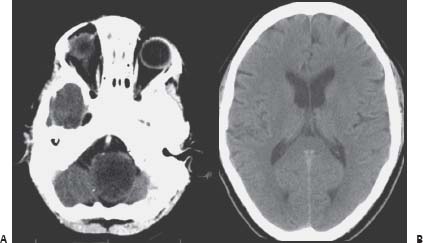
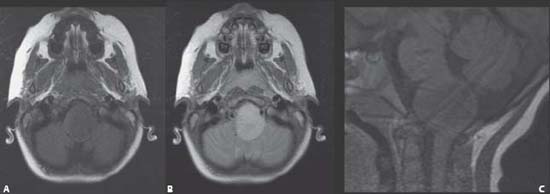
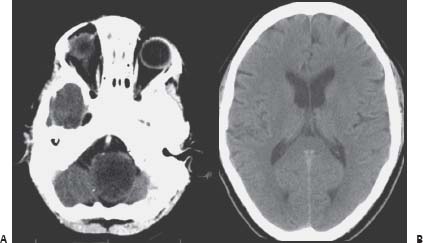
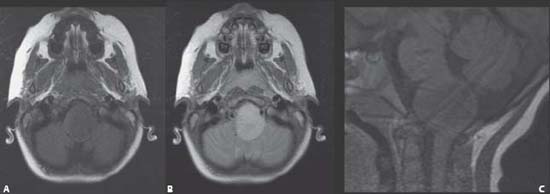
Case 59 Brainstem Glioma 2: Medulla Oblongata Jean-Pierre Farmer, Abdulrahman J. Sabbagh, and Ahmad Al-Jishi The patient was taken to surgery. A tumor was expanding the medulla oblongata, deforming the anatomy, and displacing the midline (Fig. 59.3). Using neuronavigation, the area closest to the surface was the point used for entry. On the frozen section, the patient’s specimen confirmed a diagnosis of juvenile pilocytic astrocytoma. Fig. 59.1 Computed tomography scan of the brain at the level of the (A) medulla and the (B) lateral ventricles.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
59 Brainstem Glioma 2: Medulla Oblongata
Case 59 Brainstem Glioma 2: Medulla Oblongata Fig. 59.1 Computed tomography scan of the brain at the level of the (A) medulla and the (B) lateral ventricles.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


