8 Adult and infant brains react differently to hypoxia and ischemia. In general, infant brains are more resistant than those of adults; hypoxic-ischemic lesions have a different distribution in infants and adults reflecting an age-related differential (selective) vulnerability to such insults (Fig. 8.1). Because of the brain’s immense metabolic demands, after the onset of ischemia levels of brain glycogen, glucose, ATP and phosphocreatine plummet and are often depleted within 10 min of the acute event. After 15 min of cardiac arrest, up to 95% of the brain may be damaged. Primary respiratory arrest (e.g. due to aspiration, anaphylaxis, or airway trauma) may cause transient brain dysfunction, but less severe damage than ischemia. Optimal brain function and respiration are dependent upon the availability of glucose; however, the neuropathology of hypoglycemic brain injury differs from that due to hypoxia-ischemia. 8.1 Regions of selective vulnerability to hypoxic–ischemic damage are different in the adult and infant brain. Lesions may be considered as either acute/subacute or chronic. Acute/subacute lesions include the following: 8.2 Coronal section through a nonperfused (‘respirator’) brain.
Adult hypoxic and ischemic lesions
TERMINOLOGY
PATHOPHYSIOLOGIC CONSIDERATIONS
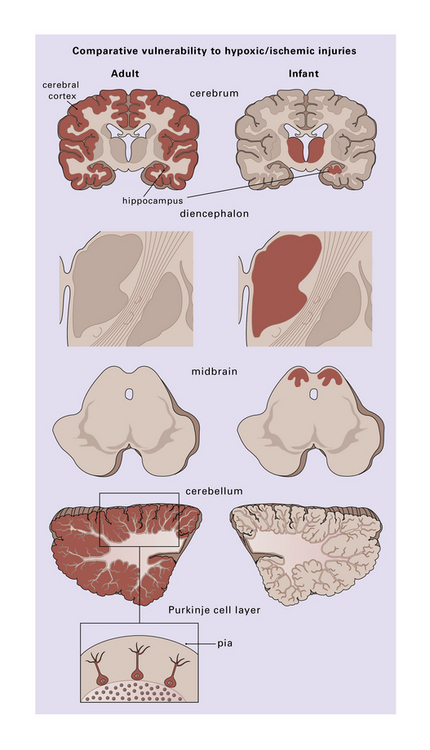
Those regions most susceptible to such an insult are colored in the diagram, though individual cases may show much significant variation. Inset (lower left) emphasizes the observation that cerebellar Purkinje cells are especially at risk during hypoxia.
PATHOLOGY
MACROSCOPIC APPEARANCES
 Precursors of cystic infarcts – especially in watershed territories.
Precursors of cystic infarcts – especially in watershed territories.
 Cortical laminar necrosis (or, in extreme cases and if hypoxia is severe and prolonged, pancortical necrosis). In rare instances with prolonged survival, pancortical necrosis may be associated with calcification.
Cortical laminar necrosis (or, in extreme cases and if hypoxia is severe and prolonged, pancortical necrosis). In rare instances with prolonged survival, pancortical necrosis may be associated with calcification.
 Patchy gray discoloration of cortex, with blurring of the gray-white matter interface – an appearance almost identical to that of subacute infarction.
Patchy gray discoloration of cortex, with blurring of the gray-white matter interface – an appearance almost identical to that of subacute infarction.
 Bright pink color and edema – after acute CO poisoning.
Bright pink color and edema – after acute CO poisoning.
 Generalized dusky discoloration and softening – the appearance of ‘non-perfused’ brain (Fig. 8.2).
Generalized dusky discoloration and softening – the appearance of ‘non-perfused’ brain (Fig. 8.2).
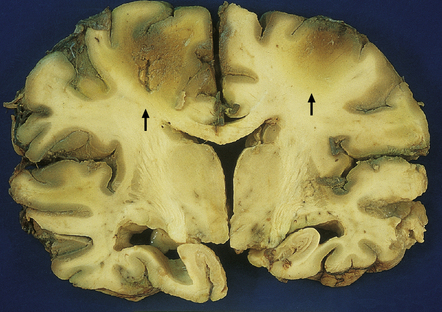
The brain is edematous with focally accentuated gray-brown discoloration throughout the cortex and extending into the subcortical white matter, most notably in the watershed regions (arrows) between the perfusion territories of the middle and anterior cerebral arteries.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Adult hypoxic and ischemic lesions
Only gold members can continue reading. Log In or Register to continue
































