32 Anterior Cervical Corpectomy
I. Key Points
– Anterior cervical corpectomy is a safe and effective technique for decompression of the ventral cervical spinal cord.
– The surgical approach and exposure for corpectomy are similar to the case for the more common anterior cervical discectomy (see Chapter 33).1
II. Indications
– Generally corpectomy is indicated when there is ventral spinal cord compression and discectomy is inadequate for decompression.
• Degenerative conditions, such as spondylotic myelopathy in which ventral spinal cord compression is not restricted to the disc level and/or is complicated by cervical kyphosis
• Tumor infiltration of the vertebral body causing vertebral body collapse and spinal cord compression
• Traumatic cervical spine injury, such as a teardrop fracture with associated spinal cord compression from retropulsion of vertebral body fragments and spinal instability
• Osteomyelitis with epidural abscess and concomitant ventral spinal cord compression
• Ossification of the posterior longitudinal ligament
III. Technique
– Intubation via fiberoptic technique, whether awake or asleep, is safer in cases with significant cervical spinal cord compression, myelopathic signs, myelomalacia, and/or cervical instability.
– Awake fiberoptic intubation allows for neurologic assessment immediately following intubation to assess for changes in neurologic function.
– Tape the endotracheal tube away from the side of surgical incision.
– Steroid administration preoperatively or intraoperatively lacks scientific support.
– Neurologic monitoring is prudent during operations on myelopathic patients.
– Some authors routinely use 8 to 10 lb of traction with Gardner-Wells tongs or chin strap craniocervical traction to increase disc space distraction.
– Place patient supine on the operating table.
• Pressure points should be padded, especially the ulnar nerve.
• A roll between the scapulae may improve lordosis and access to the level of interest. In patients with myelopathy, neck extension must be avoided.
• Shoulders should be taped down to allow for fluoroscopic visualization of the level of interest; however, excessive traction can injure the brachial plexus.
– Localize, with fluoroscopy or using external landmarks, the approximate level of incision along the neck.
– The surgeon may approach the anterior cervical spine from the right or left side; the left-sided approach theoretically involves less risk to the recurrent laryngeal nerve.2
– The incision may be made transversely or longitudinally depending on the number of levels involved and surgeon preference.
– After incision, identify the platysma beneath the subcutaneous layer, and divide it sharply in a transverse or longitudinal fashion.
• Dissecting under the platysma superiorly and inferiorly allows for better mobilization of the tissues.
– Identify the medial border of the sternocleidomastoid (SCM).
– Using Metzenbaum scissors, dissect in the areolar plane between the SCM and the medial structures.
• The carotid artery should be palpated to ensure that the trajectory of dissection is correct.
– Using a hand-held retractor, retract the medial structures from the SCM to expose the prevertebral fascia.
– Incise the fascia to expose the cervical spine; use Kittners to sweep the prevertebral fascia superiorly and inferiorly.
– Use a spinal marker in the vertebral body (and not the disc) to confirm the level with x-ray or fluoroscopy image.
– With electrocautery or periosteal elevator, dissect the longus colli laterally from their midline attachments.
– Place self-retaining retractors and deflate the cuff of the endotracheal tube to minimize esophageal/tracheal edema.
– Caspar pins may be placed into the vertebral bodies above and below the level of interest, with distraction then applied.
– The discs above and below the level of interest should be incised and removed with curettes and pituitary rongeurs.
– When necessary, anterior osteophytes can be removed with a rongeur.
– A burr can be used to thin the vertebral body to the posterior longitudinal ligament (PLL).
– The PLL is carefully pierced with a small hook or curette.
– A small Kerrison rongeur (1 or 2 mm) can then be used to lift the PLL away from the dura and complete the decompression.
– Lateral decompression (foraminotomy) is generally completed at the level of the uncovertebral joint. The uncus can be thinned with a burr and then removal is completed with a microcurette or Kerrison rongeur (Fig. 32.1).
– A strut graft or cage with autograft, allograft, or bone graft substitute material is placed into the defect after contouring of the vertebral body end plates.
– An anterior plate can be used to enhance fusion and prevent graft migration. If possible, multiple points of screw fixation should be established. Posterior instrumentation does, however, provide greater stability and may be required.
– Some authors recommend rigid anterior fixation to enhance rigidity and reduce graft subsidence; others argue that variable plates and screws may enhance fusion by dynamically loading the graft (Wolf’s law). Data in support of either approach are limited to theoretical considerations and retrospective studies.3,4
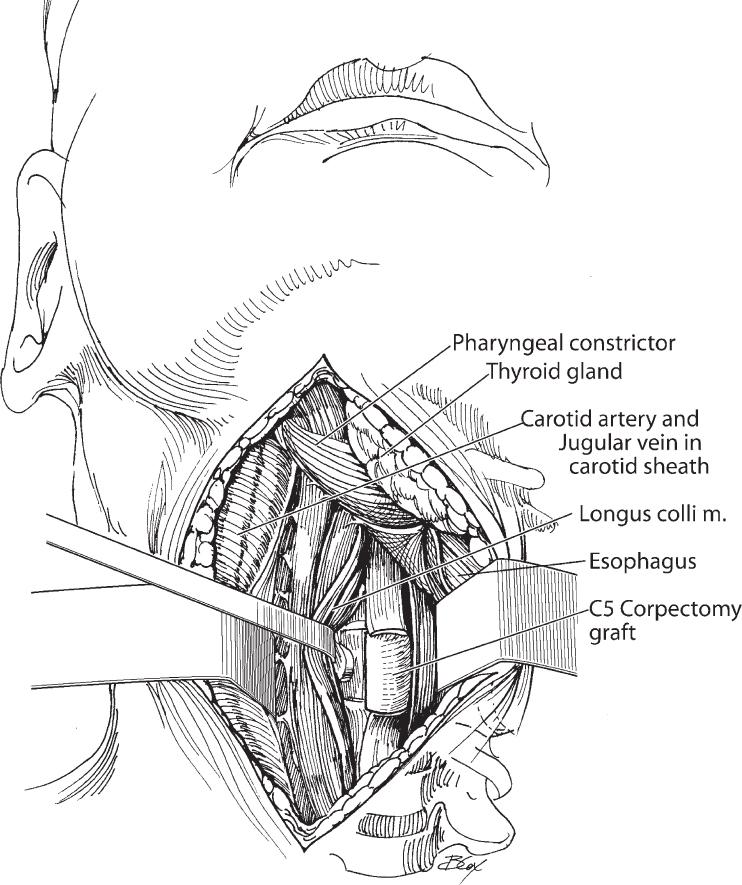
Fig. 32.1 Anterior view of the surgical field after single-level corpectomy in the cervical spine.
IV. Complications
– Wound infection
– Transient hoarseness
• Reduce risk by reducing endotracheal cuff pressure.
• Avoid dissection into the carotid sheath.
• Some surgeons advocate a left-sided approach to avoid risk of recurrent laryngeal nerve injury.
– Permanent hoarseness
– Transient or permanent dysphagia
– Nerve root or spinal cord injury5
– Acute airway obstruction from swelling or hematoma
• Immediately stabilize the airway and intubate.
• Open the wound at the bedside to allow for decompression of the hematoma and thereby ease intubation in an emergent setting.
– Cerebrospinal fluid (CSF) leak
• Extremely difficult to close primarily
• Cover with fibrin glue or dural sealant.
• Place lumbar drain to divert CSF if there is concern about the risk of persistent drainage.
– Vascular injury
• Vertebral artery
 The vertebral artery lies lateral to the uncovertebral complex and is often surrounded by a collection of veins.
The vertebral artery lies lateral to the uncovertebral complex and is often surrounded by a collection of veins.
 Inadvertent injury can lead to massive bleeding.
Inadvertent injury can lead to massive bleeding.
 In the event of injury, the surgeon must immediately administer tamponade to the bleeding, usually with the aid of Gelfoam (Pfizer, New York) or another hemostatic agent. The vessel can be repaired primarily if visualized, or ligated surgically with low risk of neurologic sequelae.6,7
In the event of injury, the surgeon must immediately administer tamponade to the bleeding, usually with the aid of Gelfoam (Pfizer, New York) or another hemostatic agent. The vessel can be repaired primarily if visualized, or ligated surgically with low risk of neurologic sequelae.6,7
 An emergent angiogram should be considered to rule out vertebral artery dissection and may require vertebral artery embolization.
An emergent angiogram should be considered to rule out vertebral artery dissection and may require vertebral artery embolization.
 The artery can be sacrificed with little consequence if it is nondominant; sacrifice of the dominant vertebral artery has a higher incidence of ischemic injury to the brain stem.6
The artery can be sacrificed with little consequence if it is nondominant; sacrifice of the dominant vertebral artery has a higher incidence of ischemic injury to the brain stem.6
– Graft dislodgment/instrumentation failure
• Graft dislodgment may indicate pseudarthrosis, hardware failure, infection, or a combination of factors.
• Of primary importance is airway stablization; if there is significant tracheal compression, emergent intubation and reoperation may be required.
• Revision of the graft may include the use of autograft, such as iliac crest, and posterior cervical instrumentation and fusion to supplement the anterior construct.
V. Postoperative Care
– After a prolonged procedure involving concern for anterior soft-tissue swelling, consider keeping the patient intubated for 24 to 48 hours (until able to breathe around deflated airway cuff).
– Consider external immobilization of the cervical spine.
– Patients with myelopathy and gait unsteadiness may benefit from physical and occupational therapy evaluations.
– Ensure that the patient is tolerating oral intake and swallowing normally prior to discharge.
VI. Outcomes
– The goals of decompressive corpectomy are neurologic preservation, cervical spine stabilization, and/or reduction of deformity.
– Available outcomes studies are limited in their retrospective nature, but indicate excellent technical results (greater than 98% fusion rate) and improvement in radicular and myelopathic symptoms in 86%.8
– Even in patients with severe myelopathy resulting in a bedridden or wheelchair-bound condition, clinical outcomes showed improvement in over 60% of patients who underwent surgery.9
VII. Surgical Pearls
– Identify the location of vertebral artery on preoperative imaging studies.
– Avoid extension of the cervical spine during positioning.
– Generous dissection of the longus colli muscle allows better identification of midline, proper placement of retractor blades underneath the muscle fibers, and decreased pressure on vascular structures laterally or esophagus and trachea medially.
– Begin decompression with discectomy cranial and caudal to the intended corpectomy. This will assist in identification of the appropriate depth and width (uncus to uncus) of corpectomy.
– When the PLL is severely adherent, dissociation of the PLL from the adjacent structures, thus eliminating its constrictive effect on the spinal cord and preventing thecal sac manipulation, is the primary goal. Removing the PLL entirely becomes a secondary goal if it can be safely achieved.10
Common Clinical Questions
1. True or false: The fusion rate after anterior cervical corpectomy increases with augmented posterior fixation, especially after two- and three-level corpectomies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







