13.1).
(2) Motor evaluation. The motor functions of the trigeminal nerve are assessed by means of testing the muscles of mastication. By having a patient clench the jaw, the strength of the masseters and temporalis can be tested bilaterally. Weakness is evidenced by absent or reduced contraction of the muscles on the side of the lesion. The lateral pterygoids are tested by having the patient move the jaw from side to side against the resistance of the examiner’s hand. The jaw deviates toward the paralyzed side on opening the mouth because of contraction of the intact contralateral lateral pterygoid muscle. It cannot be deviated to the opposite, nonparalyzed side. Finally, the patient should be asked to protrude the jaw. Any evidence of atrophy or fasciculation is noted.
(3) Reflex evaluation.
(a) Corneal reflex. This reflex is assessed by means of touching a wisp of a sterile cotton-tipped applicator to the edge of the cornea (not the sclera) bilaterally. The afferent portion of the reflex is carried by V1 (upper cornea) and V2 (lower cornea), and the efferent portion is carried by cranial nerve VII, both ipsilaterally and contralaterally. Lesions of the trigeminal nerve may cause a diminished or absent response both ipsilaterally and contralaterally.
(b) Orbicularis oculi reflex (blink reflex). This reflex is assessed by means of tapping the glabella or supraorbital ridge. This elicits an early ipsilateral blink followed by bilateral blinking.
(c) Sternutatory reflex. This reflex is assessed by means of checking light touch sensation of the lateral nasal mucosa with a cotton-tipped applicator. The appropriate response is immediate withdrawal from the irritating stimulus. This reflex may be diminished or absent in lesions of the maxillary division (V2).
(d) Masseter reflex or jaw jerk. This reflex is assessed by means of tapping the slightly opened lower jaw. Lesions of the trigeminal nerve may result in a hypoactive ipsilateral jerk, whereas bilateral supranuclear lesions may result in a hyperactive response.
b. The rest of the neurologic examination.
(1) Speech. Dysarthria may be present with profound facial, tongue, or oral sensory deficits.
(2) Cranial nerves. Careful attention should be paid to associated abnormalities of cranial nerves, especially II, III, IV, VI, VII, and VIII.
(3) Motor and muscle stretch reflexes.
(4) Sensory loss. It is important to evaluate for evidence of other regions of sensory loss, especially generalized sensory neuropathy.
(5) Coordination. Coordination can be impaired by a process such as a tumor in the cerebellopontine angle.
(6) Gait and station.
Five domains are required for correct diagnosis. These domains are often formulated as “assessment” after the history and examination are completed.
• Time course.
• Is the facial numbness acute, subacute, or chronic?
• Is it progressive, transient, or stable? Note transient numbness is often due to migraine, epilepsy, or functional complaints.
• Was the onset abrupt, subacute, or chronic?
• Quality.
• Paresthesia—a spontaneous abnormal sensation.
• Dysesthesia—an unpleasant abnormal sensation produced by normal stimuli.
• Hypoesthesia—this is classic numbness when the threshold for sensory detection is increased.
• Pain—Trigeminal nerve dysfunction associated with pain is discussed in Chapter 14.
• Location.
• Bilateral vs. unilateral: Unilateral numbness is more common. Bilateral numbness can be associated with brainstem involvement, leptomeningeal disease, or systemic diseases, or it can be idiopathic.
• Partial or complete.
• Distribution: Trigeminal branches or branches of cervical plexus.
• Does it include the mucous membranes?
• Associated symptoms. Brainstem, higher cortical function, headache, and other sensory, for example.
• Red flags. These are associated with potentially serious disorders.
• Brainstem signs:
• Horner’s syndrome: This can be seen both in carotid dissection and brainstem pathology.
• Cerebellar signs: These signs, including slurring of speech, can be seen in pontine lesions.
• Multiple cranial nerve involvements: Most commonly VII, VIII.
• Hemiplegia: Points to motor tracts of the brainstem being involved.
• Myelopathic signs. High spine lesions can cause numbness in the C2 distribution.
• Confusion. May suggest a cortical process.
• Numbness not confined to the face. May suggest lesions of the neuraxis.
• Change in vision or diplopia. May suggest retro-orbital or cavernous etiology.
