Acute Back Pain/Radiculopathy, Post-Operative
Kevin R. Moore, MD
DIFFERENTIAL DIAGNOSIS
Common
Intervertebral Disc Herniation, Recurrent
Intervertebral Disc Herniation, Acute
Intervertebral Disc Herniation, Cervical
Intervertebral Disc Herniation, Thoracic
Intervertebral Disc Herniation, Lumbar
Intervertebral Disc Extrusion, Foraminal
Peridural Fibrosis
Less Common
Post-Operative Infection
Abscess, Paraspinal
Abscess, Epidural
Abscess, Subdural
Post-Operative Complication
Hematoma
Hematoma, Epidural
Hematoma, Subdural
Hardware Failure
Vertebroplasty Complications
Bone Graft Complications
Rare but Important
Post-Operative Complication
Brachial Plexus Traction Injury
Infarction, Spinal Cord
Post-Operative Infection
Abscess/Myelitis, Spinal Cord
ESSENTIAL INFORMATION
Helpful Clues for Common Diagnoses
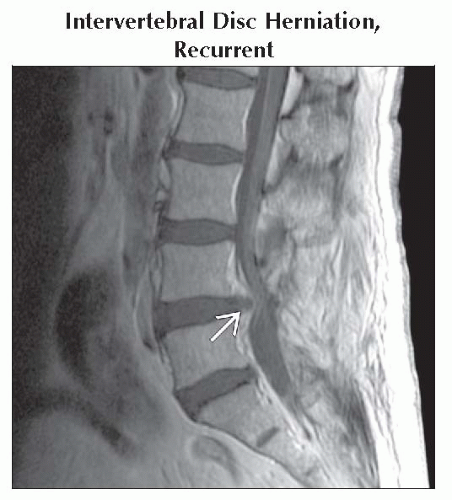
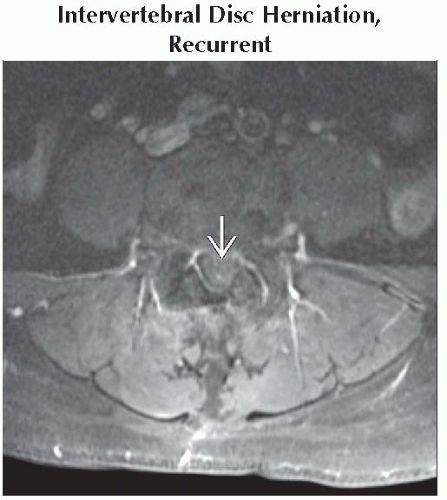
Intervertebral Disc Herniation, Recurrent
Focal extension of disc material beyond endplate margins at previously operated intervertebral disc level
Subset of failed back surgery syndrome (FBSS)
Fat suppression of T1WI (pre- and post-gadolinium) may increase sensitivity for detecting peridural fibrosis and for differentiating fibrosis from disc herniation
Intervertebral Disc Herniation, Acute
Localized (< 50% of disc circumference) displacement of disc material beyond edges of vertebral ring apophyses
Unfortunate luck to present with new disc herniation after previous surgery at another level
Peridural Fibrosis
Scar formation within epidural space following lumbar surgery
Subset of FBSS
Fat suppression of T1WI (pre- and post-gadolinium) increases sensitivity for detecting peridural fibrosis and for differentiating fibrosis from disc herniation
Helpful Clues for Less Common Diagnoses
Post-Operative Infection
Infectious sequelae following operative procedures
May manifest in one or more areas at operative site including paravertebral tissues and subdural or epidural spaces, but frequently starts in intervertebral disc space
Abscess, Paraspinal
Infection of paravertebral soft tissues surrounding spine
Paravertebral enhancing phlegmon or peripherally enhancing liquified collection
Abscess, Epidural
Extradural spinal infection producing abscess formation
Frequently spondylodiscitis extends into adjacent epidural space ⇒ enhancing epidural phlegmon ± peripherally enhancing fluid collection
May also see isolated epidural abscess without discitis
Lower thoracic, lumbar > cervical, upper thoracic
Abscess, Subdural
Purulent pus collection developing in “potential” space between dura and arachnoid
Post-Operative Complication
Hematoma, Epidural
Blood extravasation into the epidural spinal compartment
Long segmental extra-axial mass encasing or displacing spinal cord or cauda equina
Typically multisegmental, but may be focal when associated with focal fracture or disc extrusion
Hematoma, Subdural
Accumulation of blood between dura and arachnoid
Signal characteristics variable depending on age of blood products
Hardware Failure
Mechanical breakdown, malfunction, or malposition of metallic implant
May present either with chronic pain or calamitously with acute pain
Vertebroplasty Complications
Cement extravasation into spinal canal, foramen, or vertebral venous plexus
Pulmonary artery cement embolization
Vertebral osteomyelitis
“Bounce back” vertebral fracture
Bone Graft Complications
Graft migration, graft displacement, or graft extrusion
Abnormal alignment, position, or placement of graft ± associated neurologic deficit, instability, infection
Cervical > thoracic > lumbar
Helpful Clues for Rare Diagnoses
Post-Operative Complication
Brachial Plexus Traction Injury
Stretch injury or avulsion of ≥ 1 cervical roots, brachial plexus
Stretch injury: Enlargement or attenuation of stretched (but contiguous) plexus elements
Avulsion injury: Attenuated or disrupted proximal roots/rami within or immediately distal to lateral CSF-containing dural sac diverticulum devoid of neural elements ± retracted distal nerve roots, nerve “retraction ball”
Infarction, Spinal Cord
Thoracic spinal cord infarction 2° arterial occlusion (radicular artery)
Artery of Adamkiewicz frequently implicated
Usually extends to involve more than one vertebral body segment
Central hyperintensity on T2WI more common than wedge-shaped involvement of anterior 2/3 of spinal cord
Post-Operative Infection
Abscess/Myelitis, Spinal Cord
Spinal cord infection with necrosis
Spinal cord neoplasm mimic; ring-enhancing mass within cord with appropriate clinical history of inflammation/infection is highly suggestive
Pyogenic infection most common but granulomatous infections have been described
May show positive diffusion (reduced ADC) restriction similar to brain abscess, but lack of diffusion restriction does not exclude abscess
Image Gallery
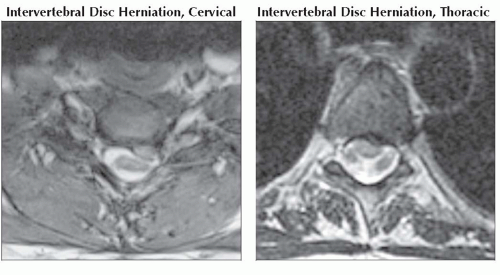 (Left) Axial T2* GRE MR reveals a large left cervical disc herniation producing spinal cord deformation and narrowing of the left lateral spinal canal. (Right) Axial T2WI MR depicts a left paracentral thoracic disc herniation that produces mild spinal cord deformation but no significant narrowing of the central spinal canal.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|