A. Structural causes
Structural etiologies of altered mental status can be caused by trauma, anoxic-ischemic injury, hemorrhages, infarctions, neoplasms, and hydrocephalus. Trauma can result in hemorrhagic or nonhemorrhagic brain contusions or diffuse axonal injury, which produce varying degrees of encephalopathies. Patients with long-bone fractures from polytrauma can develop cerebral fat embolization manifesting as a transient encephalopathy with or without seizures and focal neurologic deficits lasting up to a month. While contusions and hemorrhages are easily identifiable on a noncontrast head computed tomography (CT), diffuse axonal injury and fat emboli are better visualized by magnetic resonance imaging (MRI) and should be considered when patients have persistent encephalopathy following trauma. Brain hemorrhages (intraparenchymal, subdural, epidural, or subarachnoid), infarctions, or tumors located in both cerebral hemispheres, the thalami, or brainstem can lead to an acute confusional state or varying degrees of stupor or coma. Lesions located in one cerebral hemisphere can be large enough to cause tissue shift and compression of the contralateral hemisphere, thereby producing an acute confusional state associated with focal neurologic deficits. In other cases, a lesion may be strategically located (i.e., in the frontal or temporal lobes) such that it produces acute confusion in the absence of significant edema. Carcinomatous meningitis, the diffuse infiltration of neoplastic cells into the meninges, may occur in the setting of leukemias, lymphomas, malignant melanoma, and lung or breast cancers. Patients with carcinomatous meningitis often present with headache, neck stiffness, and cranial nerve abnormalities because of direct infiltration of cancer cells. Severe hypoxemia or global reductions in cerebral blood flow can also cause irreversible injury because brain regions with high metabolic demand such as the basal ganglia and motor and occipital cortices suffer anoxic-ischemic injury.
B. Metabolic causes
“Metabolic encephalopathy” is one of the most common reasons for neurologic consultation in the hospital. Any acute organ dysfunction can produce an acute confusional state, and the severity varies depending on the degree of organ dysfunction and the rapidity over which it developed. For example, when renal failure develops very slowly over many months, the brain is often able to adapt, whereas when it develops suddenly over days to weeks, accumulation of toxins can lead to severe confusion or even coma. The exception is chronic liver failure, where patients may develop acute episodes of encephalopathy periodically without a corresponding acute decline in liver function. The most common causes of “metabolic encephalopathy” by far are liver or kidney dysfunction. Other causes include diabetic ketoacidosis and nonketotic hyperglycemic state, hyper- or hypothyroid states, or major electrolyte imbalances or acid–base derangements. Generally, encephalopathy resulting from metabolic derangements resolves with correction of the underlying organ injury, acid–base imbalance, and endocrine or electrolyte derangement. It is acceptable to rapidly correct the majority of these conditions (when possible); however, clinicians should exercise caution in the setting of an acute on chronic hyponatremia where rapid correction may precipitate a frequently irreversible osmotic demyelination syndrome otherwise known as central pontine myelinolysis.
C. Nutritional causes
Alcoholic patients are prone to several nutritional deficiencies, some of which may lead to a subacute or chronic cognitive decline. Thiamine deficiency, specifically, can produce an acute confusional state known as “Wernicke’s encephalopathy” if patients are given glucose before thiamine repletion. Thiamine supplementation is therefore recommended before glucose administration in any patient with suspected or known chronic alcohol use as well as any patient with risk factors for nutritional deficiencies such as those with cancer, prior gastric bypass, inflammatory bowel disease, or eating disorders in order to avoid irreversible injury to the mamillary bodies. Wernicke’s syndrome may variably result in a constellation of symptoms including acute encephalopathy, ophthalmoplegia, and ataxia. The full triad is rare.
D. Toxic causes
Toxic causes of encephalopathy include intoxication or withdrawal syndromes, drug–drug interactions, or drug toxicity in the setting of reduced renal or hepatic function. As discussed in the pathophysiology section, certain drugs have the potential at therapeutic levels to cause acute confusional states because of their alteration of neurotransmitter concentrations. While some drugs are more likely offenders than others, any drug is a potential culprit when it becomes supratherapeutic or when combined with the wrong drug.
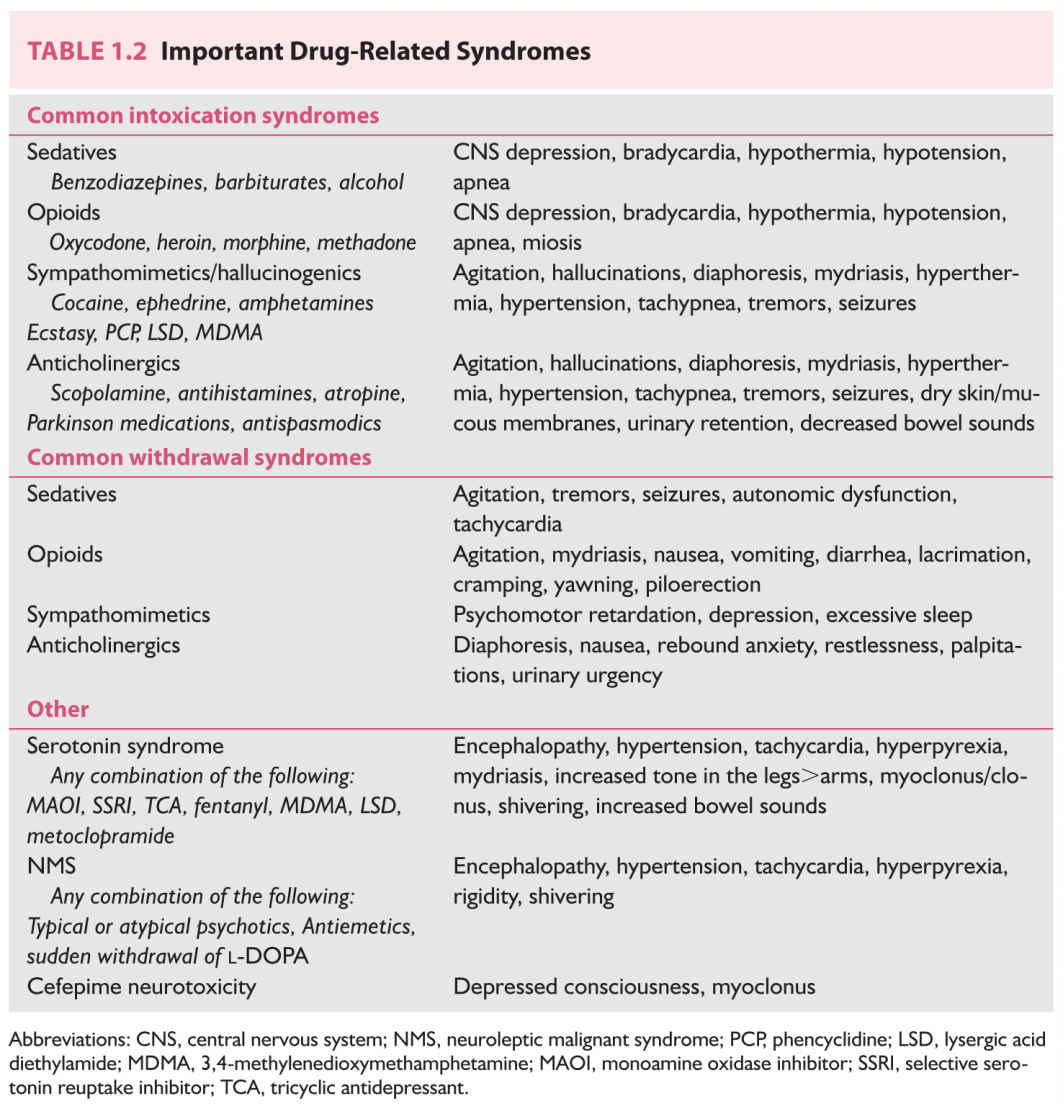
