Figure 17-1 The serial nerve conduction studies of the left peroneal motor nerve (A) and the right tibial motor nerve (B) in acute stage: upper trace, the initial study which revealed severe conduction block between knee and ankle at 15 hours after symptom onset; lower trace, follow-up study at 7 days after symptom onset, which showed deceased amplitude from stimulation at both levels (knee and ankle). These findings suggest that 15 hours after paraplegia, conduction block was observed between knee and ankle. By 7 days conduction block was no longer present and many nerve fibers had degenerated leaving small and similar potentials from stimulation at both knee and ankle sites.
Twenty hours after symptom onset, transverse arteriotomy was performed on both the common femoral arteries. A multihole angiography catheter was introduced into the abdominal aorta and intraoperative aortogram was taken. The injected dye was stagnated in the distal abdominal aorta (Fig. 17-2A). Embolectomy using balloon catheter was performed under C-arm guidance at both iliac and femoral arteries. After the procedure, blood flow was maintained from abdominal aorta to both femoral arteries (see Fig. 17-2B). The extracted embolus had a saddle shape (Fig. 17-3), which was composed of blood clot. Two weeks later, the motor function of both lower extremities improved to above grade 3 on the MRC scale. After postoperative week 3, follow-up nerve conduction studies revealed a low-amplitude response in all the motor responses (Fig. 17-4), but all the sensory responses of lower extremity including sural, superficial peroneal sensory, medial femoral cutaneous nerves were unobtainable. Electromyography revealed abnormal spontaneous activities and polyphasic or complex polyphasic motor unit potentials in bilateral lower extremity muscles tested including the bilateral iliopsoas and gluteus maximus muscles. Abnormal spontaneous activities were observed in the right L4/5 and L5/S1 paraspinal muscles. Several subsequent electrodiagnostic studies suggested axonal injury in both lower extremity nerves with predominant involvement in the distal nerves (see Fig. 17-4). In follow-up laboratory tests, aspartate transaminase (AST) and alanine transaminase (ALT), which were normal at admission, were significantly elevated to 334 U/L (nL< 45) and 141 U/L (nL < 50), respectively, on the second admission day, were sustained for several days, and subsequently returned to normal levels two weeks after the onset of symptoms. Muscle enzymes, lactate dehydrogenase (LDH) and creatine phosphokinase (CPK), which was performed 17 days after onset of symptoms, were 765 U/L (nL < 450) and 68 (nL < 52), respectively, and then were normalized. After rehabilitation, he could walk with a cane 4 months following the onset of lower extremity weakness.
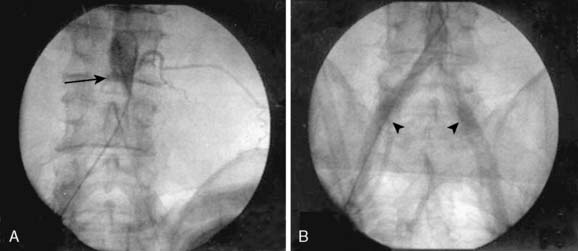
Figure 17-2 Intraoperative aortogram using a C-arm showed that (A) the injected dye stagnated in the distal abdominal aorta (arrow); (B) after embolectomy using balloon catheter, blood flow was restored from abdominal aorta to both femoral arteries (arrowheads).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








