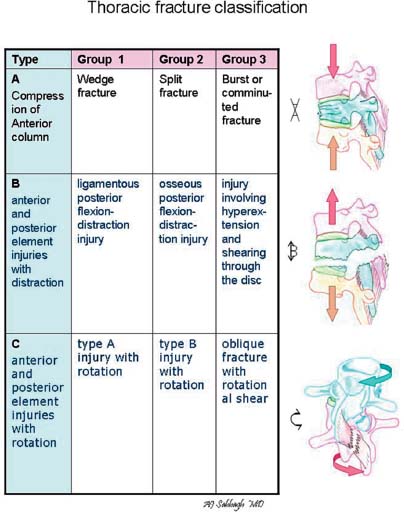
Case 85 Compression Fracture of the Thoracolumbar Spine Fig. 85.1 (A) Sagittal reconstructed computed tomography of the lumbar spine and (B) sagittal T2-weighed magnetic resonance image of the lumbar spine are shown. Fig. 85.2 Classification of thoracic fractures : (A) Type A, injury caused by compression of the anterior column; (B) type B, injury of the anterior column and the two posterior columns with distraction of the anterior or posterior elements; (C) type C, rotational injury of all three columns.

 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
85 Compression Fracture of the Thoracolumbar Spine
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


