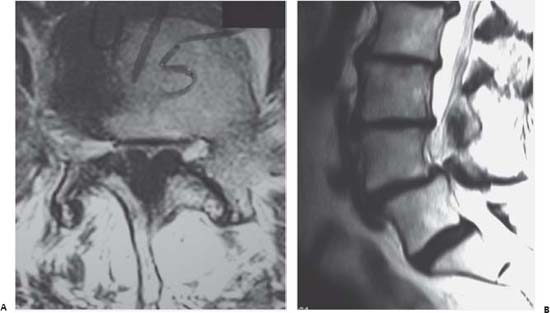
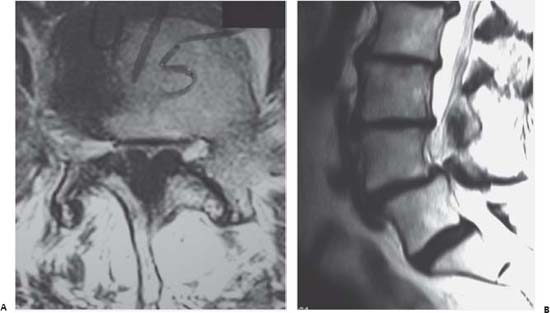
Case 90 Neurogenic versus Vascular Claudications Eric P. Roger and Edward Benzel Fig. 90.1 (A) Axial T2- weighted magnetic resonance image (MRI) at the L4–L5 disk space. (B) Sagittal T2- weighted MRI of the lumbar spine at the level of the midline. The patient has no evidence of arterial insufficiency on examination and has a positive “shopping cart” sign (resolution of the leg pain when leaning on a shopping cart while walking). He is able to use a stationary bicycle without pain or symptoms. His ankle brachial indices (ABIs) are 1.10 on the right, 1.08 on the left side.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
90 Neurogenic versus Vascular Claudications
Case 90 Neurogenic versus Vascular Claudications Fig. 90.1 (A) Axial T2- weighted magnetic resonance image (MRI) at the L4–L5 disk space. (B) Sagittal T2- weighted MRI of the lumbar spine at the level of the midline.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


