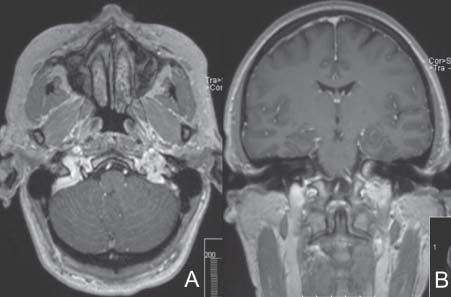
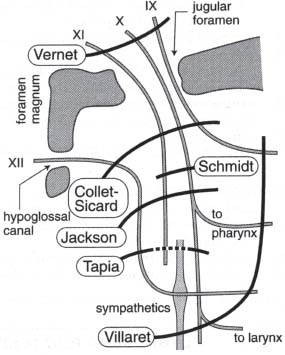
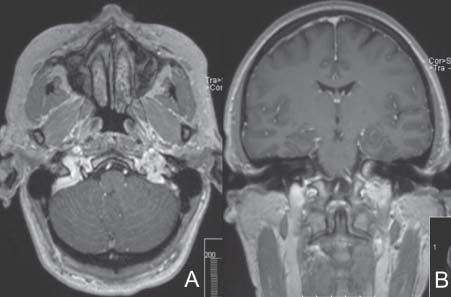
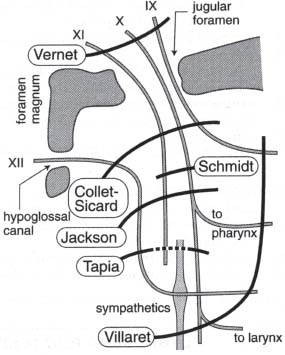
Case 25 Paraganglioma Nazer H. Qureshi and Ossama Al-Mefty Fig. 25.1 T1-weighted magnetic resonance image with contrast injection. (A) Axial cut taken at the level of the skull base and (B) coronal cut. At the first follow-up visit you discuss the pathology report with the patient, which reads as follows, “… sustentacular cell density and the immunohistochemical staining with S-100 and chromogranin of the chief cells in this tumor was very low.” Fig. 25.2 Left external carotid artery injection angiogram. Fig. 25.3 Schematic diagram of jugular foramen syndromes. (From Greenberg MS. Handbook of Neurosurgery. 6th ed. New York: Thieme Medical Publishers; 2006:86. Adapted with permission.)
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
25 Paraganglioma
Case 25 Paraganglioma Fig. 25.1 T1-weighted magnetic resonance image with contrast injection. (A) Axial cut taken at the level of the skull base and (B) coronal cut. Fig. 25.2 Left external carotid artery injection angiogram. Fig. 25.3 Schematic diagram of jugular foramen syndromes. (From Greenberg MS. Handbook of Neurosurgery. 6th ed. New York: Thieme Medical Publishers; 2006:86. Adapted with permission.)
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