When patients present for evaluation of acute encephalopathy, intoxication with a drug of abuse should be considered. When the encephalopathy develops after admission the patient may be withdrawing from a regularly used drug or alcohol. Urine and serum drug screens can detect most commonly used drugs of abuse; however, newer synthetic agents including bath salts and synthetic marijuana may not be detectable by conventional drug screens. Alcohol intoxication can be assessed through odor and serum alcohol levels but alcohol withdrawal symptoms are easily overlooked. Intoxication and withdrawal syndromes as well as certain drug interactions and toxicities may be life threatening and therefore require prompt recognition and timely intervention. Signs and symptoms of common culprits are listed in Table 1.2.
Neuroleptic malignant syndrome (NMS) and serotonin syndrome may develop during hospitalization of a patient on psychiatric medications. Both syndromes share common features including hyperpyrexia, rigidity, tachycardia, hypertension, and encephalopathy but important differences exist. Fentanyl and antiemetics are common precipitants of a serotonin syndrome in the hospital when they are initiated in patients receiving selective serotonin reuptake inhibitors.
Antineoplastic and immunosuppressive agents may potentiate a posterior reversible encephalopathy syndrome (PRES). PRES is a clinicoradiographic syndrome thought to be due to endothelial dysfunction and vasogenic edema preferentially affecting the posterior cerebral regions. The primary triggers include acute hypertension or blood pressure swings, sepsis, autoimmune conditions, cytotoxic medications (including antineoplastic and immunosuppressants), and pre-eclampsia or eclampsia. The majority of patients recover completely within 2 to 8 days. However, severe cases of PRES can lead to irreversible brain injury because of infarcts and hemorrhages in the areas of edema.
The most notable antibiotics causing severe encephalopathy are cefepime and metronidazole. In patients with renal impairment, serum and cerebrospinal fluid (CSF) levels of cefepime can approach toxic thresholds to trigger seizures, confusion, myoclonus, and even coma. The pathophysiology of metronidazole-induced encephalopathy is less understood and is thought to occur as a result of modulation of neurotransmitters by the metabolites of metronidazole.
E. Infectious causes
Infections such as meningitis and encephalitis and opportunistic infections such as aspergillosis and toxoplasmosis in immunosuppressed individuals can undoubtedly result in acute confusional states by direct invasion of the brain and severe inflammation. These infections can variably lead to hemorrhages, arterial infarctions as a result of infectious vasculitis, venous ischemia from cerebral venous and dural sinus thrombosis, or abscess formation. Systemic infections, especially sepsis and septic shock, may also provoke robust cytokine storms that result in dysfunction of several cell types and disruption of neurotransmission and calcium homeostasis. Disruptions in blood–brain barrier expose the brain parenchyma to various circulating toxic infectious molecules or to inappropriately metabolized drugs due to concurrent liver or kidney injury. The severity of encephalopathy in sepsis is related to the severity of sepsis. It should be noted that septic encephalopathy can occur in the absence of overt organ injury.
1. Nonconvulsive seizures, nonconvulsive status epilepticus, or postictal state
Nonconvulsive seizures found in up to 8% of critically ill patients, nonconvulsive status epilepticus (NCSE), or postictal states can present as acute confusional states. Nonconvulsive seizures or status epilepticus can be suspected in somnolent or lethargic patients found to have subtle twitching of the face or limbs or the patient may simply appear withdrawn and disengaged. The diagnosis is very challenging and can evade even the most experienced of clinicians.
F. Hypertensive encephalopathy
Sudden spikes of blood pressure due to any cause above the limit of cerebral autoregulation can result in endothelial injury, breakdown of the blood–brain barrier, and subsequent vasogenic edema. Hypertensive urgency and emergency are reversible when identified and managed early; however, delayed recognition can lead to hemorrhages, ischemia, and cerebral edema. It can also precipitate a syndrome of reversible encephalopathy and vasogenic edema, known as PRES (discussed earlier).
G. When no clear cause is identified “delirium”
Patients with any degree of underlying cognitive impairment can easily decompensate in the setting of an acute medical or neurologic insult, a condition known as “beclouded” or “decompensated” dementia. Patients with neurocognitive disorders are at higher risk for development of delirium and may take longer to recover from events such as anesthesia, sedatives, postoperative states, postictal states, and prolonged hospitalizations.