STEP 2: LOCALIZATION
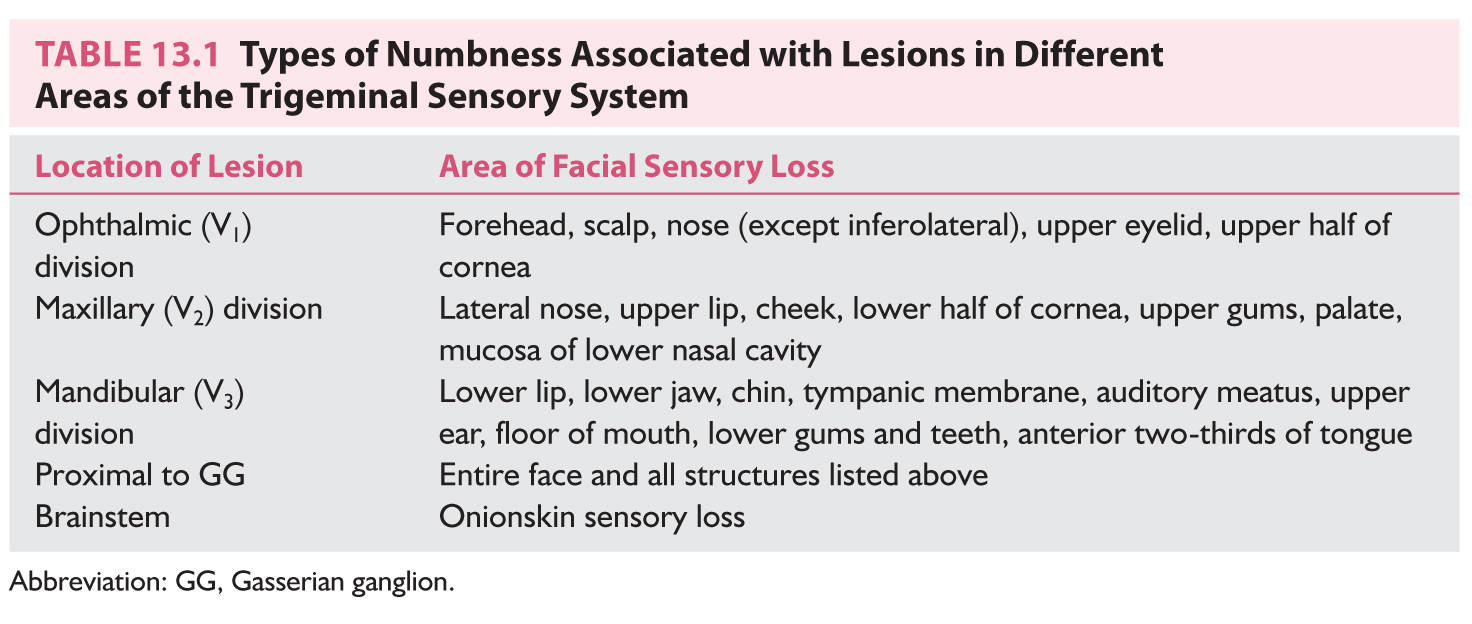
Facial numbness may be caused by a variety of causes including cortical, subcortical, brainstem, trigeminal nerve, cervical plexus (angle of the jaw numbness) (Table 13.1), and higher cord lesions. Several generalizations may be used to localize the lesion.
1. Lesions of the divisions of cranial nerve V have distinct areas of sensory loss (Fig. 13.1).
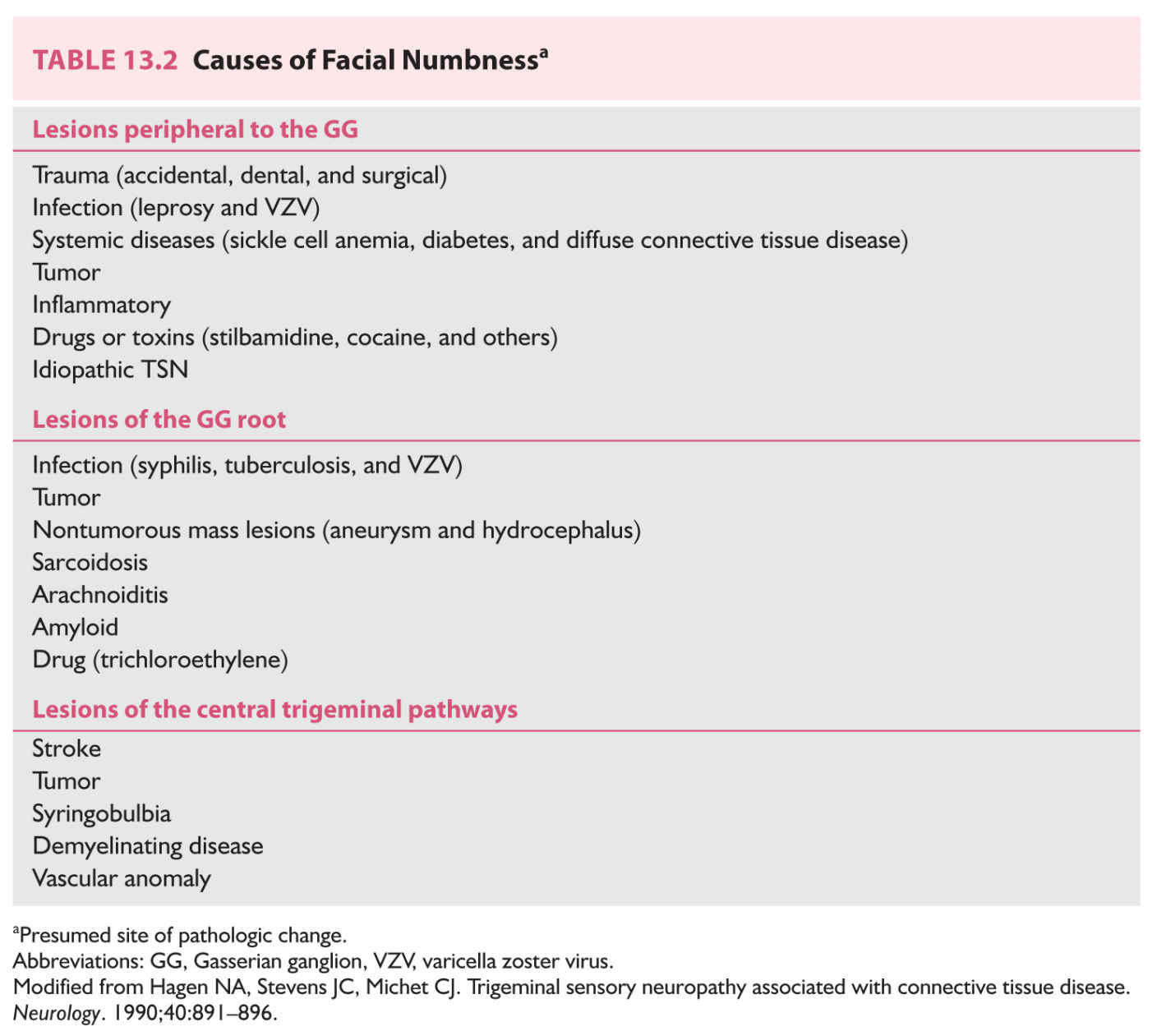
2. Lesions proximal to the Gasserian ganglion (GG) cause cutaneous numbness of the entire face and the anterior scalp (Fig. 13.2).
