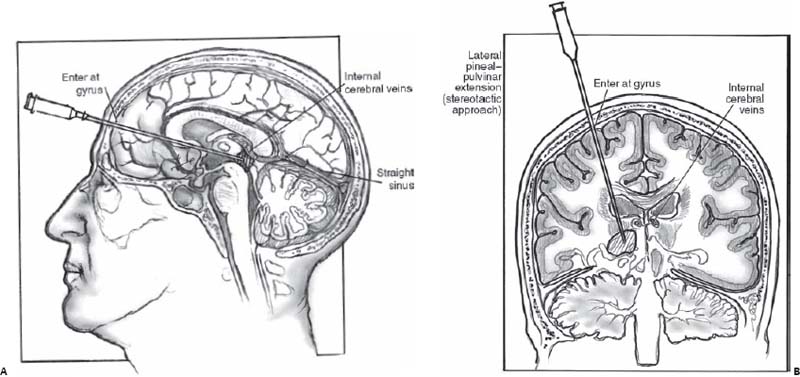
Case 60 Pineal Region Tumor Claude-Edouard Chatillon, José-Luis Montes, and Jean-Pierre Farmer Fig. 60.1 Computed tomography scan of the head without contrast at the level of the pineal gland. Fig. 60.2 Artist’s rendering of stereotactic approaches to pineal region tumors. (A) Low frontal (precoronal) approach avoids the internal cerebral veins above the tumor. (B) The lateral pineal pulvinar approach, which is lateral to the deep veins, is depicted. (From Sekhar L, Fessler R. Atlas of Neurosurgical Techniques: Brain. New York: Thieme Medical Publishers; 2006:570–571. Reprinted with permission.) In this case, tumor markers in the serum and cerebrospinal fluid (CSF) are negative.

 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
60 Pineal Region Tumor
Case 60 Pineal Region Tumor Fig. 60.1 Computed tomography scan of the head without contrast at the level of the pineal gland. Fig. 60.2 Artist’s rendering of stereotactic approaches to pineal region tumors. (A) Low frontal (precoronal) approach avoids the internal cerebral veins above the tumor. (B) The lateral pineal pulvinar approach, which is lateral to the deep veins, is depicted. (From Sekhar L, Fessler R. Atlas of Neurosurgical Techniques: Brain. New York: Thieme Medical Publishers; 2006:570–571. Reprinted with permission.)

 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


