumor, infection, recurrent radiculopathy (TLIF) Fig. 1.13 Lumbar pedicle screw placement. (A) Pedicle screw placement. (B) Lateral x-ray of L4–S1 pedicle screw fusion with tangent bony posterior lumbar interbody fusion (PLIF). (C) Anteroposterior x-ray of L4–S1 pedicle screw fusion with tangent bony PLIFs. (Fig. 1.13B,C with permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 138, Fig. 12.12A,B.) N. Lateral lumbosacral 1. Access to L2–L4 (e.g. DLIF or XLIF) if you are familiar with them; cannot reach L1 laterally due to ribs or L5 laterally due to iliac crest VI. COMMON COMPLICATIONS ASSOCIATED WITH BASIC APPROACHES (WITH PREVENTION/TREATMENT STRATEGIES) A. Transoral—cerebrospinal fluid (CSF) leak (lumbar drain), infection (preop oral cultures), vascular injury (preop computed tomography angiography [CTA]), dysphagia (postop percutaneous endoscopic gastrostomy tube [PEG]), respiratory difficulties (postop tracheotomy), tongue swelling (relax retractor every hour [q1h]) B. Anteromedial cervical—wrong level (intraop fluoroscopy), paralysis from hyperextension injury in severe stenosis (fiberoptic intubation, exam after positioning, somatosensory evoked potentials [SSEPs]), dysarthria (use left side to avoid the lower coursing left recurrent laryngeal nerve [RLN]), dysphagia (good longus coli release to hold retractor, postop barium swallow study for esophageal leak, postop steroids), thoracic duct injury (leave drain; low-fat diet), stroke and Horner syndrome (do not dissect lateral to longus coli or around carotid sheath), CSF leak (leave eggshell of bone in OPLL), C5 palsy (don’t retract nerve), vertebral artery injury (don’t go beyond lateral annulus), sleep apnea or bradycardia (C3/4 procedures), pneumothorax (check postop chest x-ray [CXR] in low cervical cases), CSF leak (treat with fibrin glue and lumbar drain), graft subsidence (too much endplate drilling), pseudo-arthrosis (redo, extend fusion, add posterior tension band fusion), worsened myelopathy in 5% (counsel patient preop) C. Posterior cervical—wrong level (intraop fluoroscopy), neurologic injury (fluoroscopy, SSEPs, and motor evoked potentials [MEP]), infection (lavage, Prolene sutures), C5 palsy (1–2 mm Kerrison rongeur during foraminotomy), vertebral artery injury (don’t pull out screws that hit artery), instability (fuse if straight or kyphotic) D. Thoracotomy—pneumothorax (chest tube), chylothorax (try to ligate; leave drain; low-fat diet), vascular (ask CT surgeon), neurologic injury (restrict only to anterior pathology; SSEPs and MEPs), thoracic radiculopathy (avoid neurovascular bundle adhered to inferior rib margin), hypohidrosis or Horner (avoid high thoracic sympathetic chain) E. Left lateral paramedian incision for anterior lumbar—vascular and visceral injuries (ask general surgeon to expose), infertility (avoid sympathetic plexus, monitor hypogastric plexus), hernia (ask general surgeon to close) G. Traction with Gardner-Wells or Halo 1. Epidural hematoma, skull fracture, herniated disk, occipitoatlantal dislocation, infection 2. Halos can result in swan neck deformity in midcervical (C3–5) H. Prophylactic Surgical Antibiotics 1. Ancef—1 g intravenously (IV) 1 hour before incision and 24 hours postsurgery 2. Vancomycin—if patient allergic to Ancef 3. For nasal or oral surgery—gentamicin 120 mg IV q8h and clindamycin 300 mg IV q8h for 24 hours Helpful Hints
1: SPINAL ANATOMY AND APPROACHES
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree