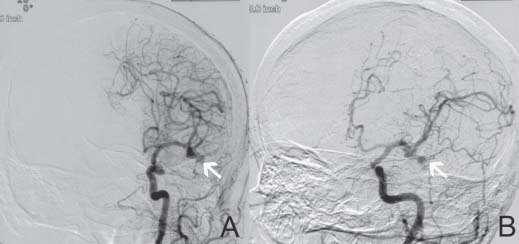
Case 44 High-grade Carotid Stenosis and Intracranial Aneurysm Fig. 44.1 Cerebral angiogram, left carotid injection, showing on (A) anteroposterior and (B) lateral views showing a left middle carotid artery trifurcation aneurysm of 7 mm in size.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue



