Acute Spinal Cord Syndromes
Acute Spinal Cord Syndromes
Natalie R. Weathered
Noam Y. Harel
INTRODUCTION
Patients presenting with acute spinal cord syndromes represent true neurologic emergencies. Pathologic damage to the cord is usually incomplete. Therefore, there is opportunity to salvage (and peril of losing) vital cord tissue and function over the ensuing minutes and hours after presentation. As with other neurologic presentations, clinicians must first localize and then differentiate the type of damage in order to initiate the most effective interventions.
SPINAL CORD ANATOMY
To aid with localization, recall that the caudal spinal cord segments do not align with the vertebrae bearing the same names. The spinal cord ends around L1, with the roots of the cauda equina below that vertebral level. Additionally, within the cervical cord, the spinal roots exit the spinal canal above the associated vertebral level except for root C8, which exits between C7 and T1. Thereafter, each spinal root exits below the corresponding vertebral body.
MOTOR SYSTEM
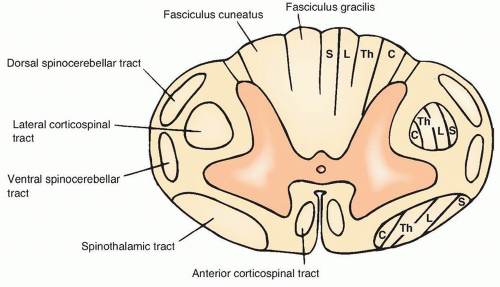
The majority of the corticospinal tract, mediating a large proportion of our volitional limb movements, decussates in the medulla before descending in the contralateral lateral corticospinal tract. The minority of motor axons that do not decussate within the medulla form the anterior corticospinal tract. The lower motor neurons, receiving input from corticospinal fibers as well as segmental interneurons, reside within the ventral horn (
Fig. 16.1).
SENSORY SYSTEM
Afferent sensory fibers from the dorsal root ganglia enter the spinal cord at the dorsal horn. From there, their course depends on the type of modality being transmitted.
Pain and Temperature
These fibers travel rostrally within Lissauer tract for one or two spinal segments before synapsing within the dorsal horn and crossing to the contralateral anterolateral system. The anterolateral system is composed of the anterior spinothalamic tract, which carries crude touch sensory fibers, and the lateral spinothalamic tract, which carries pain and temperature fibers.
Vibration, Proprioception, and Two-Point Discrimination
These fibers travel within the ipsilateral dorsal columns to the gracilis and cuneatus nuclei of the lower medulla. Axons from the legs (fasciculus gracilis) are pushed medially by entering axons from the arms (fasciculus cuneatus) (see
Fig. 16.1).
AUTONOMIC SYSTEM
Sympathetic
Sympathetic preganglionic neurons are located within the inter-mediolateral nucleus of the thoracic and upper lumbar (L1-L2) spinal cord. Their axons exit via the ventral roots and synapse on the postganglionic sympathetic neurons in the paravertebral ganglia (the “sympathetic chain ganglia”) or the prevertebral ganglia.


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access