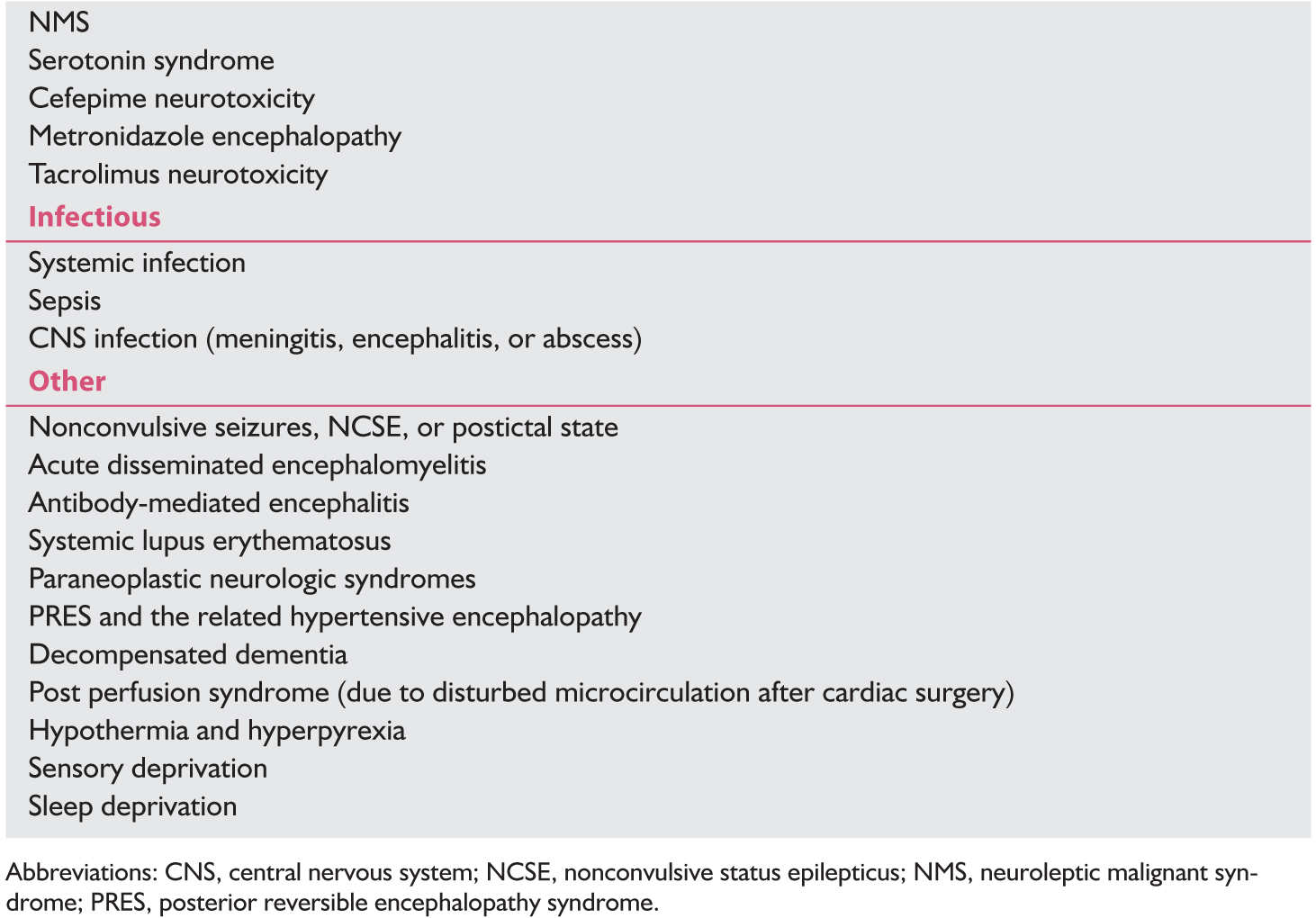
DIFFERENTIAL DIAGNOSIS OF ACUTE CONFUSIONAL STATE
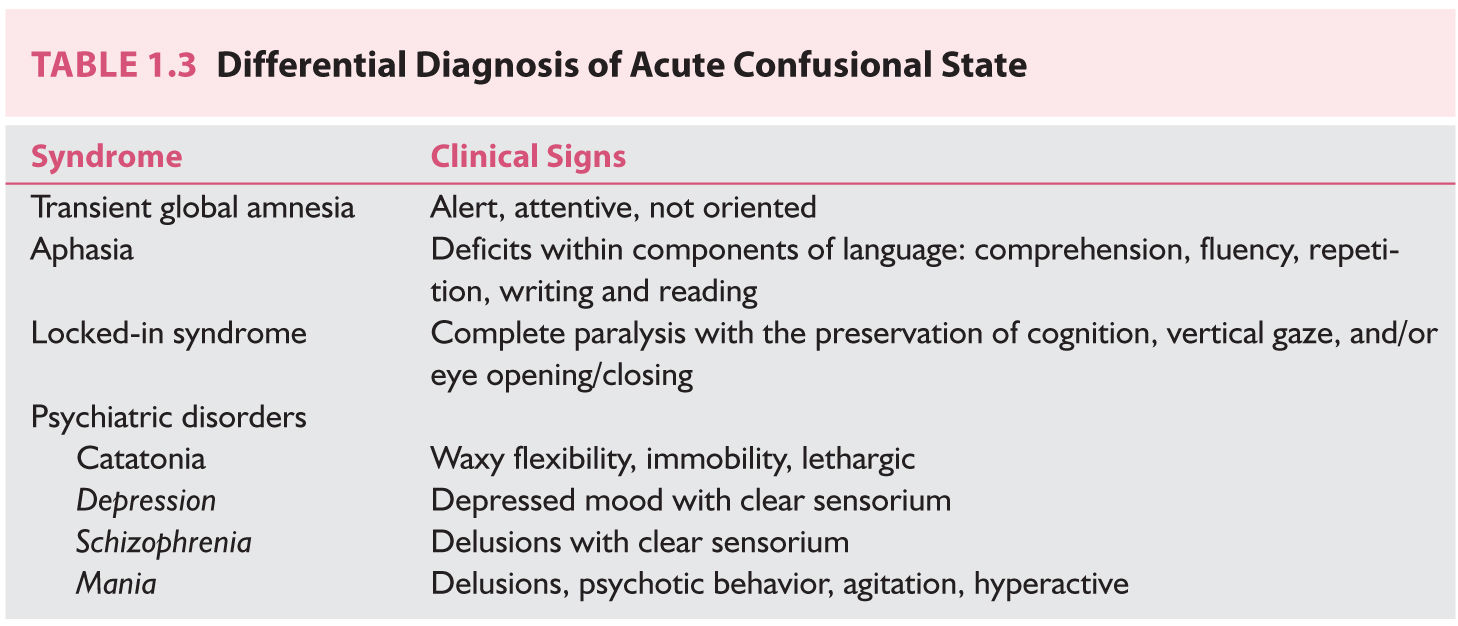
The differential diagnosis of acute confusional state is shown in Table 1.3. Locked-in syndrome should be suspected in an otherwise unresponsive patient who is only able to blink and produce vertical gaze movements. Infarcts affecting the ventral pons disrupt corticospinal, corticopontine, and corticobulbar tracts but spare supranuclear eye movements and the RAS, thus preserving consciousness and vertical eye movements.
Transient global amnesia typically occurs in middle-aged or elderly persons and manifests clinically as an acute episode of amnesia for the present and recent past. Episodes are usually self-limited and last up to several hours. There is no consensus on the cause but hypotheses include a vascular etiology (either arterial or venous), a migrainous phenomenon or cortical spreading depression, seizures, or a psychogenic etiology.
Patients with psychiatric disease can develop acute mania, psychosis, catatonia, or dissociative fugue states. These should be differentiated from the acute confusional states discussed earlier as the management is very different. Catatonia presents as a motionless, apathetic state in which the patient is oblivious or does not react to external stimuli. Patients in this state make little or no eye contact and may be mute and rigid sometimes alternating with excitement, immobility, and waxy flexibility. Catatonia is treated with benzodiazepines, and in refractory cases, electroconvulsive therapy is indicated.
A. Case
A neurology consultation is placed for an elderly individual with progressive agitation and confusion after presenting with a mechanical fall fracturing several ribs and acute kidney injury. He was treated with oxycodone and fentanyl for pain, and subsequently with haloperidol and quetiapine for agitation. His confusion worsens and he begins to develop abnormal involuntary movements. Family recalls a previous admission related to another fall 2 years prior, which was also complicated by confusion and “twitching” and which took several weeks to resolve. Upon a detailed interview of family members, it is discovered that the patient has become slowly withdrawn over several years and occasionally demonstrates a unilateral resting tremor. On examination, he is inattentive, disoriented, and has prominent multifocal asterixis and myoclonus and there appears to be an underlying tremor (Video 1.1)![]() . No focal findings or meningeal signs were identified on examination.
. No focal findings or meningeal signs were identified on examination.
B. Diagnostic approach
Determining the etiology of a patient’s encephalopathy can be challenging. A systematic approach to an acutely altered patient will make the encounter less intimidating. A focused history, followed by an organized medical record review, careful clinical examination, and then prudent selection of diagnostic tests when necessary, including laboratory, imaging, and electrophysiologic studies, is recommended.
C. Brief history
The patient’s history, arguably the most important step in elucidating the etiology of acute confusional state, is commonly sparse. The provider should interview members close to the patient including family members and first responders such as emergency medical staff and emergency room providers. Important questions apart from medical and psychiatric history, medication lists, and prior substance abuse include the following. How abruptly did the confusion begin? It is often enlightening to ask when the patient was last completely normal. Despite being consulted for acute confusion, in many instances this question will bring out a more subacute story of forgetfulness and lapses in judgment. Has the confusion been persistent or fluctuating? Has this happened before? Does the patient have access to drugs or medications of abuse? Has there been any exposure to sick contacts, carbon monoxide, or other potential neural toxins? Have there been any associated fevers or chills? A thorough 14-point review of systems is useful to ensure that all associated symptoms are identified as family members may not think to mention the recent initiation of an herbal supplement to help with their depression, for example, as they may not think it could be related to their presenting complaint.
CLINICAL MANIFESTATIONS
While the level of consciousness may be depressed in an acute confusional state, the hallmark of an acute confusional state is alteration of the content of consciousness and inattention. Attention refers to the ability to focus as well as to sustain and shift focus. Disorientation and deficits in memory, language, perception, and visuospatial ability are also prominent. Autonomic hyperactivity such as tachycardia, hypertension, and hyperhidrosis may accompany delirium; however, their presence should alert the provider to the possibility of acute brain injury (i.e., paroxysmal sympathetic hyperactivity), infection (encephalitis), or a toxidrome (serotonin syndrome or NMS). In delirious patients, agitation can predominate at night and drowsiness through the daytime, sometimes referred to as “sundowning.” Hallucinations may occur as well as significant cognitive deficits. Patients with agitation, hallucination, and restlessness are easily seldom missed. This presentation is termed “hyperactive delirium” and accounts for less than 5% of episodes of delirium. The most common presentation is the so-called “hypoactive delirium,” in which the patient appears withdrawn and lethargic.
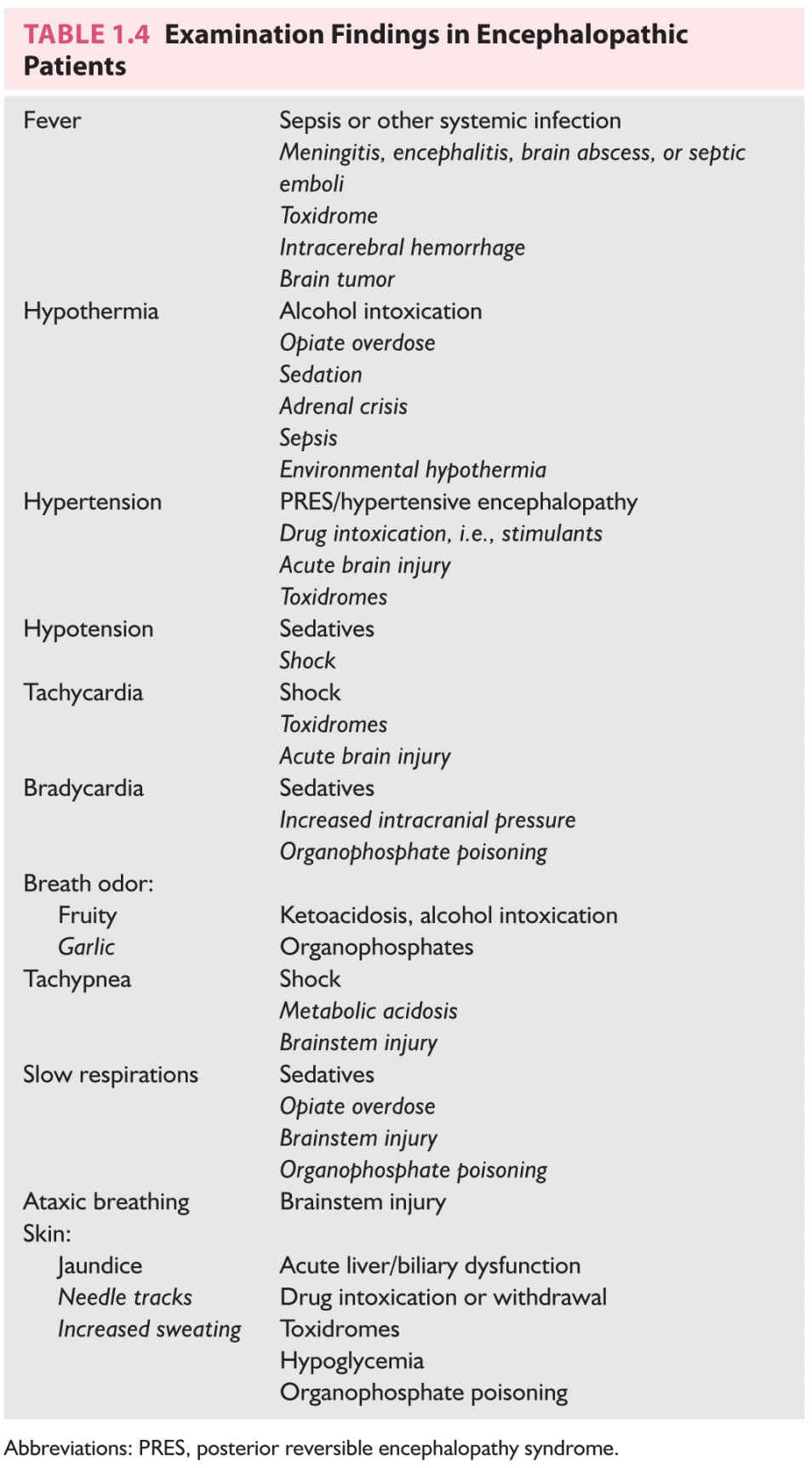
The examination of an encephalopathic patient can be completed within a few minutes by an experienced provider. Certain causes of mental status changes can be discovered solely by thorough examination. The general examination includes an assessment of vital signs, respiratory pattern, and skin as outlined in Table 1.4. A hypersympathetic state manifesting as fever, tachycardia, hypertension, and tachypnea may indicate an early shock state, acute brain injury, or a toxidrome such as a serotonin syndrome or NMS. Hypothermia on the other hand may point toward sepsis, adrenal crisis, or a sedative, opiate, or alcohol overdose. Breath can have a fruity odor in a patient with diabetic ketoacidosis while alcohol intoxication and a garlic odor may indicate organophosphate toxicity. Skin examination may reveal dermatomal rashes or needle tract signs implicating varicella or drug abuse, respectively.
The mental status examination entails assessment of the level of consciousness, attention, orientation, memory, organization of thought, and mood. The level of consciousness can be described as alert, drowsy, somnolent, stuporous, and comatose. An alert individual is spontaneously awake. Drowsy patients require repeated verbal prompting to maintain alertness. A somnolent patient will transiently arouse to physical stimuli, commonly requiring tactile or even nociceptive stimulation, whereas a comatose patient will not arouse to any stimuli. This can be documented as spontaneous eye opening (alert), eye opening to voice (drowsy), eye opening to touch (somnolence), eye opening to pain (stupor), or no eye opening (coma). Attention refers to the ability to focus as well as to sustain and shift focus. Orientation testing should include orientation to patient’s name, location including immediate location (i.e., hospital), city and state, time including day, date, month, year, and season, as well as purpose of hospitalization. Memory tests should be completed with remote history as well as immediate recall. Disordered thinking and emotional lability should also be noted if present.
A careful language examination can help to differentiate an acute aphasia from the tangential and mumbling speech of an encephalopathic or delirious patient. When alert, encephalopathic patients should be able to name simple objects, and repeat and follow simple commands although it may require significant redirection and repetition of the commands to complete this portion of the examination.
Examination of the cranial nerves can alert the provider to the presence of a structural brain lesion but some findings are easily explained by drugs. Mydriatic pupils are usually a result of sedative medications or overdose of anticholinergics but may also reflect a hypersympathetic state as is seen with in serotonin syndrome or NCSE. Miotic pupils on the other hand are most commonly reflective of opiate administration but can also result from sympathomimetic drugs of abuse or a pontine lesion. Bilaterally fixed pupils with absence of all other brainstem reflexes can reflect complete neuromuscular blockade or brain death. A unilaterally dilated pupil should raise concern in an encephalopathic patient as it reflects compression of the third nerve along its pathway, either as a result of a posterior communicating artery (PCOM) aneurysm, cavernous sinus syndrome, or herniation of the uncus of the temporal lobe. When it occurs in an alert patient it may still result from a PCOM aneurysm but is more likely to reflect administration of a topical mydriatic agent such as a scopolamine, antiemetic patch, or aerosolized respiratory medications. Oval pupils may reflect prior ocular surgery, midbrain disease, or increased intracranial pressure.
A forced gaze deviation or a gaze preference can be seen in unilateral hemispheric lesions. A destructive lesion such as an infarct affecting the frontal eye field will result in ipsilateral gaze deviation, whereas an irritative lesion such as an epileptic focus will produce a contralateral gaze deviation at the time of seizure occurrence. An irritative lesion can produce ipsilateral gaze deviation following a seizure. A downward gaze can reflect thalamic or dorsal midbrain injury, acute hydrocephalus, or raised intracranial pressure. Upward gaze is uncommon and poorly localizable. Skew deviation is a vertical misalignment of the eyes resulting from a cerebellar or brainstem injury. Ocular bobbing is rapid downward and slow upward correction that occurs spontaneously in the setting of pontine lesions. Slow downward followed by rapid upward correction is known as ocular dipping, which also localizes to the pons. Roving eyes are spontaneous slow horizontal movements of the eyes and are commonly observed in the setting of encephalopathy when the level of consciousness is depressed. The presence of roving eye movements is nonspecific and simply reflects the depression in the level of consciousness. Nystagmus noted in the primary resting position is frequently indicative of a toxidrome.
The corneal reflex arc may be interrupted by midbrain or pontine lesions. Note that patients who have had prolonged intensive care unit admissions can have scleral edema and patients who routinely use contact lenses will have a depressed corneal reflex.
Tone in a severely encephalopathic patient may be the most important part of the clinical examination. Increased tone throughout all limbs associated with fever can be indicative of a toxidrome such as neuroleptic malignant syndrome or malignant hyperthermia but may also occur as part of paroxysmal sympathetic hyperactivity (in the setting of acute brain injury) or in central nervous system (CNS) infections. When tone is disproportionately increased in the lower extremities when compared with the upper extremities, this suggests a possible serotonin syndrome and other signs should be sought (i.e., tremor-like movements, myoclonus, and increased bowel sounds). Unilateral hypotonia when accompanied by weakness is suggestive of a contralateral hemispheric infarction. Meningismus, Brudzin ski’s, and Kernig’s signs indicate meningeal irritation either by subarachnoid hemorrhage or by meningitis.
When possible, strength can be assessed by asking the patient to flex and extend individual muscle groups. However, when cooperation or level of consciousness is reduced, observation for amplitude, symmetry, and purpose of the movements is very informative. The presence of a restraint only unilaterally, for example, offers a clue to the presence of a hemiparesis. In a patient who is not moving spontaneously, motor response is assessed by administration of a painful stimulus to the nail bed of each extremity. The response may be described as localization, withdrawal/flexion, extension, or absent.
Many adventitious movements occur in encephalopathic patients and should be noted. Patients may have tremor-like movements, which may indicate shivering or low-amplitude clonic movements, myoclonus, spontaneous clonus, or asterixis. Fine motor twitching may suggest nonconvulsive seizures. Asterixis or negative myoclonus is the inability to sustain a motor contraction such as wrist extension or lip puckering. Myoclonus is a sudden involuntary twitch of a muscle. Both asterixis and myoclonus can accompany metabolic derangements such as renal or hepatic failure or may result from drug–drug interactions or drug toxicity such as gabapentin accumulation in the setting of renal disease.
ORGANIZED MEDICAL RECORD REVIEW
An organized review of the medical record often reveals laboratory or vital sign trends, medication combinations, newly initiated medications, previously documented examination changes, or previous hospitalizations with similar symptoms, among other pertinent information. The medical record should be examined in a systematic and organized manner such that important components are not overlooked. Clues to the etiology of encephalopathy can be attained by paying close attention to changes in vital signs or trends, such as a slow increase in the heart rate that may otherwise have gone unnoticed. Such a systematic review should include (1) vital sign review over the duration of the hospitalization, (2) laboratory review over the duration of the hospitalization, (3) review of the medication administration record, (4) review of prior neurologic examinations in the current hospitalization as well as in prior documented notes (to obtain a baseline), (5) and any prior neuroimaging.
In a consultation for altered mental status, the medication administration record may arguably be the most helpful in discovery of the etiology for encephalopathy. A careful review can result in identification of common deliriogenic medications such as anticholinergics in the elderly, high doses of fentanyl in the setting of chronic serotonin reuptake inhibitor use, or cefepime, which may be of concern in a patient with renal failure, to name a few. In addition to the administered medications, assessing for abruptly discontinued outpatient medications during ongoing hospitalization, namely benzodiazepines, may lead to identification of the cause of acute confusional state. Prior documented neurologic examinations may document a facial palsy that the patient’s family had not noted, obviating the need for further evaluation of that finding and prior neuroimaging may explain a previously undocumented subtle hemiparesis.
DIAGNOSTIC TESTING
Tests that are potentially useful in aiding the evaluation of an encephalopathic patient include basic laboratory studies, toxicology studies, imaging, electroencephalography (EEG), and lumbar puncture (LP) for CSF analysis. These studies should be pursued in a judicious fashion rather than as a shotgun approach. Reflexively ordering an MRI, LP, and EEG on every encephalopathic patient does not require any training on the provider’s part. A suggested diagnostic approach can be found in Figure 1.1.
General laboratory studies should include a complete chemistry panel including electrolytes, urea, creatinine, and blood glucose levels. Thyroid function studies, liver function studies, and ammonia levels may be indicated in some patients. In suspected individuals, a blood and urine toxicology screen should be obtained including an alcohol level. Patients with concomitant respiratory illness should have an arterial blood gas sampled to assess for hypercapnia or acidosis. In patients with fever, hypothermia, leukocytosis, subjective chills, or urinary symptoms, a urinalysis and blood cultures should be obtained. Take caution in attributing the cause for alterations of consciousness to mildly abnormal laboratory values. A mild case of urinary tract infection (UTI) or mild hypo- or hypernatremia should conclude the evaluation of encephalopathy only in rare cases such as elderly patients who have a history of acute confusional state associated with previous UTIs. Patients with serious electrolyte derangements, hypoglycemia, or hyperammonemia, on the other hand, may not require additional evaluation. Persistent encephalopathy upon correction of the suspected causal laboratory derangement, or in the presence of focal neurologic signs on examination should prompt further testing.
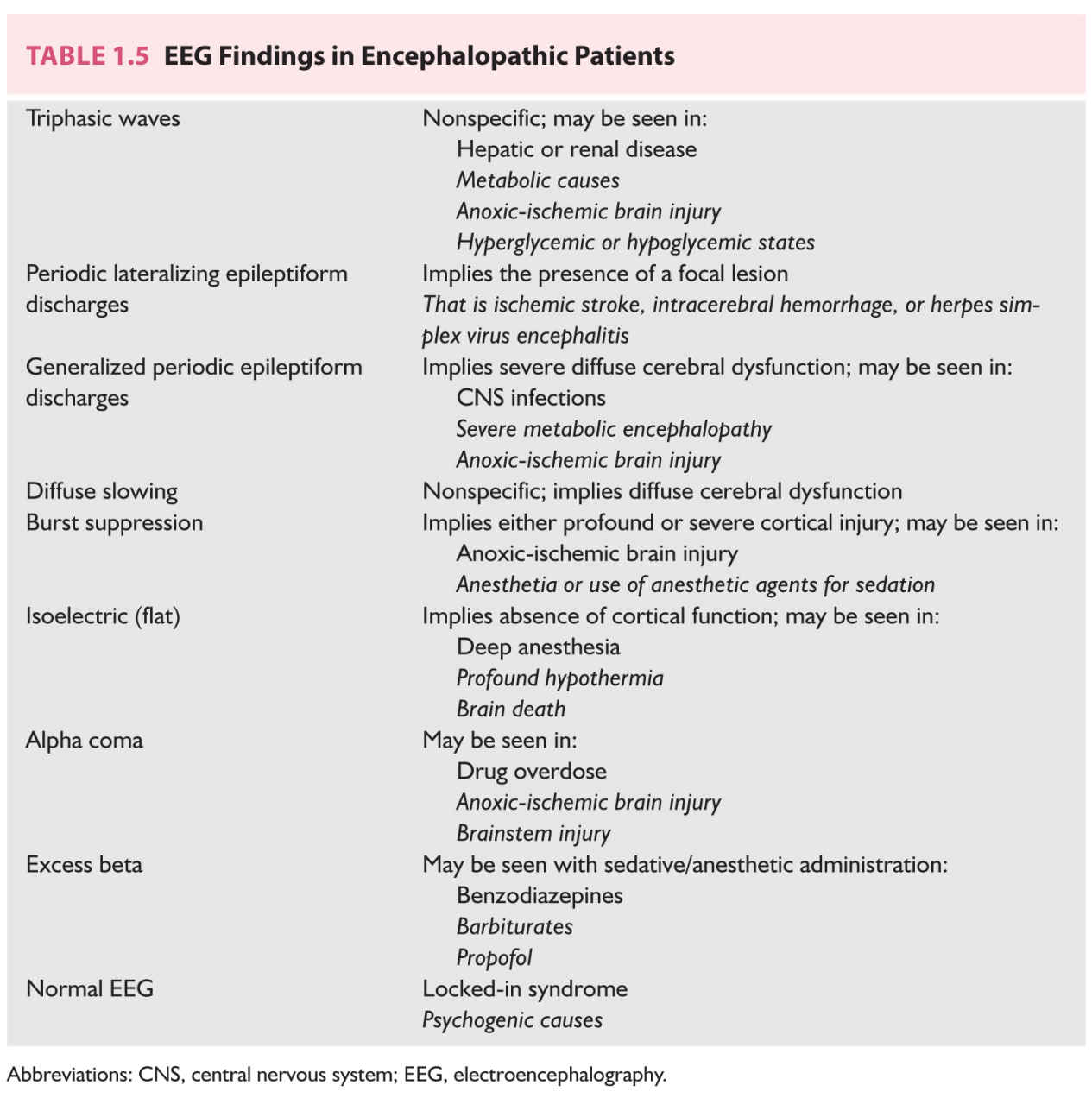
EEG has limited utility in the encephalopathic patient except to exclude nonconvulsive seizures or status epilepticus. Up to 8% of critically ill patients may suffer NCSE. Almost all patients with acute confusional state will have an abnormal EEG with either a posterior dominant rhythm frequency of less than 8 Hz or a relative decrease from an alpha wave of 10 to 12 Hz. As the encephalopathy worsens, the EEG background becomes disorganized, and high-voltage theta and delta activity appears with loss of EEG reactivity at frequencies less than 5 to 6 Hz. Triphasic waves, while classically associated with hepatic encephalopathy, are nonspecific and can be seen in any type of metabolic encephalopathy. Excessive beta activity is typically due to administration of benzodiazepines or anesthetic agents such as propofol. Table 1.5 outlines common EEG findings in encephalopathic patients and their clinical implications.
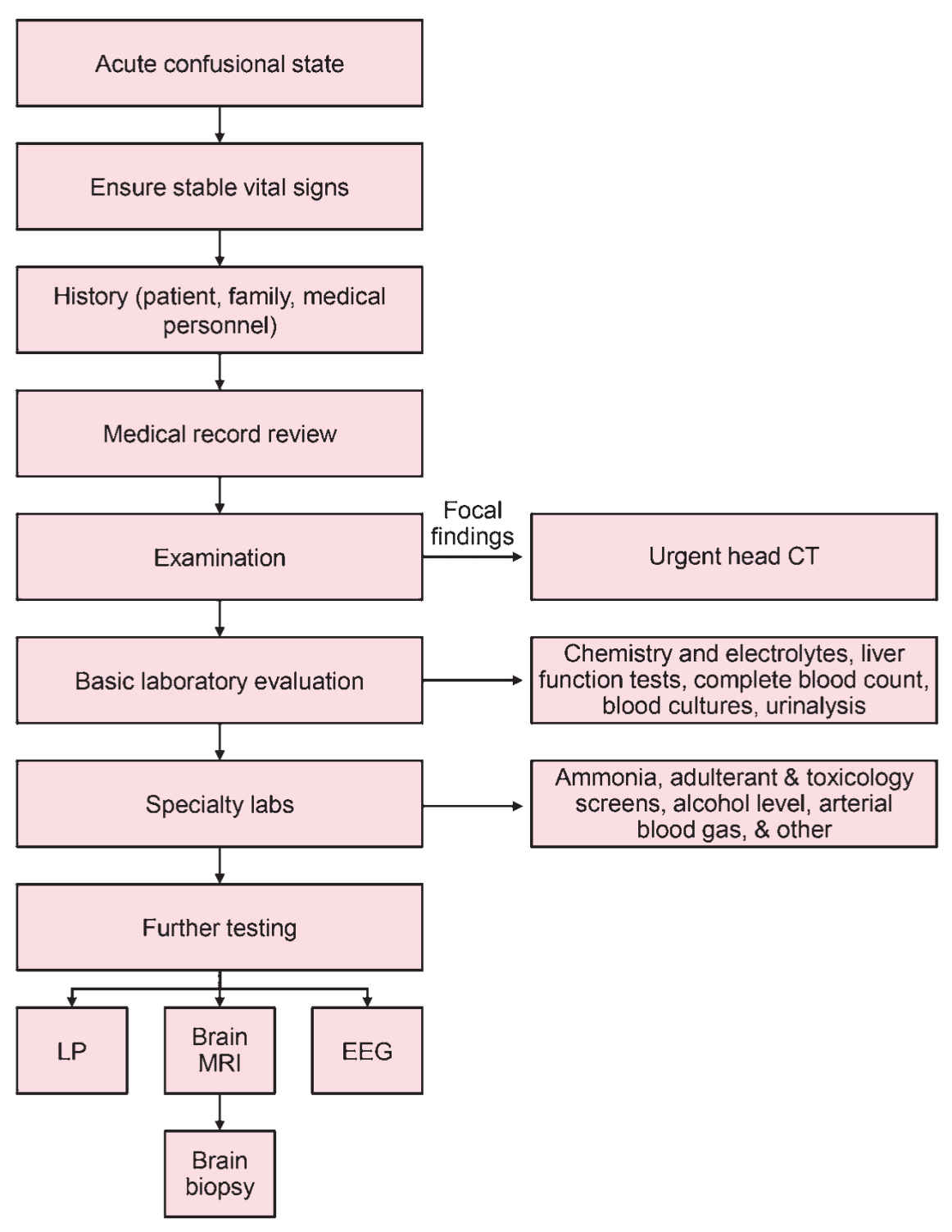
FIGURE 1.1 Approach to evaluation of acute confusional state. CT, computed tomography; EEG, electroencephalography; LP, lumbar puncture; MRI, magnetic resonance imaging.