3. Lesions of the brainstem can produce an onionskin distribution of sensory loss (Fig. 13.3).
4. Lesions of cranial nerve V typically spare the angle of the jaw, which is supplied by C2 and C3 (Fig. 13.1).
5. Lesions of the trigeminothalamic pathway above the brainstem are often accompanied by involvement of the trunk because of the involvement of adjacent sensory pathways.
6. Cortical lesions leading to facial numbness may be accompanied by motor symptoms because of the involvement of the adjacent motor cortex.
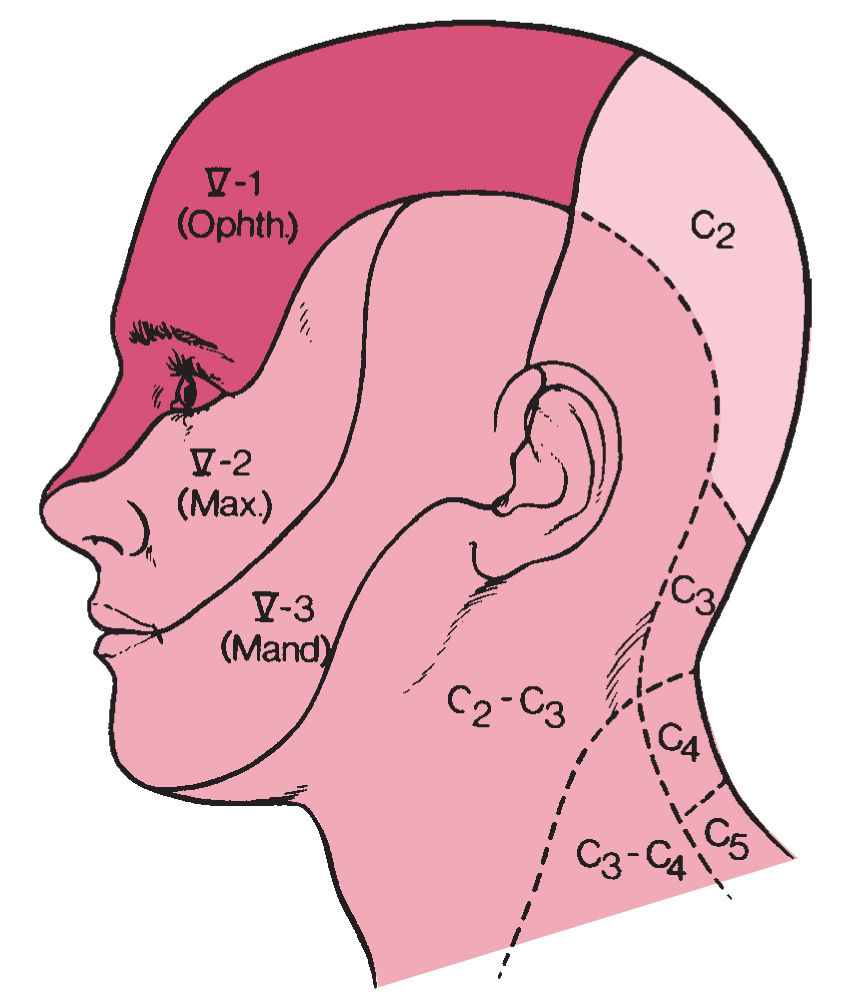
FIGURE 13.1 Regions of the face supplied by the three sensory divisions of the trigeminal nerve (V1, V2, and V3). (Modified from Sears ES, Franklin GM. Diseases of the cranial nerves. In: Rosenberg RN, ed. Neurology. New York, NY: Grune & Stratton; 1980, with permission.)
