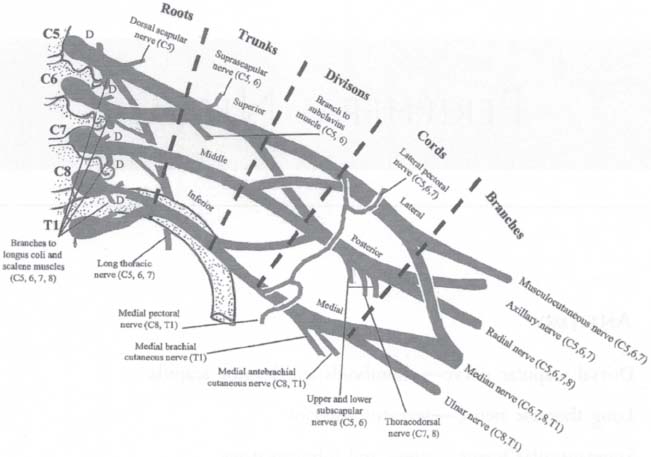
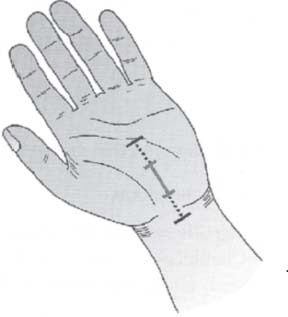
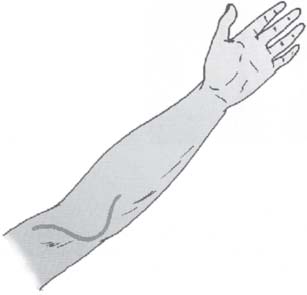
C H A P T E R 13 PERIPHERAL NERVES I. ANATOMY A. Dorsal scapular nerve—rhomboids and levator scapula B. Long thoracic nerve—serratus anterior C. Suprascapular nerve—supra- and infraspinatus D. Thoracodorsal nerve—latissimus dorsi E. Phrenic nerve (C3–C5)—diaphragm F. Axillary nerve—deltoid and teres minor G. Musculocutaneous nerve—coracobrachialis, biceps, and brachialis H. Radial nerve—triceps, brachioradialis, and extensor carpi radialis longus and brevis 1. Posterior interosseous nerve—supplies the supinator, extensor carpi ulnaris, extensor digitorum, extensor digiti minimi, extensor pollicis longus and brevis, extensor indicis, and abductor pollicis longus (not median nerve) I. Median nerve—pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, abductor pollicis brevis, flexor pollicis brevis (also by ulnar nerve), opponens pollicis, and lumbricals 1 and 2 1. Anterior interosseous nerve—supplies the flexor digitorum profundus 1 and 2, flexor pollicis longus, and pronator quadratus J. Ulnar nerve—flexor carpi ulnaris, flexor digitorum profundus 3 and 4, abductor digiti minimi, opponens digiti minimi, flexor digiti minimi, lumbricals 3 and 4, dorsal and palmar interosseous, flexor pollicis brevis (also by the median nerve), and adductor pollicis Fig. 13.1 Brachial plexus anatomy. (With permission from Citow JS. Comprehensive Neurosurgical Board Review. New York, NY: Thieme Medical Publishers; 2000: 80, Fig. 1–44.) K. Brachial plexus (Fig. 13.1) L. Superior gluteal nerve (L4–S1)—gluteus medius and minimus and tensor fascia lata M. Inferior gluteal nerve (L5–S2)—gluteus maximus N. Femoral nerve (L2–4)—iliacus, psoas, quadriceps femoris (rectus femoris and vastus lateralis, intermedius, and medialis), and sartorius 1. There is also sensory innervation to the knee (anterior femoral cutaneous nerve) and medial knee to foot (saphenous nerve). O. Obturator nerve (L2–4)—adductor brevis, adductor longus, adductor magnus (also by sciatic nerve), gracilis, and obturator externus P. Sciatic nerve (L4–S3)—exits through the greater sciatic foramen to innervate the semimembranosus, semitendinosus, biceps femoris, and adductor magnus (also by the obturator nerve) a. Medial plantar nerve—abductor hallucis, flexor digitorum brevis, and flexor hallucis brevis b. Lateral plantar nerve—abductor digiti minimi, flexor digiti minimi, adductor hallucis, and interosseus muscles 2. Common peroneal nerve a. Superficial peroneal nerve—peroneus longus and brevis b. Deep peroneal nerve—tibialis anterior, extensor digitorum longus, extensor hallucis longus, peroneus tertius, and extensor digitorum brevis 3. Sensory branches—posterior femoral cutaneous nerve, tibial nerve (most of lower leg and sole of foot), and sural nerve (a small patch of lateral foot) Q. Lateral femoral cutaneous nerve (L2, L3)—sensation to lateral thigh R. Pudendal nerve (S2–S4)—sensation to perineum and external genitalia and motor to the external anal and urethral sphincters S. Pelvic nerves (S2–4)—parasympathetic input for bowel, bladder, and sexual function T. Miscellaneous sensory nerves—subcostal (T12), iliohypogastric (L1), ilioinguinal (L1), and genitofemoral (L1, 2) II. ENTRAPMENT SYNDROMES A. Greater occipital neuralgia—from a C2 sensory branch 1. Superior nuchal trigger point—2.5 cm lateral and below the external occipital protuberance near the occipital artery 2. C1 or C2 fracture or subluxation—may crush the dorsal root ganglia 3. Treatment—usually with a nerve block using local anesthesia and steroids (10 mL 1% Marcaine and 40 mg Depo-Medrol) a. Surgery—can be performed to avulse the nerve beyond the transverse process of C2 and the inferior oblique muscle (rarely needed) B. Carpal tunnel syndrome—median nerve entrapment at the wrist by the transverse carpal ligament 1. Anatomy a. Median nerve—passes between the two heads of the pronator teres in the upper forearm b. Anterior interosseus nerve branch—supplies motor innervation for wrist and finger flexion c. Median nerve—passes under transverse carpal ligament (TCL) medial to flexor carpi radialis tendon, lateral to palmaris longus tendon, and above tendons of flexor digitorum superficialis and profundus d. Recurrent motor branch—normally arises under TCL (though rarely it runs through it) to supply lumbricals 1 and 2, opponens pollicis, and abductor and flexor pollicis brevis (LOAF) muscles e. Palmar cutaneous branch—arises from radial side of nerve, 5 cm proximal to TCL and passes above it f. TCL—extends from palm to 3 cm beyond distal wrist crease 2. Cause—most cases related to repetitive hand motion a. Acute severe carpal tunnel syndrome may be caused by thrombosis of a persistent median artery or a local hematoma. b. Associated conditions—acromegaly, amyloid, multiple myeloma, hypothyroidism, diabetes, mucopolysaccharidosis, rheumatoid arthritis, and pregnancy 3. Signs/Symptoms a. Dysesthesias (usually nocturnal) involving the palmar side of the thumb, index and middle fingers, and half of the ring finger b. Sensory loss c. Weakness of the LOAF muscles d. Thenar atrophy e. Characteristic splitting of sensation of the fourth finger does not occur with nerve root or plexus lesions. a. History b. Motor evaluation—especially opponens of thumb to middle finger and thumb elevation/abduction c. Tinel sign—tapping over TCL d. Phalen’s maneuver—symptoms reproduced by wrist flexion e. Nerve conduction velocity (NCV)—prolonged distal latency >3.7 f. Thyroid panel, growth hormone, complete blood cell count (CBC; for myeloma), glucose, and renal panel g. Laboratory evaluation—usually reserved for young patients with no history of repetitive hand movements 5. Treatment a. Most cases resolve with conservative management such as rest, nonsteroidal antiinflammatory drugs (NSAIDs), neutral position splinting, and steroid injections (in line with the ring finger medial to the palmaris longus tendon to avoid injuring the nerve). b. Surgery—involves division of the TCL i. Incision—from distal wrist crease to base of thumb in line with web space between third and fourth digits (Fig. 13.2) ii. Care is taken to avoid sectioning the palmar cutaneous branch on the radial side of the nerve. iii. To section entire TCL—scissors should be used to undercut 3 cm proximal to wrist crease and distally into hand until there is loss of resistance iv. Endoscopic division of TCL—also an option 6. Complications a. Section of palmar cutaneous branch or motor branch b. Damage to median nerve c. Delayed neuroma or hypertrophic scar formation Fig. 13.2 Carpal tunnel incision. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 163, Fig. 14.2.) d. Insufficient release of TCL e. Reflex sympathetic dystrophy—rare, usually self-limited in 2 weeks, and treated with phentolamine intravenously (IV) or a sympathetic block C. Pronator teres syndrome—entrapment of median nerve in forearm between the two heads of the pronator teres. The median nerve may also rarely be compressed in the upper arm at Struthers’ ligament connecting the medial epicondyle and the supracondylar process (an anatomic variant located 5–7 cm proximal to the medial epicondyle). 1. Causes—repetitive pronation or direct trauma 2. Signs/Symptoms—aching and fatiguing with grip weakness and median distribution paresthesias a. No characteristic nocturnal exacerbations b. Numbness in the palm; not seen with carpal tunnel syndrome because the palmar cutaneous branch travels over the TCL 3. Treatment—conservative, with surgery reserved for rare progressive cases D. Anterior interosseous syndrome—dysfunction of the anterior interosseous nerve, a branch of the median nerve innervating the flexor digitorum profundus 1 and 2, flexor pollicis longus, and pronator quadratus Fig. 13.3 A left claw hand. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 165, Fig. 14.3.) 1. “Pinch sign” may be seen with poor flexion of the thumb and distal phalanges 2. No sensory loss 3. Most cases resolve in 8–12 weeks with conservative management. E. Ulnar nerve entrapment—usually occurs at the elbow 1. Signs/Symptoms—hand weakness, hypothenar and interosseus wasting, claw deformity (by weakness of lumbricals 3 and 4), and sensory loss and paresthesias of the medial hand, pinky, and medial half of the ring finger (Fig. 13.3) 2. Evaluation—Tinel sign at the elbow, examination of finger abduction and digits 4 and 5 flexion, sensory examination (two-point discrimination is the most sensitive), and NCV 3. Treatment a. Neurolysis with or without transposition—subcutaneous (SC), intramuscular (IM), or submuscular b. Medial condylectomy—seldom performed at this time c. Results appear similar with neurolysis alone and with submuscular transposition—excellent 60%, fair 25%, poor 15% (no improvement or continued worsening) d. Technique for submuscular transposition i. Lazy incision ventral to medial epicondyle ii. Decompression of nerve across elbow iii. Opening cubital tunnel between the two heads of the flexor carpi ulnaris distally iv. Opening the arcade of Struthers proximally (a flat band of aponeurotic tissue anterior to the medial head of the triceps) v. Flexor tendons mass is then divided and the nerve tucked underneath along the bone vi. Tendon mass is then repaired in a relaxed fashion to avoid compression of the nerve vii. Care should be taken to avoid sectioning articular branches and branches to the flexor carpi ulnaris (Fig. 13.4). 4. Entrapment at the wrist—in Guyon canal above the transverse carpal ligament a. Rare and may be due to compression by a ganglion cyst b. No sensory loss in the dorsal hand and fingers because these nerve branches do not pass through the canal Fig. 13.4 Ulnar nerve incision. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 166, Fig. 14.4.) 5. Diffentiate from C8 radiculopathy a. Radiculopathy is associated with neck pain, referred medial scapular pain, and more proximal arm pain. b. All of the intrinsic hand muscles should be weak, including the median nerve–innervated muscles. c. No sensory loss splitting the ring finger F. Radial nerve entrapment—usually in the mid–upper arm (Saturday night palsy) 1. Cause—operative positioning or a humerus fracture 2. Signs/Symptoms—wristdrop without triceps weakness a. Rule out lead poisoning b. Entrapment in the forearm at the arcade of Frohse may cause a posterior interosseous syndrome with finger extension weakness, but no wristdrop or sensory loss. c. Radial tunnel syndrome is due to compression in the supinator tunnel above and below the elbow and causes elbow pain with little muscle weakness. It may respond to decompression. 3. Evaluation—NCV; exploration indicated if there is no improvement in 8 weeks. G. Suprascapular nerve entrapment—occurs in the suprascapular notch under the transverse scapular ligament 1. Signs/Symptoms—deep shoulder pain and supraspinatus and infra-spinatus muscle atrophy 2. Treatment—surgical decompression is effective if conservative management fails. H. Meralgia paresthetica (lateral femoral cutaneous nerve syndrome) 1. Cause—nerve entrapment under lateral inguinal ligament near anterosuperior iliac spine a. Usually seen with obesity, diabetes, pregnancy, and after surgery 2. Signs/Symptoms—burning dysesthesias over the anterior upper thigh 3. Evaluation—magnetic resonance imaging (MRI) and electromyogram (EMG) 4. Treatment—weight loss, NSAIDs, steroid injections, or open section of the inguinal ligament I. Peroneal nerve entrapment—usually due to compression of the common peroneal nerve at the fibular head. Symptoms include weakness of foot dorsiflexion and extensor hallucis longus, and less often foot eversion. Sensory loss is less common and involves the lateral aspect of the lower half of the leg. Evaluation is with MRI (rule out lumbar radiculopathy) and NCV. Footdrop may rarely be caused by a parasagittal brain tumor. Treatment is with decompression of the common peroneal nerve posterior to the fibular head, under the peroneus longus and above the soleus (Fig. 13.5). Fig. 13.5 Peroneal nerve exposure. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 168, Fig. 14.5.) 1. Cause—posterior tibial nerve entrapment under medial malleolus 2. Signs/Symptoms—pain and paresthesias of the toes and sole of the foot and weakness of intrinsic foot muscles 3. Treatment—surgical decompression indicated if conservative management (i.e., ankle support) fails III. PERIPHERAL NEUROPATHY A. Causes—DANG THE RAPIST—diabetes and drugs, amyloid, neoplasm and nutritional (B12), Guillain-Barré syndrome, trauma, heredity, endocrine, electrolytes, and entrapment, renal and radiation, alcohol and AIDS, porphyria and paraneoplastic syndrome, infectious, immunologic, and ischemic, sarcoid, and toxins (i.e., lead) B. Evaluation—glucose, Hgb1AC, thyroid stimulating hormone test (TSH), erythrocyte sedimentation rate (ESR), B12, NCV, EMG, and muscle and nerve biopsies IV. DIABETIC NEUROPATHY—may be sensory, motor, or autonomic A. Most commonly involves the distal sensory nerves (stocking-glove sensory loss) or femoral nerve B. Femoral neuropathy (which also may be caused by a psoas hematoma) is distinguished from an L4 radiculopathy by the presence of hip flexion weakness. V. CHARCOT-MARIE-TOOTH DISEASE—inherited peroneal hypertrophic neuropathy causing peroneal-innervated muscle atrophy. A. Onset—in adolescence B. Distal muscle atrophy occurs first in the feet and then the hands (claw hand). C. There is also sensory ataxia and weakness without autonomic dysfunction. A. Cause—autoimmune attack on the brachial plexus 2 weeks after an upper respiratory infection 1. May also be seen after radiation treatment or with diabetes B. Signs/Symptoms—shoulder pain, numbness, paresthesias, and polyradicular weakness C. Evaluation—NCV (demonstrates demyelination after 3 weeks) and a brachial plexus MRI and chest x-ray (CXR) (to rule out a structural lesion such as a Pancoast or plexus tumor) 1. Pancoast tumors usually involve the lower plexus. D. Treatment—steroids; usually resolves over time VII. BRACHIAL PLEXUS TRAUMATIC INJURY A. Preganglionic 1. Proximal to dorsal root ganglia 2. Not fixable 3. Associated with Horner syndrome, serratus anterior paralysis with scapular winging, and rhomboid weakness from dorsal scapular injury B. Postganglionic 1. May be amenable to nerve grafting procedures 2. Evaluation—EMG/NCV after 3 weeks 3. Erb-Duchenne palsy—C5–C6 birth injury with proximal weakness and bellhop tip posture 4. Klumpke’;s palsy—C8–T1 injury from a fall or Pancoast tumor causing a weak hand with claw deformity 5. T1 lesion may cause Horner syndrome VIII. TRAUMATIC NEUROPATHY B. Axonotmesis—interruption of axons and myelin with intact perineurium and epineurium. Spontaneous regeneration may occur at 1–2 mm/d. C. Neurotmesis—complete transection of the nerve and nerve sheath. Axonal regeneration may lead to neuroma formation. D. Nerve repair 1. Perform immediately (to prevent retraction) only for a clean laceration with a very sharp object that did not crush the nerve (i.e., scalpel) 2. Otherwise, wait 3–6 weeks to explore, to allow the scar to heal and the inflammation to resolve 3. Evaluation—may include physical examination to determine the injured nerve, NCV, and MRI (to visualize continuity) 4. Treatment a. In surgery, perform nerve action potentials (NAPs) over the neuroma to determine nerve continuity, and if positive, do only a neurolysis. b. Distal stump stimulation may be negative due to Wallerian degeneration, thus should not inhibit repair. c. If NAP is negative, resect the neuroma until clean fascicles are seen and repair with nerve grafts (sural nerve, radial cutaneous nerve, intercostals nerve, etc.) d. Earlier surgery preferred and if performed after 18 months, the muscle end plates may no longer be functional and the muscle may be fibrotic. e. When cable grafting, shorter distances are more successful, and be sure to avoid tension. f. Bioabsorbable polyglycol alcohol (PGA) tubes are now being used in place of nerve grafts. g. Apply a splint if the repair crosses over a joint. h. Results of repair will usually not be evident for 6 months. i. For flail arm, consider an intercostal nerve to musculocutaneous nerve repair and a tendon transfer; arm fusion may be needed to prevent dislocation. IX. PERIPHERAL NERVE TUMORS A. Neuroma—not a neoplasm 1. Inflammatory mass consisting of tangled axons, Schwann cells, and fibroblasts 2. Usually painful and rubbery B. Schwannoma 1. Firm, encapsulated, benign tumors growing eccentrically on the nerve with an epineurium capsule 2. Occur intracranially and along the spinal cord at the root entry zone of sensory nerves, in the head and neck, posterior mediastinum, retroperitoneum, and flexor surface of the extremities 3. Treatment—surgical resection when symptomatic C. Neurofibroma 1. Fusiform, unencapsulated, benign tumors infiltrating the width of the nerve 2. Cannot be completely removed without sacrificing the nerve 3. No reliable way to determine preoperatively whether the tumor is a schwannoma or a neurofibroma D. Malignant peripheral nerve sheath tumor 1. Unlike a benign tumor, usually painful and frequently causes motor deficit 2. 50% of patients have neurofibromatosis I (NF-1). 3. Treatment—resection and radiation E. Mass behind knee 2. Ganglion (Baker) cyst 3. Nerve sheath tumor—positive Tinel sign, able to be moved side-to-side, but not the length of the nerve, rarely with motor deficit unless malignant Helpful Hint
13: PERIPHERAL NERVES
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree