INTRODUCTION
Anxiety is an adaptive emotional state related to anticipation of threat; it can encompass fearful thoughts, symptoms of physiologic arousal, and preparation for fight or flight. Anxiety disorders are characteristic syndromes of maladaptation to various types of anticipated threat. Examples include dangers from predators, interpersonal conflicts, germs, and other hazards. Anxiety disorders are distinguished from mild episodes of anxiety by their persistence and intensity and also by the diagnostic requirement that they cause marked distress or impairment in functioning.
Anxiety disorders have historically included panic disorder, agoraphobia, specific phobias, social anxiety disorder, generalized anxiety disorder, obsessive-compulsive disorder (OCD), acute stress disorder, and posttraumatic stress disorder (PTSD). The recent revision of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), places OCD in a separate category of obsessive-compulsive and related disorders and PTSD in a separate category of trauma- and stressor-related disorders, in recognition of their unique features. Two disorders previously categorized as childhood disorders, separation anxiety disorder and selective mutism, are now also recognized as anxiety disorders that can persist into adulthood.
Anxiety and anxiety disorders may co-occur with neurologic disease through a variety of mechanisms. Neurologic disease processes may cause anxiety symptoms directly by dysregulating function of brain circuits that subserve anxiety. Alternatively, primary neurologic illnesses may lead to anxiety via psychological mechanisms as when visible signs of a movement disorder lead to embarrassment and social anxiety or when an uncertain or poor prognosis leads to anticipatory anxiety. A primary anxiety disorder or its treatment may generate neurologic manifestations, such as syncope secondary to hyperventilation in panic disorder, or a seizure due to abrupt discontinuation of a benzodiazepine. Neurologic and psychiatric conditions may also co-occur secondary to another causal agent as when combat trauma leads to both traumatic brain injury (TBI) and PTSD.
EPIDEMIOLOGY
The historical category of anxiety disorders constitutes the most common type of psychiatric disorder with a lifetime prevalence of over 25%. Anxiety disorders are more common in women by a 2:1 ratio, have an age of onset before 30 years in most cases, and tend to be chronic. Community prevalence rates for individual anxiety disorders range from 5% to 12% for social anxiety disorder and specific phobias to 1% to 2% for panic disorder and OCD with intermediate rates for PTSD and generalized anxiety disorder.
PATHOBIOLOGY
The neural circuits, neurochemistry, and behaviors mediating human anxiety share features with neural systems that mediate withdrawal responses to aversive stimuli across species. In humans, these responses incorporate higher cortical functions such as anxious anticipation and adaptations based on life experiences and culture. Twin studies show heritability of specific anxiety disorders in the range of 10% to 60%, but findings for individual genes explain only very small proportions of the overall risk. Environmental risk factors for anxiety disorders include early childhood trauma and acute stressors, such as interpersonal loss.
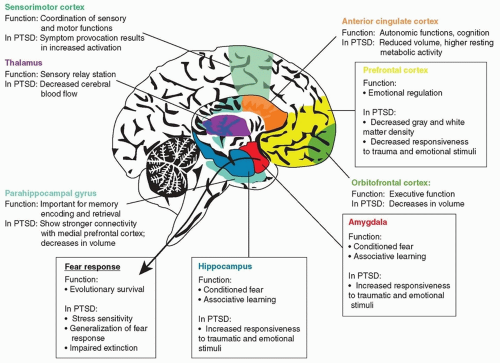
Studies in rodents and humans have implicated central nervous system (CNS) fear circuitry, including the amygdala, hippocampus, and prefrontal cortex, in the development and maintenance of conditioned fear; this circuitry is activated when persons with social anxiety disorder, specific phobias, or PTSD are exposed to fear-inducing stimuli (
Fig. 150.1). Anxiety disorders also have been shown to be associated with dysfunction of several neurotransmitter systems, including serotonin, norepinephrine,
γ-aminobutyric acid (GABA), and glutamate. Dopamine dysfunction has also been reported, and elevated rates of panic disorder, generalized anxiety disorder, and social anxiety disorder have been reported in Parkinson disease. Sympathetic nervous system and hypothalamic-pituitary axis abnormalities have been found across anxiety disorders. Panic disorder has been associated with hyperventilation, hypocapnia, and disordered CO
2 regulation.
The pathobiology of OCD shows some differences from other anxiety disorders. Anatomic and brain imaging evidence suggest hyperactivity in a circuit involving the orbitofrontal cortex, basal ganglia, and thalamus. Acquired lesions in the corticostriato-thalamic circuit, parietal and temporal cortex, cerebellum, and brain stem have been reported to induce compulsivity. OCD has been associated with other neurologic conditions involving the basal ganglia, such as Tourette syndrome, Huntington disease, and Sydenham chorea.
CLINICAL FEATURES
Anxiety disorder patients may present with anxiety, avoidance, physical symptoms, secondary depression, or substance abuse. Complaints of anxiety should be assessed with respect to symptoms and cognitions, frequency and intensity, environmental precipitants, avoidance, and interference with functioning. Some anxiety disorder features can occur across these disorders. Anticipatory anxiety refers to apprehension in anticipation of a feared situation and may include worry, difficulty concentrating, or physical symptoms. Anxiety disorders are often marked by a failure of the habituation that normally occurs during continuing exposure to a feared situation. A panic attack is defined by intense fear that reaches a peak in minutes and includes a group of physical anxiety symptoms, often with feelings of unreality, dizziness, paresthesias, dyspnea, and fear of dying. Phobic avoidance involves excessive avoidance of circumscribed feared situations, and it is often the most directly disabling of anxiety disorder features.
Anxiety often leads to symptoms of depression, so anxious patients should be evaluated for depressed mood, loss of pleasure, change in weight, sleep disturbance, fatigue, poor concentration, and suicidal ideation. Substance abuse is also common in anxiety disorder patients and may be either a precipitant of anxiety or a response to it. People with anxiety disorders are usually aware that the symptoms are related to an excessive or unrealistic reaction on their part, and in this way, they differ from patients with psychotic disorders with delusional fears.
Anxiety disorders may interact with other medical conditions so that patients with asthma may also experience dyspnea related to panic attacks, and individuals with disorders that attract unwanted attention (e.g., essential tremor) may be impaired by excessive fear of embarrassment as in social anxiety disorder. Medical conditions that can directly mimic anxiety symptoms include hyperthyroidism; hyperparathyroidism; cardiac arrhythmias; reactions to caffeine, cocaine, or marijuana; pheochromocytoma; and vestibular dysfunction.


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access