Case 86 Lumbar Burst Fracture
Ahmed Jaman Alzahrani and Khalid N. Almusrea
Fig. 86.1 (A) Computed tomography scan of the lumbar spine with axial section through L3 and (B) sagittal reconstructed image.
- A 70-year-old man presents 4 days after a motor vehicle accident, transferred from a local hospital, with the complaint of severe lower back pain.
- The pain radiates to left thigh in an L3 dermatomal distribution.
- On examination he is neurologically intact.
- He has an unremarkable past medical history.
- A computed tomography (CT) scan of the lumbar spine was done at the local hospital (Fig. 86.1).
Fig. 86.2 Magnetic resonance imaging scan of the lumbar spine with (A) T2-weighted sagittal section and (B) axial section images through L3.
< div class='tao-gold-member'>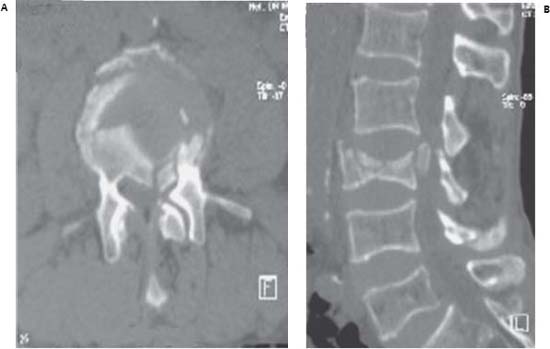
 Clinical Presentation
Clinical Presentation Questions
Questions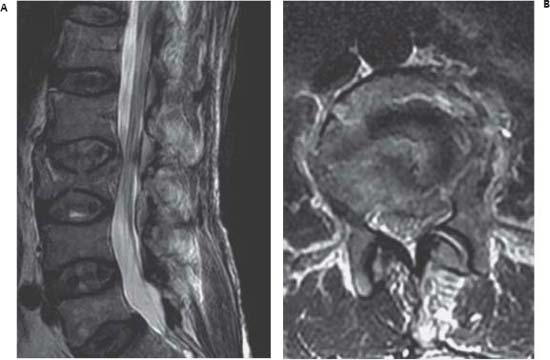
 Answers
Answers


