Case 72 Tic Douloureux
Burak Sade and Joung H. Lee
- An 83-year-old right-handed man presents with a 2-year history of neuralgia-like pain on the right side of his face involving the ophthalmic (V1) and maxillary (V2) divisions of the trigeminal nerve.
- He has been taking carbamazepine and topiramate, which provided minimal relief, and says he no longer wishes to use these medications.
- His neurologic evaluation is within normal limits.
- Magnetic resonance imaging (MRI) of the brain is shown in Fig. 72.1.
- The patient underwent a microvascular decompression (MVD) procedure. At the time of surgery, the trigeminal nerve was found to be in severe compression by a redundant vertebrobasilar complex ventrally and inferiorly and by the anterior inferior cerebellar artery superiorly. Decompression was achieved using small pieces of Teflon paddies.
- He experienced immediate and complete recovery of his pain following surgery.
Fig. 72.1 Magnetic resonance imaging scan of the brain. Three-dimensional axial image of the Circle of Willis demonstrating a prominent vascular loop ventral to the trigeminal nerve root entry zone on the right side.
< div class='tao-gold-member'> Clinical Presentation
Clinical Presentation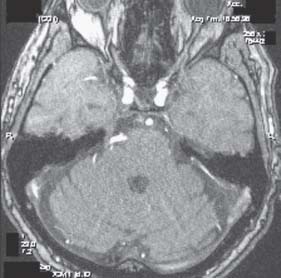
 Questions
Questions Answers
Answers