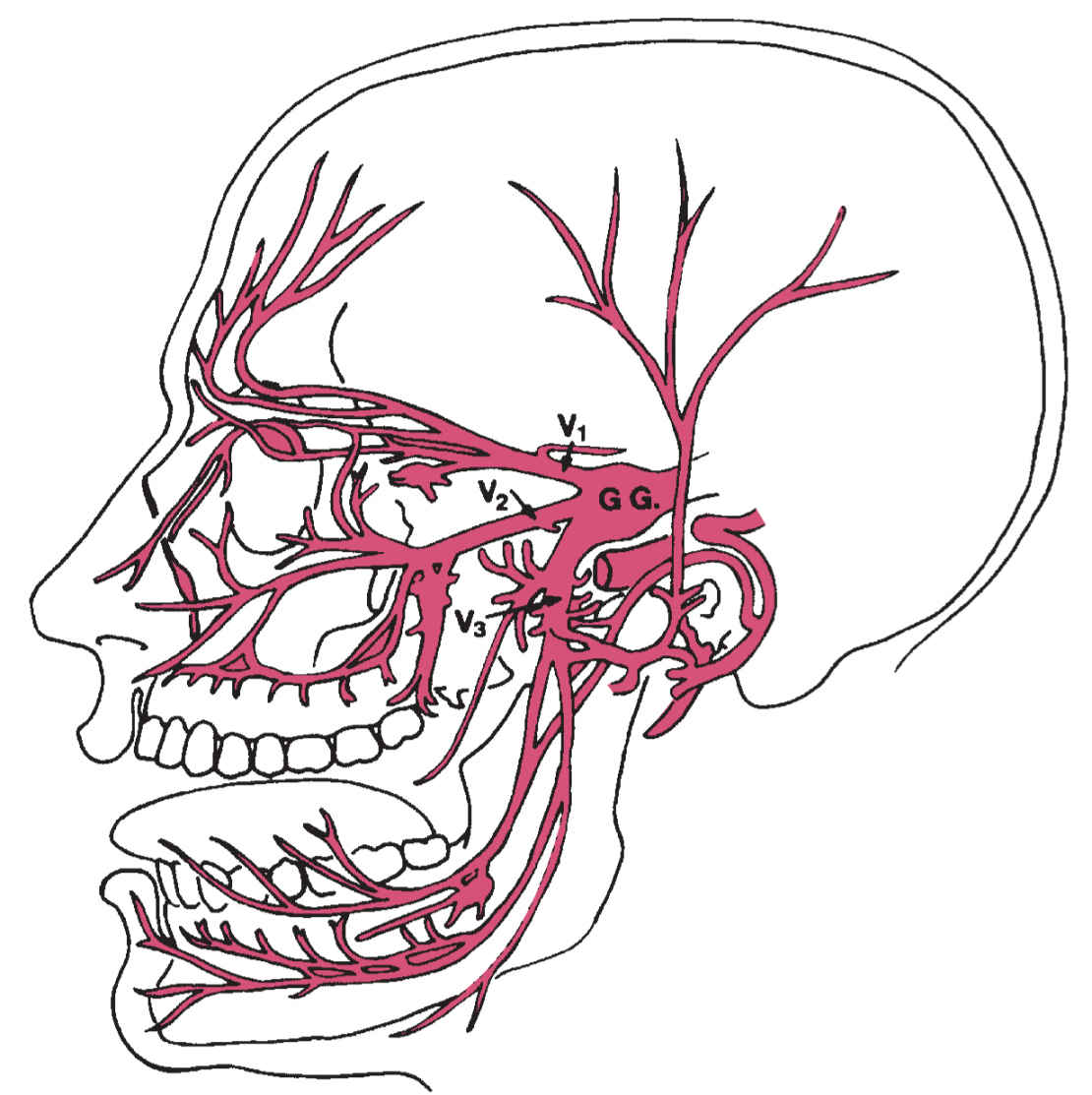
FIGURE 13.2 Relations between the divisions of the trigeminal nerve and the GG.
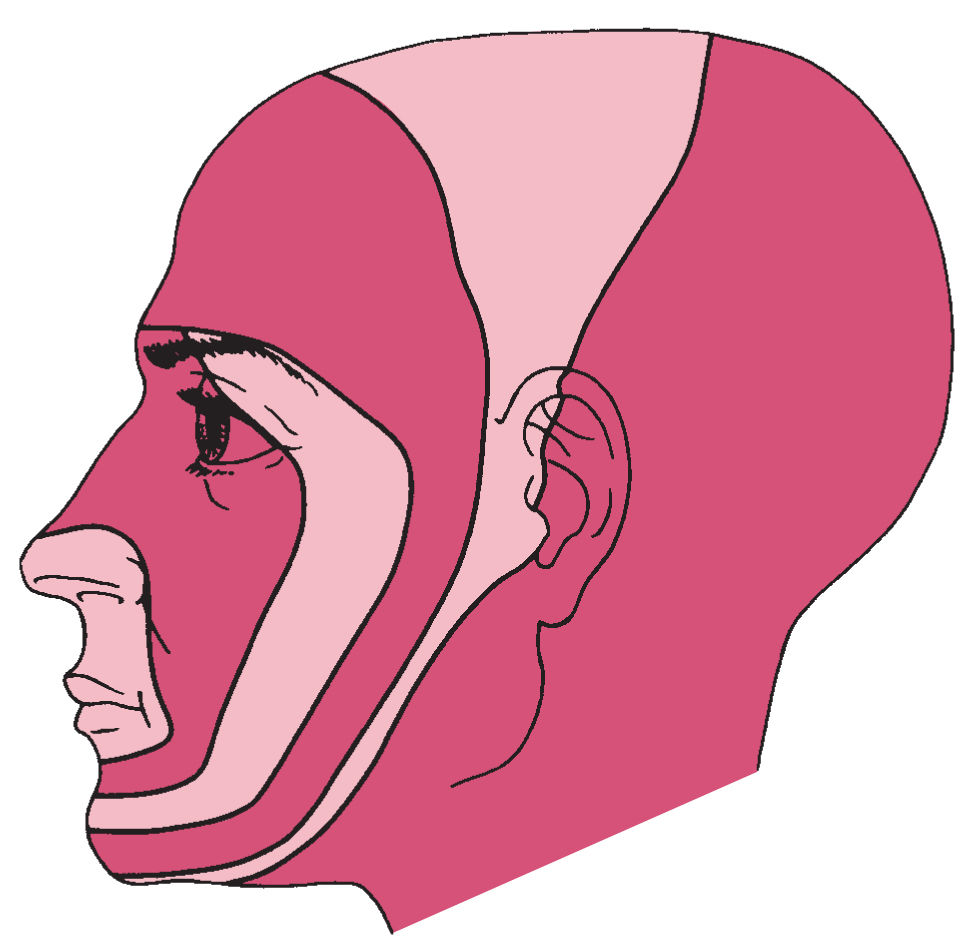
FIGURE 13.3 Onionskin sensory loss resulting from brainstem lesions.
These rules of thumb are based on the neuroanatomy of the trigeminal pain system:
A. Neuroanatomy of the trigeminal sensory system
1. The trigeminal nerve (cranial nerve V) is a mixed sensory and motor nerve.
a. The sensory portion of the nerve is the largest portion, transmitting sensation from areas of the face, oral cavity, and nasal passages.
b. There are three divisions of the sensory portion of the trigeminal nerve (Fig. 13.1).
(1) Ophthalmic (V1). The ophthalmic division provides cutaneous supply to the forehead and anterior scalp to approximately the vertex, parts of the nose and the upper eyelid, and the upper half of the cornea. Branches of this division to the facial structures are the nasociliary, infratrochlear, supratrochlear, lacrimal, and supraorbital nerves.
(2) Maxillary (V2). The maxillary division provides cutaneous supply to portions of the nose, upper lip, cheek, lower half of the cornea, upper gums and teeth, palate, and nasal mucosa. Branches of this division are the zygomaticofacial, zygomaticotemporal, and infraorbital nerves.
(3) Mandibular (V3). The mandibular division provides cutaneous supply to the lower lip; chin; portions of the jaw, ear, and mouth; lower gums and teeth; and the anterior two-thirds of the tongue. Branches of this division are the auriculotemporal, buccal, and mental nerves. The combined nerve trunk of the mandibular division and the motor portion gives rise to the inferior alveolar nerves and the lingual nerves.
(a) The motor portion of the trigeminal nerve is a smaller division that travels with V3. It provides motor function to the muscles of mastication and the tensor tympani. This portion is not discussed further. However, it is important to examine the patient for dysfunction of the motor portion of the nerve.
c. The three sensory divisions (V1, V2, and V3) enter the cranial cavity through the superior orbital fissure, foramen rotundum, and foramen ovale, respectively, to unite in the Gasserian or semilunar ganglion, which lies at the apex of the petrous bones. The first-order neurons for trigeminal nerves are in these ganglia. The exception to this are the proprioceptive fibers, the first-order neurons of which are in the mesencephalic nucleus of trigeminal.
d. Second-order neurons are in the spinal, principal, and mesencephalic nuclei of trigeminal. They synapse on the ventroposteromedial nucleus of thalamus, which projects to the primary and secondary somatosensory cortices.
STEP 3: LOCALIZATION: CAUSES OF FACIAL NUMBNESS
In general, the causes of facial numbness are wide ranging and may include the following (Table 13.2):
A. Tumor
B. Infection
C. Trauma
D. Connective tissue disease
E. Drug or toxin
F. Nontumor mass lesion
G. Vascular disorder
H. Demyelinating disorder
I. Other systemic or rare disease
J. Idiopathic disorder
Since there are so many causes of facial numbness, anatomical localization plays an important role in narrowing down the differentials. The different causes are discussed according to the known or presumed site of involvement of the trigeminal pathway.
1. Lesions peripheral to the GG (V1, V2, and V3). The mnemonic VITAMIN D may be used to remember the various causes.
a. Vascular disorders. In rare instances, carotid artery dissection can produce facial numbness.
(1) Leprosy. Worldwide, lepromatous leprosy is the most common cause of facial numbness. There can be facial hypalgesia and resultant accidental mutilation of the face.