An LP for CSF analysis should be obtained in any patient with suspected meningitis and encephalitis, or in patients with suspected malignancy to assess for carcinomatous meningitis or paraneoplastic antibodies. Carcinomatous meningitis can occur in patients with lymphoma, leukemia, melanoma, and lung and breast cancers. CSF analysis is also warranted in most immunocompromised acutely encephalopathic patients to assess for opportunistic infections. When LP is performed, the minimum requirements for CSF analysis include cell count, glucose, protein, culture, and gram stain. A serum glucose obtained within the hour the LP is performed allows for calculation of the CSF/serum ratio. Further testing is pursued if the initial tests are abnormal or depending on the clinical question. For example, if a paraneoplastic syndrome is suspected to be the cause of the patient’s acute confusional state, a CSF paraneoplastic panel should be ordered even in the setting of a normal CSF cell count and chemistry.
A noncontrast head CT can identify the majority of structural causes of acute confusional state, including hemorrhage, tumors, infarction, hydrocephalus, and brain edema. An MRI is useful in the evaluation of acutely confused patients with suspected encephalitis, white matter processes (i.e., acute disseminated encephalomyelitis or PRES), brainstem infarctions, Wernicke’s encephalopathy, multifocal lesions such as septic emboli or metastatic disease, or hypoxic-ischemic brain injury, where the CT may be normal.
Patients with acute confusional state but an otherwise normal physical examination and no fever, leukocytosis, or history of seizures, who meet diagnostic criteria for delirium, may not require any additional testing beyond a basic laboratory evaluation and medication review. A period of observation after initiation of reorientation, sleep enhancement, and other management strategies is recommended, with reconsideration of further testing (specifically neuroimaging) if the patient fails to improve over a specified period of time.
MANAGEMENT
Treatment strategies rely strongly on addressing the primary etiology of the acute encephalopathy. Once the etiology is discovered, successful correction of the encephalopathy depends on timely reversal of all contributing factors. For example, dialysis will eventually improve encephalopathy due to uremia; however, the rate of improvement will vary significantly and may be delayed in comparison with correction of the laboratory values. Lactulose administered for treatment of hepatic encephalopathy often readily improves the encephalopathy in most cases; however, delayed recognition and initiation of treatment may lead to permanent cognitive changes. In some instances, no specific contributing acute organ injury, infection, drug, or other etiology can be identified, and in these patients, if criteria for delirium are present, the management is focused on symptom control, maintenance of sleep–wake cycles, and frequent reorientation.
The yield of general nonpharmacologic approaches in the management of a patient with acute confusional state should not be underestimated. A comprehensive interdisciplinary approach includes prevention of aspiration, avoidance of skin breakdown by encouraging progressive mobility, and prevention of urinary retention or ileus. Prevention of sensory deprivation by means of visual or auditory assist devices, and gentle physical contact are several techniques that can easily be undertaken. Sleep enhancement can be requested in which disruptions are minimized (i.e., lab draws and nursing cares) during sleep hours. This helps promote a normal sleep–wake cycle. Familiarization of the patients with their environment by frequent reorientation, use of photographs of loved ones, or the physical presence of family members can aid in reducing behavioral disturbances. Bodily restraints should be used as a last resort in order to ensure patient and staff safety.
The pharmacologic management of behavioral dyscontrol related to acute confusional state primarily consists of antipsychotic agents. Haloperidol and chlorpromazine are typical antipsychotics historically used in the management of delirium. In an emergency where either the safety of the patient or care providers is at risk, haloperidol remains the drug of choice. More recently, atypical antipsychotics with their improved adverse effect profile such as quetiapine, olanzapine, and aripiprazole have been increasingly utilized. These newer agents have fewer extrapyramidal symptoms including akinesia, akathisia, acute dyskinesias or dystonic reactions, tardive dyskinesia, and parkinsonism. Aripiprazole is the agent of choice in patients with prolonged QTc on electrocardiogram. These medications may be administered on a scheduled as well as an as-needed basis but their use in the morning should be avoided if possible as they are frequently sedating. Benzodiazepines should be reserved for treatment of benzodiazepine withdrawal, alcohol withdrawal, catatonia, or for control of myoclonus or clonus in the setting of a toxidrome such as serotonin syndrome or neuroleptic malignant syndrome.
PROGNOSIS
The majority of acute confusional states are reversible with treatment of the underlying cause; however, many can result in permanent neurologic morbidity or mortality if diagnosis and treatment are delayed. For example, unrecognized PRES can lead to infarctions or hemorrhage. Untreated hyperammonemia can result in irreversible encephalopathy and delayed recognition of serotonin syndrome with sustained serotonergic overdrive can lead to fatal systemic complications from hyperthermia, rhabdomyolysis, and renal failure. Delirium related to prolonged hospitalization, recent operation, or sedation is also typically reversible; however, there is clearly an independent relationship between mortality and delirium in hospitalized patients. Furthermore, patients with delirium in the hospital may develop new long-term cognitive impairment.
COMMENTARY ON THE CASE
An underlying neurocognitive disorder with exposure to opiates in the setting of acute renal failure and a UTI likely resulted in this patient’s acute encephalopathy. During routine laboratory testing, which also consisted of blood cultures and urinalysis, given his fever, a UTI was identified. He could be said to have decompensated dementia, delirium, or acute encephalopathy secondary to UTI, opiate administration, and acute kidney injury. All would apply. Opiates were discontinued, his infection was treated, and he was continued on an atypical antipsychotic (quetiapine), given his possible Parkinsonism. His confusion slowly resolved.
• Any acute organ dysfunction can produce an acute confusional state and the severity varies depending on the degree of organ dysfunction and the rapidity over which it developed.
• Toxic causes of encephalopathy include intoxication or withdrawal syndromes, drug-drug interactions, or drug toxicity in the setting of reduced renal or hepatic function.
• Nonconvulsive seizures, status epilepticus, or postictal states can present as acute confusional states.
• Patients with underlying cognitive impairment can easily decompensate in the setting of an acute medical or neurologic insult, a condition known as “beclouded” or “decompensated” dementia.
• The differential diagnosis of acute confusional state includes locked-in syndrome, transient global amnesia, and psychiatric disease.
• Nonpharmacologic approaches to the management of acute confusional state include prevention of sensory deprivation, sleep enhancement, familiarization of the environment by frequent reorientation, use of photographs of loved ones, or the physical presence of family members.
• Haloperidol remains the drug of choice in an emergency where either the safety of the patient or care providers is at risk.
• The majority of acute confusional states are reversible with treatment of the underlying cause unless recognition is delayed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree