Figure 66-1 Autonomic testing. A, The patient performs a Valsalva maneuver (blowing into a sealed tube for 15 seconds against an expiratory pressure of 35 mm Hg). There is no change in the heart rate response (seen by the gray line) and a dramatic and sustained fall in blood pressure. B, The patient undergoes tilt-table testing. The blood pressure drops to unmeasurable levels immediately after head-up tilt to 60 degrees. There is no compensatory heart rate increase (gray line).
(From Gibbons CH, Vernino SA, Kaufmann H, Freeman R. L-DOPS therapy for refractory orthostatic hypotension in autoimmune autonomic neuropathy. Neurology 2005;65:1106, with permission.)
She was treated with fludrocortisone (0.4 mg), vasopressin (0.4 mg qhs), erythropoietin (3000 units triweekly), and midodrine (40 mg qid). She required straight catheterization for her urinary retention and multiple agents (docusate sodium, lactulose and enemas) for management of her severe constipation. She received plasma exchange (five treatments over 10 days) and intravenous immunoglobulin (2 g/kg divided over 5 days).1
After 2 weeks of maximal symptomatic therapy and immunomodulatory therapy, she was still unable to stand for more than 1 minute. After institutional board review and informed consent, the patient received the experimental norepinephrine precursor, L-threo-3,4-dihydroxyphenylserine (L-DOPS) to augment blood pressure. The effect of L-DOPS on blood pressure and standing time is shown in Figure 66-2. She was maintained on L-DOPS 300 mg and was able to walk for 60 minutes without syncope and was discharged home.1 She was unable to stand for any length of time if she omitted a dose of the medication.
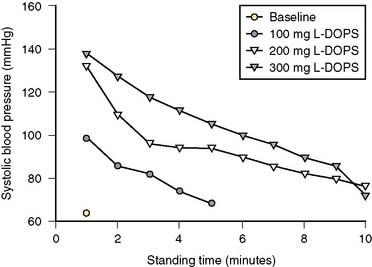
Figure 66-2 Standing time. The length of time that the patient could stand, with the corresponding blood pressure, at baseline and during increasing doses of L-DOPS. Without L-DOPS the patient could barely stand for 1 minute, at 200-mg and 300-mg doses of L-DOPS the patient was able to stand for 10 minutes.
(From Gibbons CH, Vernino SA, Kaufmann H, Freeman R. L-DOPS therapy for refractory orthostatic hypotension in autoimmune autonomic neuropathy. Neurology 2005;65:1105, with permission.)
CONCLUSION
The patient had an acute autonomic neuropathy with antibodies to the ganglionic acetylcholine receptor. The antibodies are present in up to 50% of patients in some idiopathic autonomic neuropathy series. The preferred term for idiopathic autonomic neuropathy (also called idiopathic autoimmune autonomic neuropathy, subacute autonomic neuropathy, and pure pandysautonomia),3 when these antibodies are present, is AAG because the primary pathology is in the autonomic ganglia rather than nerve fibers.8
This acquired immune-mediated disorder, which is associated with and most likely caused by antibodies to the ganglionic nicotinic acetylcholine receptor, leads to autonomic failure.2 Preclinical studies suggest that these antibodies impair ganglionic synaptic transmission by depleting acetylcholine receptors on the ganglionic neuron.4 Some patients present with a rapid clinical decline, whereas others have a more indolent course that can mimic a neurodegenerative process.5,6 An antecedent viral infection is frequently reported, although no specific infectious agent has been identified. Recent immunization and surgical procedures are also associated with the condition.
Patients present with sympathetic adrenergic symptoms (orthostatic lightheadedness, pre-syncope and syncope), sympathetic cholinergic symptoms (anhidrosis or hypohidrosis), and cholinergic symptoms (secretomotor dysfunction, bowel and bladder hypomotility). There is clinical heterogeneity among patients with AAG. Those patients with the highest antibody titers tend to have more widespread dysautonomia, whereas those with lower antibody levels may have more focal or restricted presentations involving the cardiovascular, bladder, bowel, sudomotor, or secretomotor systems.2,5.7
Orthostatic hypotension is the most incapacitating symptom of AAG. Patients present with orthostatic intolerance, presyncope, and syncope. Orthostatic blood pressure falls in some patients are greater than 100 mm Hg and are accompanied by profound falls in blood pressure during phase II of the Valsalva maneuver. There is a sigmoidal relation between the fall in blood pressure and antibody titers with a threshold antibody level for the appearance of symptoms. Clinically significant orthostatic hypotension is not present in patients with antibody levels less than 1 nmol/L as seen in Figure 66-3. But when antibodies levels are greater than 1 nmol/L (the linear portion of the sigmoidal function) there is a strong positive correlation between the antibody level and the fall in systolic blood pressure.7
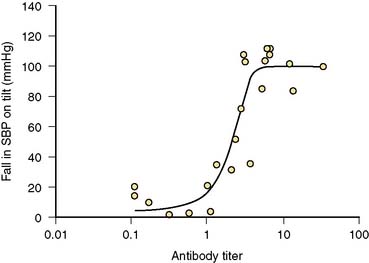
Figure 66-3 Fall in systolic blood pressure and corresponding antibody titer. Increasing antibody titers, shown on a log scale, result in larger falls in systolic blood pressure between the supine and standing position. The sigmoidal relationship (r2 = 0.84) has a threshold antibody titer of approximately 1 nmol/L, below which antibodies have little effect on systolic blood pressure. Antibody titers of 1 to 3 nmol/L result in increasing falls in blood pressure with the saturation point of the curve occuring at approximately 3 nmol/L, where systolic blood pressures drop approximately 100 mm Hg.
(From Gibbons CH, Freeman R. Antibody titers predict clinical features of autoimmune autonomic ganglionopathy. Auton Neurosci 2009:146:8-12, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