(2) Herpes zoster. Although the varicella zoster virus (VZV) resides in the GG, evidence of active infection usually involves a division of the trigeminal nerve. The most commonly affected division is the ophthalmic division.
(3) Paranasal sinusitis can affect some branches of the trigeminal nerve.
c. Trauma. Injury to the peripheral branches of the trigeminal nerve can occur with head or facial trauma, dental trauma or surgery, or any surgical procedure on the face (e.g., otorhinolaryngologic or dermatologic surgery).
(1) Head or facial injury. The most frequently affected nerves are the superficial branches, including the supraorbital (branch of V1), supratrochlear (branch of V1), and infraorbital (branch of V2) nerves. The sensory loss is temporally related to the injury. Nerve regeneration can be accompanied by facial pain. The supraorbital branch can be damaged by blunt injury or as a result of a fracture of the upper margin of the orbit. The infraorbital nerve can be injured with closed head injuries or maxillary fractures. The entire ophthalmic division (V1) can be damaged in fractures through the foramen ovale. Transverse basilar skull fractures can injure the GG, resulting in anesthesia of the entire face and weakness of the masticatory muscles.
(2) Dental trauma. Facial numbness can occur after tooth extraction. The inferior alveolar or lingual nerve can be damaged, and the result is transient anesthesia. Direct nerve injury also can occur as a result of needle trauma during dental anesthesia. In patients with severe mandibular bone resorption, denture use can cause pressure on the mental nerve, resulting in chin numbness.
(3) Facial surgery. Any surgical procedure involving the face can lead to trigeminal nerve injury. Facial numbness has been described as a postoperative complication of microvascular decompression for trigeminal neuralgia due to trauma to the trigeminal root.
d. Autoimmune. The presence of facial numbness with a connective tissue disorder is rare. It has been associated with systemic sclerosis, Sjögren’s syndrome, mixed connective tissue disease, systemic lupus erythematosus, rheumatoid arthritis, and dermatomyositis.
e. Metabolic and systemic disease.
(1) Sickle cell anemia. Numbness of the chin and lower lip resulting from mental neuropathy with sickle cell crisis has been described.
(2) Diabetes. Facial numbness has been reported with diabetes and can accompany other forms of sensory neuropathy.
f. Idiopathic trigeminal sensory neuropathy (TSN). This diagnosis is one of exclusion after serious causes have been ruled out (see section Classic Clinical Syndromes).
g. Neoplastic. Regional spread of a tumor along the trigeminal nerve can occur. Disease (most commonly of the lung and breast) metastasizing to the lower jaw can affect the inferior alveolar or mental nerve and cause numbness of the chin and lower lip. Cheek or malar numbness has been described with local spread of tumors along V2 or with leptomeningeal involvement with tumors. Meckel cave tumors (Fig. 13.4) may affect one or more divisions of the trigeminal nerve. Numbness of the cheek or malar region (numb cheek syndrome) may herald the recurrence of squamous cell carcinoma of the skin. Nasopharyngeal tumors (squamous cell carcinoma is most common) arise most frequently in the roof of the pharynx. They can encroach on the trigeminal nerve, producing facial numbness. Associated features can include excessive lacrimation, facial pain, proptosis, hearing loss, and Horner’s syndrome.
h. Drugs and toxins.
(1) Stilbamidine is an agent that has been used to treat leishmaniasis and multiple myeloma. Unilateral or bilateral facial numbness and anesthesia have been reported after treatment.
(2) Cocaine abuse by the nasal route is a cause of facial numbness in the territory of the maxillary division (V2). Usually, there is associated traumatic and ischemic necrosis of the nasal mucosa.
(3) Other drugs. Many drugs can cause facial paresthesia. Circumoral paresthesia has been reported with labetalol, and mandibular neuropathy has been reported with allopurinol.
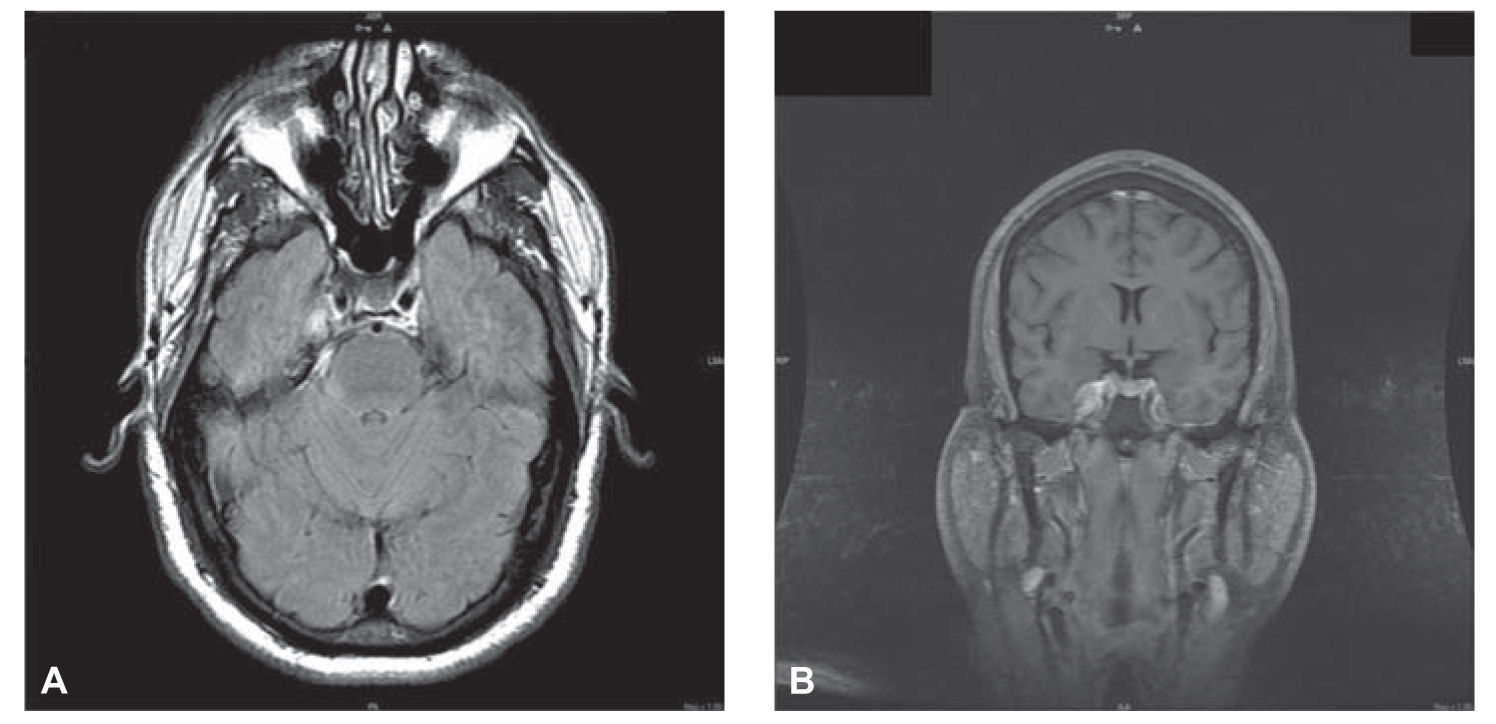
FIGURE 13.4 A and B: Brain MRI with contrast showing enhancing extra-axial mass involving the right Meckel’s cave and right cavernous sinus extending into the tentorium. (Courtesy of Drs. Ulises Nobo and José Biller.)
2. Lesions of the GG or root (mnemonic SAD TINA)
a. Sarcoidosis.
b. Amyloidosis. In rare instances, the GG or root can be the solitary site of amyloid deposits.
c. Drug. Trichloroethylene is an industrial solvent that has been associated with facial numbness.
d. Tumor. Various tumors can affect the GG or root. Tumors that arise in the ganglion (ganglioneuroma or gangliocytoma) tend to have early, associated pain. Tumors that arise primarily in the root (neurinoma or neurofibroma) tend to have predominant sensory loss without pain. Tumors that can compress or invade the ganglion or root include acoustic neuroma, meningioma, schwannoma, cholesteatoma, pituitary adenoma, chordoma, nasopharyngeal carcinoma, and metastatic lesions.
e. Infection of the GG can occur with syphilis, tuberculosis, and herpes zoster.
f. Nontumorous mass lesions (aneurysm and hydrocephalus).
g. Arachnoiditis.
3. Lesions of the central trigeminal pathways: Any process affecting the neuraxis can disrupt the trigeminothalamocortical pathway.
a. Stroke. Infarction in the lateral tegmentum of the medulla (Wallenberg’s syndrome) can produce ipsilateral facial numbness along with other cranial nerve deficits and long tract signs. In rare instances, lateral pontine hemorrhage causes isolated facial numbness, perhaps as a result of involvement of the main sensory nucleus of the trigeminal nerve.
b. Tumor. Tumors of the pons or medulla can affect the sensory nucleus of cranial nerve V, but there are usually other signs, including long tract and cranial nerve findings.
c. Syringobulbia. This central cavitation of the medulla or pons can be associated with facial numbness.
d. Demyelinating disease. Facial numbness is the initial symptom in 2% to 3% of patients with multiple sclerosis.
e. Vascular anomalies. Isolated facial numbness very rarely results from a posterior fossa aneurysm or other vascular malformation.
Testing is used to confirm or rule out differential diagnoses.
1. Biochemical tests include complete blood cell count with differential, complete chemistry profile including liver function tests and glucose level, and erythrocyte sedimentation rate. In certain situations, a Venereal Disease Research Laboratory (VDRL) test, antinuclear antibody determination, rheumatoid factor, extractable nuclear antigen antibodies, or an angiotensin-converting enzyme level may be necessary. Skin scraping or biopsy is necessary when leprosy is a consideration.
2. A purified protein derivative test should be done if there is suspicion of tuberculosis.
3. A chest radiograph should be obtained to evaluate for a malignancy, pulmonary disease, or tuberculosis.
4. Skull and sinus radiography. A radiograph of the mandible is indicated if there is a numb chin.
5. Lumbar puncture is essential if there is suspicion of infection or a malignant tumor of the leptomeninges.
6. A blink reflex may be elicited electrophysiologically by means of electrical stimulation of the supraorbital nerve. It can be helpful in detecting subtle central or peripheral lesions of the trigeminal nerve.
7. Brain imaging. Magnetic resonance imaging (MRI) without and with contrast is the imaging test of choice in most instances. The correct imaging protocol to evaluate the area of the suspected lesion should be discussed with the neuroradiologist prior to the test. Computed tomography (CT) with and without contrast enhancement may be indicated if MRI is not available or if there are contraindications to MRI.
STEP 5: TREATMENT AND REFERRAL
Because the range of possible underlying diseases that can cause facial numbness is so wide, it is often necessary to use a teamwork approach to the management of this problem. A neurologist, who should be most familiar with localization of lesions of the trigeminal nerve, should be consulted initially. It is often necessary to consult an otolaryngologist to evaluate for the presence of a nasopharyngeal tumor, acoustic neuroma, or sinusitis. A dentist or an oral surgeon may be needed to assist in ruling out a dental cause of facial numbness. In selected instances, a rheumatologist may be needed if there is evidence of associated connective tissue disease.
CLASSIC CLINICAL SYNDROMES
A. TSN. The literature is rather unclear in its definition of TSN. It has been used to describe different populations of patients with facial numbness. Blau et al. in 1969 described a population of patients with TSN who had self-limited facial paresthesia that in one-half of the cases resolved in several months. There were no associated neurologic deficits. At neurologic examination, the corneal response was intact, and the only finding was a subjective decrease in light touch and pinprick over the involved trigeminal distribution. Only 10% of these patients had identifiable causes of TSN, and 10% went on to have trigeminal neuralgia. In contrast to this population, with a seemingly benign course, Horowitz in 1974 found that 88% of a population with facial numbness had an identifiable, usually serious condition. This population almost always had other neurologic deficits (cranial nerve or ataxia). It may be concluded that these two studies involved quite different populations.
TSN is best defined as a general term for facial numbness of which there are many different causes, as previously discussed. Any area of the face can be involved. Idiopathic TSN is used to describe purely sensory impairment of unknown causation in a territory of the trigeminal nerve (usually V2 or V3) on one or both sides of the face. It can be associated with pain, paresthesia, or dysfunction of taste. Because the data currently available do not allow one to differentiate consistently between facial numbness that is benign and facial numbness that is attributable to a serious condition, idiopathic TSN remains a diagnosis of exclusion after an appropriate, thorough evaluation. Available data do indicate that the presence of associated neurologic signs and deficits usually points to a more ominous process.
B. Numb chin and numb cheek syndromes.
1. Numb chin syndrome is an uncommon form of facial neuropathy. However, the occurrence of this syndrome is notable because in the absence of a history of dental trauma, numb chin syndrome is rarely caused by benign lesions and is often a symptom of more ominous processes such as involvement of the mental or inferior alveolar nerves (branches of V3) by systemic cancer.
a. Any tumor metastasizing to the jaw can produce this syndrome, but malignant tumors of the breast, lung, and lymphoreticular system are found most commonly. Numb chin syndrome also can be caused by metastasis to the proximal mandibular root at the base of the skull or by leptomeningeal involvement with malignant tumors such as lymphoma.
b. Most patients already have a known diagnosis of cancer. However, mental neuropathy can be the initial symptom of malignant disease or it can herald tumor recurrence or progression.
c. The clinical presentation involves ipsilateral numbness or anesthesia of the skin and mucosa of the lower lip and chin that extends to the midline. There is usually no associated pain, but there can be lip swelling and ulceration from biting of the numb lip.
d. The evaluation of patients with numb chin syndrome should include radiographs of the mandible with particular attention to the mental foramen, radiographs of the basal skull, MRI of the brain with contrast enhancement, and if there is concern of leptomeningeal infiltration, cerebrospinal fluid analysis.
e. Although a numb chin is a seemingly benign problem, it should be thoroughly evaluated because of its clinical importance as a possible sign of malignant disease.
2. Numb cheek syndrome. Lesions of the maxillary division of the trigeminal nerve in the infraorbital foramen may cause the numb cheek syndrome. Unilateral numbness over the malar region and the upper lip in an infraorbital nerve distribution is typical of this syndrome. These findings can have implications similar to those of numb chin syndrome. Malignancies such as squamous or basal cell carcinoma of the facial skin can spread along the trigeminal nerve. Such tumors also can spread from regional nerves to the skull base and into the intracranial space. Numbness of the anterior gums and teeth suggests a more peripheral lesion, whereas both anterior and posterior gum and teeth involvement suggests leptomeningeal disease.
Key Points
• Diverse etiologies may be responsible for isolated facial numbness (more broad numbness that includes the face is treated elsewhere in the book). For this reason there is a need for a systematic approach to the diagnosis of causes.
• History and examination should concentrate on determining the time course of the symptoms, quality, associated symptoms, and red flags.
• Localization is the basis of narrowing down the large list of differentials.
• The treatment of facial numbness is achieved by addressing the underlying causes and will require expertise outside of neurology.
• Classic trigeminal syndromes include idiopathic trigeminal neuropathy, numb cheek, and numb chin syndromes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree