Artifacts and Mimickers
Juan C. Troncoso
Artifacts are common occurrences in the examination of autopsy brains as a result of postmortem putrefaction and autolysis and the removal, handling, and fixation of the fresh brain or spinal cord. The neuropathologist should also look for and document findings related to surgery.
ARTIFACTS
Lesions of the Dura Mater (Fig. 24.1)
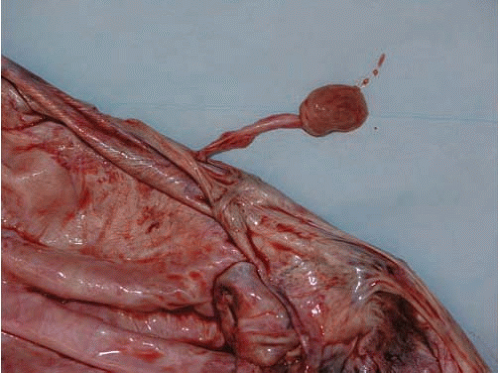
The dura mater may show premortem changes such as green discoloration in individuals with hyperbilirrubinemia and jaundice, or pink discoloration in CO toxicity. In fire victims, the dura can be charred. Tumors of the dura, in particular meningiomas, are not infrequent findings. The pathologist, however, should be aware that at times, the pineal gland may remain attached to the dura mater and mimic a meningioma
Putrefaction
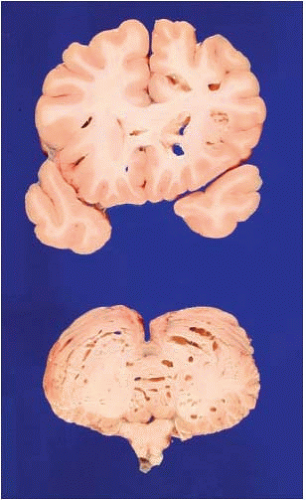
Putrefaction is the most common artifact and consists of a variable number of cysts or cavities throughout the parenchyma of the brain, predominantly in the deep cerebral white matter and basal ganglia, as shown in Figure 24.2. This artifact is also known as “swiss cheese artifact” and it is due to the postmortem proliferation of gas-producing bacteria. The gas displaces the tissue and produces cysts of various sizes, from a few millimeters to 1 or 2 cm, with very smooth and glistening surfaces.
A common mistake is to call a putrefaction cyst a lacunar infarct. This error is common when the cysts are small and located in the basal ganglia or white matter. On gross examination, the putrefaction cyst has a regular circular shape, very smooth walls, and its cavity is free of any tissue. In contrast, a lacunar infarct is irregular in shape, its surface tends to be rugged, and it usually has tissue strands that bridge the walls of the cavity. Microscopically, the putrefaction cyst contains bacteria, whereas the lacunar infarct shows macrophages in the cavity and is surrounded by an astrocytic scar.
When putrefaction cysts are abundant, it is possible to confuse them with cysticercosis. On gross examination, the difference is that the lesions of cysticercosis tend to be located in the gray matter and putrefaction cysts are more common in white matter. Microscopically, the cysticercosis cyst may contain parasites and frequently, there is a marked inflammatory response surrounding the lesion.
Poor Fixation and Pink Discoloration of the Brain
Specimens that are poorly fixed due to short time in fixative or insufficient volume of formalin frequently show a light pink discoloration of the parenchyma. This discoloration can be confused with the changes in carbon monoxide (CO) intoxication. The pink discoloration due to poor fixation is usually present in the depth of the cerebral hemispheres, but not in the cerebral cortex, a pattern explained by the diffusion of the formalin from the convexity inwards. Occasionally, the pink discoloration appears as a subtle band that corresponds to the front of the formalin diffusion. In contrast, the discoloration of CO toxicity affects predominantly gray matter, both cortical and basal ganglia. Moreover, the discoloration of CO fades on contact with air.
Pseudo Pseudolaminar Necrosis of the Cerebral Cortex
Pseudo pseudolaminar necrosis is an uncommon fixation artifact that may involve large extensions of the cerebral cortex. The only way to differentiate this artifact from true pseudolaminar necrosis is to examine a histologic section, which shows the superficial
cortical layers peeling off without necrosis of neurons or the presence of macrophages or gliosis (Fig. 24.3).
cortical layers peeling off without necrosis of neurons or the presence of macrophages or gliosis (Fig. 24.3).
Flattened Convexity of a Cerebral Hemisphere
Flattened convexity is not an uncommon occurrence and is caused by laying the fresh brain on its side on the counter before placing it in fixative; it is also known as “counter artifact” (Fig. 24.4). The flattening of the convexity can be mistaken for the effect of a subdural hematoma. Consider that, at times, the volume of a fresh subdural hemorrhage is difficult to assess. The subdural hematoma is usually accompanied by subfalcial herniation and distortion of the ventricular system, whereas the counter artifact is not.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree