Case 32 Posterior Communicating Artery Aneurysm
Pascal M. Jabbour and Erol Veznedaroglu
Fig. 32.1 Computed tomography scan of the head showing diff use subarachnoid hemorrhage.
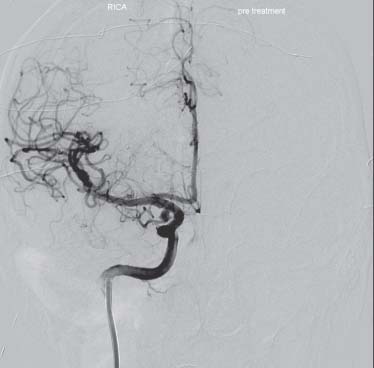
Fig. 32.2 Cerebral angiogram, right carotid injection showing a cerebral aneurysm.
- A 64-year-old right-handed woman with a history of high blood pressure and smoking presents to the emergency room after experiencing the worst headache of her life while she was driving her car.
- She does not have a history of migraine headaches and never complained of headaches before this episode.
- Her familial history is significant—a maternal aunt died 10 years ago from a ruptured brain aneurysm.
- Neurologic evaluation showed that the patient was alert, awake-oriented, with a dilated nonreactive pupil on the right side, with decreased ocular motility upward, inward and downward.
- A computed tomography (CT) scan of the head is shown in Fig. 32.1 and a cerebral angiogram is shown in Fig. 32.2.
< div class='tao-gold-member'>
 Clinical Presentation
Clinical Presentation Questions
Questions Answers
Answers


