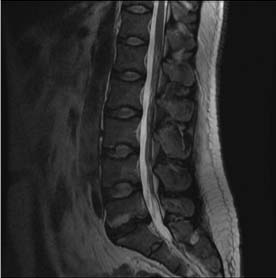
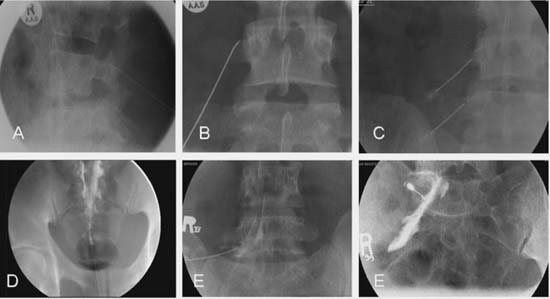
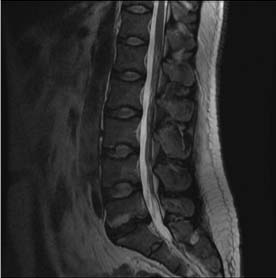
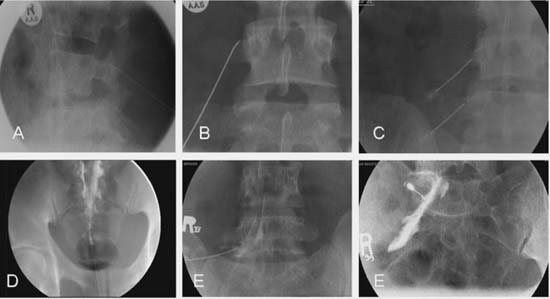
Case 89 Lower Back Pain — Conservative Management Hashem Al Hashemi, Remi Nader, and Abdulrahman J. Sabbagh Fig. 89.1 T2-weighted sagittal magnetic resonance image of the lumbar spine demonstrating degenerative disk disease at the L5–S1 level. Fig. 89.2 Plain radiographs taken while performing the following interventional procedures: (A,B) L3 medial branch neurotomy and L3 and (C) L4 medial branch blocks, (D) caudal epidural steroid injection, (E) L5 transforaminal epidural steroid injection, and (F) S1 transforaminal epidural steroid injection.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
89 Lower Back Pain — Conservative Management
Case 89 Lower Back Pain — Conservative Management Fig. 89.1 T2-weighted sagittal magnetic resonance image of the lumbar spine demonstrating degenerative disk disease at the L5–S1 level. Fig. 89.2 Plain radiographs taken while performing the following interventional procedures: (A,B) L3 medial branch neurotomy and L3 and (C) L4 medial branch blocks, (D) caudal epidural steroid injection, (E) L5 transforaminal epidural steroid injection, and (F) S1 transforaminal epidural steroid injection.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


