CHAPTER 22 Avoidance of Complications in Neurosurgery
Avoidance of complications in neurosurgery begins with the correct selection of patients who are likely to benefit from the surgical intervention planned. When possible, patients with nonmedical issues that have a known association with poor outcomes, such as workers’ compensation claims or pending lawsuits, should be investigated further to determine the patient’s motivation for recovery.1–7 Taking the time to explain the probable risks and benefits of the procedure allows the patient to make an informed decision and protects the surgeon in the event of an adverse outcome from claims of inadequate consent. The remainder of this chapter focuses on prevention of complications once the patient has arrived in the operating room. Intraoperative complications may be related to anesthetic issues, positioning of the patient, or technical or anatomic aspects of the specific surgery selected.
Before induction of anesthesia, the surgeon and anesthesiologist must discuss the case in detail and review what is likely to happen and the possible risks. Ideally, an experienced neuroanesthesiologist should be available for neurosurgical procedures. Adequate venous access, placement of a single- or double-lumen tube as required by the surgical approach, and insertion of an intracardiac central venous pressure line to potentially remove air emboli must be planned in advance. The presence of blood products in proximity to the operating room and notification of the blood bank that more may be required depend on the scope of the surgical procedure. Antibiotics should be administered within 1 hour before incisions to ensure therapeutic blood levels.8
Complications Related to Patient Positioning
After the anesthesiologist has determined that the airway has been adequately secured and that all lines and monitoring equipment are in place, the patient is ready to be positioned. Several common positioning errors can lead to complications,9–21 but most can be prevented with meticulous positioning protocols.
Prone Positioning
Nerve palsies and compression injuries are the most frequent complications seen and the most easily preventable. Radial and ulnar neuropathies can occur as a result of positioning the patient in the prone position with the arms extended if padding is inadequate or an inappropriate position is used. Keeping the arms in a mildly flexed position prevents excessive traction in either direction. Padding may be in the form of sheets or blankets placed under the elbows and forearms, or egg-crate foam padding can be used. Brachial plexus injuries can occur with rostral or caudal traction on the shoulders22 and is frequently seen in the prone position when the arms are extended in the cruciate position or too far above the head. Downward traction, such as when the shoulders need to be pulled down for x-ray localization in the low cervical or cervicothoracic junction, can also cause brachial plexus injury. If possible, any tension placed on the patient’s shoulders during radiography should be removed after the x-ray film has been obtained. Neurophysiologic monitoring of the ulnar nerve with somatosensory evoked potentials during spinal procedures has been shown to be effective in correcting and preventing position-related stretch injuries to the brachial plexus.23,24 Another common peripheral neuropathy associated with the prone position is inadequate padding of the anterior superior iliac crest, which can lead to pain or numbness in the distribution of the lateral femoral cutaneous nerve.25 A rare complication is obstruction of the external iliac artery or femoral artery from prolonged compression in the inguinal region.26,27
Another difficulty with positioning for spine surgery is the difference between the ideal position for a decompressive procedure, with the spine and hips flexed, and that for spinal fusion, with the spine in a more lordotic position and the hips and spine in neutral positions. Many patients have been subjected to iatrogenic flat-back syndrome because of improper position during a fusion procedure.28
Surgeons must be aware of the potential for unilateral or bilateral blindness after prolonged prone surgery. Causes have been hypothesized to be occlusion of the retinal artery or vein, direct trauma, orbital compartment syndrome, and ischemic optic neuropathy. Although rare, devastating complications have been described even when no direct trauma occurred, and therefore patients’ eyes should be checked frequently during the procedure. Minimizing blood loss and hypotensive episodes and maintaining a slightly elevated head of the bed may reduce the chance for this complication. If orbital compartment syndrome is suspected, emergency orbital decompression is the best chance for recovery.29–33
Lateral Positioning
The lateral or three-quarters lateral decubitus position carries with it specific risks for peripheral nerve injuries. Stretch on the brachial plexus can be prevented by placement of an axillary roll slightly thicker than the diameter of the upper part of the arm. This roll should be placed approximately four fingerbreadths below the armpit to prevent compression of the long thoracic nerve. Failure to place an adequately sized roll may lead to excessive stretch of the brachial plexus, with the greatest effects on the C5 and C6 nerve roots. The upper extremities need to be supported in relatively neutral positions to prevent ulnar neuropathies. Horner’s syndrome can occur when the head is inadequately padded and allowed to hang laterally in such a manner that excessive tension is placed on the superior cervical ganglion.34 Excessive traction on the lateral femoral cutaneous nerve can be caused by undue extension of the upper part of the leg at the hip while bending the dependent leg. Compression of the common peroneal nerve can occur as a result of inadequate padding laterally under the knee.
Intraoperative Monitoring
Various electrophysiologic modalities can be used to detect subtle signs of neurological compromise before they become fixed deficits. The use of intraoperative monitoring can reduce the likelihood of significant neurological deficits in the appropriate circumstances. Some positioning complications can be avoided with the concomitant use of intraoperative monitoring.9,35–39 At our institution, we use motor evoked potentials or somatosensory evoked potentials before and after positioning that may result in injury to the cervical cord. We have found excellent correlation between the lack of changes in evoked potentials and patient outcome. Monitoring is not necessary or indicated in all cases because it is time-consuming, can cause inappropriate movement of the patient, results in bleeding, and has the potential for needlestick injury to the operating room staff. However, in procedures with a potential for significant risk to the cord or neural structures, neurological monitoring is a helpful adjunct to the surgeon. Electrophysiologic neurological monitoring can consist of somatosensory evoked potentials, motor evoked potentials, intraoperative electromyographic responses, nerve action potential monitoring, direct spinal cord stimulation, and other methods.36,37,40–44 The information gleaned from these modalities can be used to determine whether manipulation of the neural elements is compromising conduction. Numerous authors have published series in which the surgeon has changed some portion of the procedure as a reaction to changes in electrophysiologic monitoring.9,35–39,43–48 Changes in ulnar nerve somatosensory evoked potentials can also indicate traction injury to the brachial plexus and is increasingly being used to monitor positioning, even with lumbar and thoracic procedures.23,24
Although not appropriate to monitor for position-related changes, direct epidural electrode motor evoked potential monitoring provides real-time evaluation of the spinal motor tracts and allows quantification of the measured output. This technique may be used during intramedullary spinal cord tumor resection and has been suggested to be helpful in minimizing injury during intramedullary resection.49
Cranial Fixation Complications
Pin site complications include lacerations,50 skull fractures, associated intracranial hemorrhage (i.e., epidural, subdural, or subarachnoid hemorrhages), and infections that can lead to osteomyelitis.51–56 Lacerations can be prevented by making sure that the two-pin arm swivels freely so that the force is evenly distributed between the two pins without one pin being shielded from tension, which can potentially result in pivoting on the other pin. If the pins are placed into muscle, it is wise to recheck tension on the single pin to make sure that the muscle has not settled and reduced the pressure. The three pins should be placed slightly below the center of gravity of the head when it is in final position to prevent gravity or personnel from pulling the head down and out of the pins. Ideally, the pins should not be placed directly into the coronal suture or temporal squamosal bone because these bones are most prone to fracture.57–59 Pins should be tightened to 60 to 80 lb in adults and 40 to 60 lb in children younger than 15 years. Pins are generally avoided in children younger than 2 years; however, some skull clamp systems do exist for these patients for procedures in which they are required.60
Other forms of head support include the horseshoe headrest and the four-cup headrest. Because the horseshoe headrest is not a rigid form of fixation, the head may shift during the procedure, and thus it is imperative that the anesthesiologist continuously observe for any signs of movement. The four-cup headrest is an excellent alternative to the horseshoe, although blindness, skin and scalp compression, and abnormal cervical motion are possible with either support. Alopecia has been reported as a result of scalp compression.61–67
Catastrophic Medical Complications
Venous Air Embolism
In positioning patients for neurosurgical procedures, the anesthesia team and the surgeons must be aware of the gradient between the patient’s head and the right atrium. Venous air embolism (VAE) is most often encountered with the patient in the seated position for posterior fossa surgery or cervical spine surgery.68–73 It has also been described in patients who have undergone procedures in the prone, supine, and lateral positions.68,71–77 Dehydration or blood loss leading to decreased central venous pressure may potentiate the risk for VAE. Patients with a patent foramen ovale or a known right-to-left shunt should be given special consideration before the seated position is used because the risk for paradoxical air embolism after VAE appears to be higher.
Given the dangers of VAE, early detection of the embolus is paramount in reducing the severity of this complication. Monitors used to detect emboli include precordial Doppler ultrasonography, capnography or mass spectrometry, transesophageal echocardiography, transcutaneous oxygen, esophageal stethoscope, and right heart catheter.68,69,71–74,77 The most sensitive are transesophageal echocardiography and Doppler, followed by expired nitrogen and end-tidal carbon dioxide. Electrocardiographic changes, hypotension, and heart murmurs are late signs. Because no single monitor is completely reliable, two or more should be used simultaneously. In awake patients, the presence of a cough may be the earliest sign of VAE, and it can be treated before the VAE becomes hemodynamically significant.78 Detection of VAE has increased over the past several decades, but serious morbidity and mortality have decreased. Its incidence varies from 1.2% to 60%, with morbidity and mortality rates of less than 3% in most series.
Deep Venous Thrombosis and Pulmonary Embolism
Deep venous thrombosis (DVT) and pulmonary embolism are major contributors to morbidity and mortality in postoperative neurosurgical patients. The incidence of DVT, as measured by the labeled fibrinogen technique, ranges from 29% to 43%.79–91 Most DVTs are asymptomatic and never come to medical attention. Pulmonary embolism, however, is thought to subsequently occur in 15% of such patients.80,84,89,92,93 Significant thrombi are thought to arise from the popliteal and iliofemoral veins. Risk factors include prolonged surgery and immobilization, previous DVT, malignancy, direct lower extremity trauma, limb weakness, use of oral contraceptives, gram-negative sepsis, advanced age, hypercoagulability, pregnancy, and congestive heart failure.79,81,83–89,92–100
Because of the often-fatal result of pulmonary embolism, prophylaxis against DVT is of major importance in neurosurgery. Many studies have confirmed the utility of sequential pneumatic leg compression devices in preventing DVT.80,81,83,84,89,90,101,102 These devices are placed on the patient preoperatively and should be continued until the patient is ambulatory. Early mobilization of postoperative patients is important in preventing thrombus formation. The prophylactic use of low-dose (minidose) subcutaneous heparin (e.g., 5000 IU twice daily) has been well studied over the past 25 years and has been demonstrated to be efficacious in preventing DVT.86,102–107 However, some studies have shown an increase in the rate of postoperative intracranial bleeding with minidose administration of heparin.102,103 Low-molecular-weight heparin (LMWH) has more recently been used for DVT prophylaxis in surgical patients. Several meta-analyses have been conducted, but it remains unclear whether unfractioned heparin or LMWH is superior for DVT prophylaxis in neurosurgical patients or whether increased efficacy correlates with increased hemorrhagic complications.108–111
Despite the use of such prophylactic methods, thrombi inevitably develop in one or both lower extremities in some patients. Management options include full-dose heparinization or inferior vena cava interruption. In the immediate and early postoperative period, many neurosurgeons believe that neurosurgical patients with documented DVT should undergo transvenous Greenfield filter placement.80,81,83,84,88,89,98,102 There appears to be a general consensus that full anticoagulation is acceptable 1 to 3 weeks after surgery; our institution uses the 1-week rule. Treatment with intravenous heparin (target partial thromboplastin time of 45 to 60 seconds) is followed by oral warfarin sulfate (target international normalized ratio of 2) when not contraindicated. Anticoagulation should be continued for 6 weeks to 3 months in uncomplicated cases. Gastrointestinal bleeding is the most common serious complication encountered.
Patients experiencing pulmonary embolism complain of pleuritic chest pain, hemoptysis, and dyspnea. Jugular venous distention, fever, rales, tachypnea, hypotension, and altered mental status may be found on physical examination. Arterial blood gas determination reveals a PO2 of less than 80 mm Hg in 85% of patients, accompanied by a widened alveolar-arterial gradient. The level of fibrin degradation products is elevated in most cases. In patients with massive embolism, right axis deviation, right ventricular strain, or right bundle branch block may be identified on electrocardiography. Chest radiography demonstrates an effusion or infiltrate in 90% of cases. A nuclear medicine ventilation-perfusion scan is sensitive in detecting pulmonary embolism but is not specific. The entire clinical scenario, including patient examination, laboratory results, and radiographic evaluation, leads to the diagnosis.80,84,89,93,112–116 Spiral computed tomography (CT) has become the preferred diagnostic study for pulmonary embolism.117 However, pulmonary angiography is the “gold standard” and may be necessary to confirm the diagnosis in as many as half of patients.
Wound Complications
Several potential problems related to the wound area and wound closure can be anticipated and prevented. The first category is postoperative blood collections, or hematomas. Ideally, postoperative hematomas can be prevented by meticulous hemostasis during the procedure, but such is not always the case. The use of postoperative drainage devices (e.g., Hemovac, Jackson-Pratt drain) in wounds for which hemostasis was difficult to achieve before closure can reduce the incidence of postoperative hematoma. Postoperative drainage may also be advantageous in patients in whom postoperative anticoagulation may be required because some of these patients have slightly delayed hematoma formation.118 An obese patient undergoing spine surgery may have significant serous exudation that can continue for up to 5 days or longer postoperatively. It is best to keep a drain in the submuscular space during this time to prevent a postoperative seroma that can become infected.
Risk Factors Related to Anatomy or Technique in Specific Surgeries
Cranial Surgery
Postoperative Seizures
The risk for postoperative seizures within the first week after supratentorial procedures has been well described in the literature.119–132 The underlying cause of these seizures may be metabolic derangements, cerebral hypoxia, preoperative structural defects, stroke and vascular abnormalities, or congenital seizure disorder. Manipulation of brain tissue, postoperative edema, and hematoma formation are common causes of surgically induced seizures. The overall incidence of immediate and early seizures after craniotomy is 4% to 19%.
It is important to identify any risk factors that may contribute to the development of seizures postoperatively. Lesions of the supratentorial intracranial compartment are responsible for seizures after craniotomy in most situations; seizures after infratentorial procedures are attributed to the resultant retraction or movement of supratentorial structures.119,120,124–129,131,133–136 Brain abscesses, hematomas, intra-axial and extra-axial tumors, aneurysms, arteriovenous malformations, and shunts have been reported to be epileptogenic.128,136–149 Patients with a preoperative history of epilepsy are at a higher risk for seizures postoperatively. Patients with subtherapeutic levels of prophylactic agents are also at a higher risk for immediate and early postoperative seizures.126,129,134,150–153
Preventing a seizure is preferable to treating one that has already begun. Adequate preoperative loading of parenteral or oral phenytoin has definitively been shown to decrease the incidence of postoperative seizures.154–156 In patients unable to tolerate phenytoin, phenobarbital or carbamazepine may be substituted. It follows that therapeutic preoperative levels should be measured in patients undergoing supratentorial procedures whenever possible. Administration of the anticonvulsant should continue through the acute and early postoperative period. Electrolyte abnormalities should be corrected immediately in the postoperative period to further reduce the chance for a seizure.
Reports have called into question the routine practice of phenytoin prophylaxis for patients without a history of seizures.126,152,157 How this will affect practices remains to be seen because a full medicoeconomic and medicolegal analysis is not yet available.
Postoperative Edema and Increased Intracranial Pressure
The neurological deficits caused by brain swelling may be permanent or transient, and the severity of the deficit depends on the patient. Edema usually begins within 5 hours after the procedure and reaches its maximum approximately 48 to 72 hours later.158–166 Altered mental status, cranial nerve deficits, and motor or sensory dysfunction can all occur. The diagnosis may be confirmed with non–contrast-enhanced CT, and hemorrhage, hydrocephalus, and pneumocephalus may be ruled out. Cerebral hypodensity, sulcal effacement, midline shift, loss of the gray-white matter interface, and small lateral ventricles are the hallmarks of postoperative edema. If impaired venous drainage secondary to the incompetence of venous sinuses is suspected, conventional venous-phase angiography or magnetic resonance venography may be helpful in diagnosing the location and severity of the occlusion. Appropriate surgical and medical measures may then be instituted.
The goal of treatment of increased ICP is to maintain cerebral perfusion pressure (CPP) at greater than 55 to 60 mm Hg while reducing the amount of cerebral edema.166–173 This entails measuring arterial blood pressure and ICP continuously. Induction of arterial hypertension with vasopressors may be necessary to achieve the desired CPP. Short-term hyperventilation to a PCO2 of 30 mm Hg can reduce ICP effectively. High-dose dexamethasone should be given to patients with vasogenic edema to alleviate tumor-related swelling. Increasing the head of the bed to 30 to 45 degrees can assist in venous return, and maintaining a neutral midline head position and administering diuretics such as furosemide and mannitol can further reduce ICP. When using diuretics, it is important that serum chemistries and osmolalities be monitored to ensure that the patient does not become severely dehydrated. Hypertonic saline solutions are now increasingly being used with success for the treatment of vasogenic edema.174,175 In refractory cases, sedation may be used to suppress cerebral metabolism and paralysis induced to reduce ICP by limiting agitation and muscle exertion. As a final resort, barbiturate coma with mild hypothermia or temporal lobectomy may be used to control ICP and maintain CPP.
Specific Cranial Disorders
Supratentorial Craniotomy
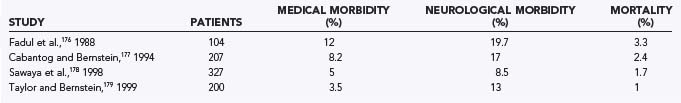
Numerous lesions may be approached via supratentorial craniotomy. In low-grade gliomas, long-term control and cure are possible. Because high-grade gliomas are not curable by surgery, surgery represents a palliative treatment aimed at reducing tumor bulk and maximizing quality of life. Patients with metastatic brain lesions can have a significant improvement in their survival by removal of brain metastases. It is therefore incumbent on neurosurgeons to minimize complications when patients are in the early stages of their disease and their clinical condition is best. The decision about whether surgery is warranted involves carefully weighing the possible surgical complications against the potential benefits. Studies have shown that craniotomies for intraparenchymal lesions typically result in mortality rates of 2.2% and morbidity rates of 15% (Table 22-1).176–179
Tumors located in eloquent or deep brain areas are more difficult to surgically debulk and carry a higher risk for neurological morbidity. Surgery on gliomas typically results in more morbidity and mortality than does surgery on brain metastases.178 Surgical outcome is closely tied to the patient’s age and preoperative neurological status as measured by the Karnofsky Performance Status score.176–178 Patients are at risk for general complications of craniotomies, including complications related to positioning, anesthesia, infection, seizures, hemorrhage, and neurological compromise. Neurological compromise may result from resection or retraction of normal functional brain tissue or compromise of the vascular supply. Neurological morbidities usually consist of motor or sensory deficits or aphasias (Table 22-2). Occasionally, visual field deficits can occur.
TABLE 22-2 Neurological Complications in Intraparenchymal Tumor Surgery
| COMPLICATION | RATE (%) |
|---|---|
| Motor or sensory deficit | 7.5 |
| Aphasia | 0.5 |
| Visual field deficit | 0.5 |
From Sawaya R, Hammoud M, Schoppa D. Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors. Neurosurgery. 1998;42:1044-1055.
Computer-assisted stereotactic systems enhance the ability of the surgeon to delineate between normal brain and tumor. Stereotactic systems also facilitate targeting of tumors that cannot be visualized at the brain’s surface. Intraoperative functional mapping helps identify and avoid injury to eloquent cortex. Craniotomy performed while the patient is awake is particularly helpful in resecting lesions surrounding the speech centers. Using an awake craniotomy technique, Taylor and Bernstein reported an overall complication rate of 16.5% and a mortality rate of 1%.179 New postoperative neurological deficits were seen in 13% of patients, but they were permanent in just 4.5%. Increasingly, functional imaging is being applied intraoperatively, with evidence suggesting that it allows more complete resection while minimizing the risk for deficits. Functional MRI and diffusion-weighted imaging can be integrated with most neuronavigation systems to allow identification and protection of motor tracts.180–183
Hemorrhage into the postoperative tumor bed represents a serious complication that may require reoperation for evacuation of hematoma. Prevention begins with checking preoperative coagulation studies and ensuring that the patient has not been taking an aspirin-containing product. Intraoperatively, meticulous hemostasis must be achieved with a variety of hemostatic agents and bipolar electrocautery. The tumor cavity may be lined with hemostatic agents such as Surgicel. Tight blood pressure control during extubation and in the postoperative period is important. Rarely, distal intracerebral or intracerebellar hemorrhages can occur, although their cause is unexplained.184
All patients undergoing surgery have a risk for thromboembolic events, but those with malignant gliomas are at significantly increased risk. Prophylaxis with low-dose heparin and external pneumatic leg muscle compression must be initiated promptly. The neurosurgical staff must maintain a high index of suspicion for phlebitis and pulmonary embolism so that treatment can be initiated early. Inferior vena cava filters may be placed to prevent the occurrence of pulmonary embolism. Full anticoagulation is preferable in patients seen more than 3 weeks after surgery.90,185
Wound infection and wound dehiscence occur rarely with craniotomies and develop in less than 1% of patients.178 The routine use of steroids in patients with intraparenchymal tumors apparently has little effect on overall wound healing.
Surgery for gliomas is rarely curative, and many patients with recurrences are subject to reoperation. However, studies have demonstrated that reoperation does not necessarily predispose patients to a greater complication rate.176,178,186
Meningiomas differ from parenchymal tumors in that they are often associated with venous sinuses, and thus venous infarction or injury to the sinuses is an additional risk. These tumors can invade the wall of sinuses and eventually narrow and obliterate the sinus lumen. When meningiomas are located in proximity to a sinus, preoperative venous angiography, magnetic resonance angiography, or magnetic resonance venography is essential to avoid complications. Entering a patent sinus can result in difficult bleeding that may require surgical reconstruction or bypass of the sinus. Sacrifice of a major venous sinus should be avoided. Complications associated with sacrificing a major venous sinus include increased ICP as a result of of brain edema and venous hemorrhagic infarction. Obtundation and seizures can develop in such patients (Table 22-3).187–189 Aggressive ICP management is essential in controlling this complication. Prudent surgical management may necessitate leaving a portion of the tumor adherent to the sinus and using adjuvant therapy or observation with surveillance MRI.190 Postoperative seizures are seen with convexity and parasagittal meningiomas.188 Sacrifice of a significant vein can result in venous infarction and an increased risk for seizures. The mortality rate for craniotomies performed for convexity and parasagittal meningiomas is 3.7% to 13%.188,191–198
Posterior Fossa Craniotomy
Leakage of CSF is seen frequently after a posterior fossa craniotomy and occurs in 3% to 15% of patients.199–201 Leakage can occur from the wound or be manifested as rhinorrhea or otorrhea. Openings into the mastoid air cells and air cells in the vicinity of the meatus can lead to otorrhea. Fluid can drain into the nasopharynx through the eustachian tube. Packing the mastoid air cells with bone wax can prevent CSF leakage. Aggressive drilling of the porus acusticus and larger tumor size have been associated with an increasing risk for CSF leaks.202 To minimize the risk for postoperative rhinorrhea, we apply bone wax aggressively to all mastoid air cells exposed during the craniectomy, as well as fibrin glue before closure. However, unroofing of air cells within the internal auditory canal can lead to persistent leakage, and we routinely apply a muscle plug, Gelfoam, and fibrin glue in this region to minimize the risk for leakage. In addition, routine prophylactic high-volume lumbar puncture may be performed daily for 3 days postoperatively to minimize the risk for leakage. When leakage occurs, management typically involves placement of a spinal drain. Operative repair may be necessary in patients who fail a trial of spinal drainage. Early recognition plus treatment of CSF leaks is imperative because CSF leakage places patients at risk for meningitis.201 Meningitis occurs in about 1% of patients, and early treatment with appropriate antibiotics is essential. Aseptic meningitis also occurs infrequently after surgery. Patients may have some elements of ataxia postoperatively, but these symptoms are usually limited and resolve within a few days. Significant headaches occur in half of patients postoperatively, and 25% complain of headaches persisting for more than a year after surgery.203
Mortality from infratentorial surgery is generally higher than that seen with supratentorial procedures. Compromise of the anterior inferior cerebellar artery and the resultant lateral pontine infarction are implicated in a third of postoperative deaths.204 The second biggest contributor to postoperative mortality is aspiration pneumonia resulting from lower cranial nerve deficits. Patients may require placement of a feeding tube and a tracheostomy to prevent aspiration pneumonia. Cerebellar contusions or hematomas can occur as a result of overaggressive retraction. Distant supratentorial hemorrhages occasionally occur for unclear reasons.205 Surgeons must be prepared to place an occipital ventricular catheter intraoperatively on an emergency basis if acute hydrocephalus results.
Transsphenoidal Surgery
Transsphenoidal surgery is commonly used to reach tumors in the sellar region. This procedure can be performed with extremely low mortality and low morbidity. Deaths have occurred in 0% to 1.75% of patients (Table 22-4). Laws206 reported 7 deaths in 786 procedures (0.9%), and Wilson207 reported 2 deaths (0.2%) in a series of 1000 patients. At our institution, 2 deaths occurred in 1800 procedures. Morbidities associated with the transsphenoidal approach are distinct from general neurosurgical complications because the approach is quite different from most transcranial approaches.
TABLE 22-4 Common Complication Rates in Transsphenoidal Surgery
| COMPLICATION | RATE (%) |
|---|---|
| Mortality | 0-1.75 |
| Nasal septum perforation | 1-3 |
| Sinusitis | 1-4 |
| Epistaxis | 2-4 |
| Visual disturbances | 0.6-1.6 |
| Transient diabetes insipidus | 10-60 |
| Permanent diabetes insipidus | 0.5-5 |
| Anterior pituitary insufficiency | 1-10 |
| Cerebrospinal fluid leakage | 1-4 |
| Meningitis | 0-1.75 |
Several complications can arise as a consequence of the transsphenoidal approach. If a sublabial incision is used, anesthesia of the upper lip and anterior maxillary teeth can occur, although this condition is usually transient.208 Removal of the superior cartilaginous septum may result in a saddle nose deformity.209 Perforation of the nasal septum occurs in 1% to 3% of patients and is more likely with reoperations.206 Postoperative sinusitis can occur in 1% to 4% of patients and may be reduced by postoperative antibiotics.210 Opening the speculum can result in diastasis of the maxilla or fracture of the medial orbital wall.206,211 Damage to the optic nerve or the carotid arteries can occur if the speculum is advanced too far. Inadequate removal of mucosa in the sphenoid sinus can lead to the postoperative formation of a mucocele.212
Vascular injuries represent serious morbidities and can lead to death. Intraoperative mucosal bleeding and delayed postoperative bleeding from the mucosal branch of the sphenopalatine artery can occur. If postoperative epistaxis persists, embolization of the internal maxillary artery may be necessary.213 Damage to the carotid arteries can occur in the sphenoid sinus or in the sella. Maintaining a midline trajectory is vital to avoid the carotid artery, and preoperative radiologic studies are essential in localizing the carotids. There are significant variations in the carotid’s parasellar course, and the distance between the two arteries may be as little as 4 mm.208 Frameless stereotaxis can be used to maintain a midline approach and may be especially useful in reoperations.214 Endoscopy is increasingly being used to minimize tissue trauma and to obtain more expansive views than those provided by microscopic visualization alone.215,216 Excessive arterial bleeding signals intraoperative injury to the carotid artery, and the only treatment involves packing the operative field.213 Other maneuvers are limited by the exposure, although if packing fails, ligation of the carotid may be required. Carotid artery injury can result in subarachnoid hemorrhage, vasospasm, false aneurysms, and carotid cavernous fistulas. A postoperative cerebral angiogram is essential to identify any of these complications.217 About 25% of deaths occurring during transsphenoidal operations are attributable to vascular injuries.21,213 Visual disturbances are also possible because of the close association of the chiasm, optic nerve, and pituitary. Damage can occur as a result of direct trauma, traction injury, or vascular compromise. Visual disturbances are more likely after reoperations because of adhesion formation between the chiasm and sella. Adhesions predispose the chiasm, optic nerve, and hypothalamus to traction injuries. In general, visual disturbances occur in 0.6% to 1.6% of patients.218 Postoperative visual loss can also signal the formation of a hematoma in the tumor bed. Such hematomas can be prevented by meticulous hemostasis. They can occur in 0.3% to 1.2% of cases.206,210,212 Injuries to the hypothalamus can also take place and potentially result in death.213 These patients are comatose and exhibit hyperthermia. Hypothalamic injury is the most common cause of death in patients undergoing transsphenoidal operations.213
Several complications can be anticipated in the postoperative period, and early recognition and appropriate treatment can circumvent catastrophic results. Patients should be closely monitored for diabetes insipidus (DI) with frequent serum sodium evaluations and careful accounting of patients’ fluid intake and urine output. An elevated serum sodium level or urine output may indicate DI. Temporary postoperative DI can occur in 10% to 60% of patients.210,219 Permanent DI is much less common and occurs in just 0.5% to 5% of patients.210 Delayed onset of the syndrome of inappropriate antidiuretic hormone secretion can also occur about a week postoperatively.213
Postoperative anterior pituitary insufficiency is one of the most commonly seen postoperative complications. Its incidence varies from 1% to 10%.206,207 Postoperative steroid therapy should be used in all postoperative patients until a thorough endocrine evaluation is complete. Adrenal insufficiency is a potentially serious complication if adequate steroid replacement therapy is not initiated.
CSF rhinorrhea is another commonly encountered complication of the transsphenoidal approach and occurs in 1% to 4% of patients.206,213 Intraoperatively, penetration of the arachnoid membrane can result in a gush of CSF into the operative field and the potential for postoperative CSF rhinorrhea. Packing the sella intraoperatively with an autologous fat graft and bone from the removed vomer can help prevent CSF leakage. Care must be taken to not overpack the sella, which may lead to compression of the chiasm.212 Patients in whom CSF rhinorrhea develops are first treated by spinal drainage for several days. Failure to close a CSF fistula with spinal drainage may indicate the need for reoperation and repacking of the sella. Early recognition and treatment of CSF rhinorrhea are important because a CSF leak can lead to meningitis. The incidence of meningitis in patients undergoing transsphenoidal surgery has been reported to be 0% to 1.75%.210,212,220 Patients with diabetes mellitus are at greater risk for the development of meningitis.
Cranial Base Surgery
The surgical approaches often call for brain retraction to adequately expose the lesion. Overly aggressive retraction can lead to tissue damage and infarction, with postoperative swelling resulting in increased ICP. Several maneuvers, including adequate bone removal, CSF drainage, and diuretics, can aid in achieving adequate exposure without excessive brain retraction. Resection of noneloquent brain tissue may be required to prevent contusions and possible postoperative herniation occurring from retraction injuries. Retraction can also compromise or injure venous outflow and result in venous stasis and hemorrhagic infarctions. This is especially important in regard to the vein of Labbé. Excessive retraction of the posterior temporal lobe can lead to tearing of the vein of Labbé and severe hemorrhagic temporal lobe edema.221
CSF leakage is one of the most common postoperative complications in cranial base surgery. The surgery often creates a communication between the CSF space and the facial sinuses. The sphenoid sinus is most commonly involved because of its association with the clivus and cavernous sinus.221 CSF leaks occur in about 8% of patients undergoing cranial base operations.221 A persistent CSF fistula may develop. Leaks generally occur in the immediate postoperative period, or they rarely develop months after surgery.221 CSF leaks are clinically manifested as clear spinal fluid draining from the nose, ear, or wound. The fluid can be collected on a pledget, and the presence of β2-transferrin confirms the discharge as CSF. Confirmatory radiographic examinations can be performed. Radioisotopic cisternography with cotton pledgets in the nasal cavity can corroborate the presence of a CSF leak. CT cisternography with intrathecal metrizamide or magnetic resonance cisternography can be used to localize the leak.222
Pneumocephalus is another postoperative complication frequently encountered in cranial base surgery. Air may be found in the extradural or intradural spaces. Intracranial air can produce alterations in a patient’s mental status that result in lethargy or agitation. Some degree of pneumocephalus is commonly found on postoperative CT, and the air is usually reabsorbed quickly. Patients operated on in the sitting position have a higher incidence of pneumocephalus.223 Increasing amounts of intracranial air signal the presence of a communication between the subarachnoid space and air sinuses and implies an undetected CSF leak. Having patients lie flat in bed and discontinuing external spinal drainage can facilitate the absorption of intracranial air. Passing a spinal needle through the bur-hole site into the air pocket can decompress the subdural air in the event of a tension pneumocephalus.221
Skull base lesions often involve the cranial blood vessels. Tumors can encase or displace these vessels, and adequate tumor removal may require sacrifice of vessels. The neurosurgeon must know the consequences of sacrificing cranial base blood vessels to minimize morbidity. Sacrifice of vessels can result in ischemic neurological deficits and infarctions in a vascular territory or watershed distribution. Preoperatively, balloon occlusion testing and xenon-enhanced CT cerebral blood flow testing can determine whether patients can tolerate sacrificing a blood vessel. Patients in whom neurological deficits develop with the balloon occlusion test or who have cerebral blood flow of less than 35 mL/100 g per minute cannot tolerate vessel sacrifice and may require a bypass graft.224
Cranial nerve morbidity is commonly encountered with cranial base surgery, and the dysfunction may be temporary or permanent. Accurate preoperative cranial nerve examination is important because postoperative dysfunction is more likely in patients with preoperative deficits. Neurophysiologic monitoring is an important adjuvant for localizing cranial nerves and preventing injury. Cranial nerve VII may be monitored via continuous facial electromyographic responses. A nerve stimulator can help locate the facial nerve. Cranial nerve XI can be localized with a nerve stimulator and observation of shoulder twitching.198
Cranial nerve injury can occur as a result of nerve retraction or direct injury during tumor dissection. Cranial nerves may also be injured by compromise of the nerves’ blood supply during surgical dissection distant from the nerves. Damage to the cranial nerves is especially significant during surgery in the cavernous sinus. Optic nerve damage occurs in 0% to 6% of patients.197,225 Permanent damage involving extraocular nerve function (i.e., cranial nerves III, IV, and VI) occurs in 20% to 30% of patients.196,197 The incidence of V1 neuropathy is 8% to 20%.196,197,225
Certain cranial nerves are more susceptible to injury than others. Cranial nerves I, II, and VIII are very sensitive to injury. Minimal manipulation can result in profound deficits, and the loss of function is often irreversible. Cranial nerves III, IV, and VI are less sensitive to manipulation, and some recovery typically occurs postoperatively if the nerve’s continuity is maintained. Injury to these nerves results in diplopia. Loss of cranial nerve IV function can be corrected by tilting the head or the use of prism glasses. Oculoplastic procedures may be necessary to correct persistent diplopia caused by injury to cranial nerve III or VI. Cranial nerve V damage is generally well tolerated, with the exception of damage to the V1 segments, which mediate the corneal reflex. Damage to the V1 division results in corneal sensory dysfunction, and patients must have meticulous eye care to prevent corneal abrasions and loss of vision in the desensitized eye.221
Unilateral injury to cranial nerve XII is generally well tolerated. When combined with other cranial nerve injuries, such as injury to cranial nerves VII, IX, or X, significant dysarthria can occur. Bilateral cranial nerve XII injury results in severe functional limitation and ultimately requires a tracheostomy and placement of a feeding tube.221
Cranial base surgery can cause morbidity from TMJ manipulation. Dislocation of the TMJ can result in postoperative trismus. Resection of the mandibular condyle may be preferred because it avoids retraction of the mandible and associated postoperative trismus. Resection of the condyle leads to a contralateral jaw deviation but no functional loss.221
Complications of Stereotactic Brain Surgery
A stereotactic frame is applied to the patient, and CT or MRI is performed. The most commonly used frames are the Leksell (Elektra Instruments, Atlanta, GA) and the Brown-Roberts-Wells (Radionics, Burlington, MA) systems.226 The fiducial markers on the frame are registered into the system and allow accurate three-dimensional navigation and localization in reference to the neuroimaging. Proper application of the stereotactic frame and precise registration are essential to achieve accurate results. Frameless systems that use cutaneous fiducial markers are available, as well as some that use surface landmarks alone, with no need to place cutaneous fiducial markers.
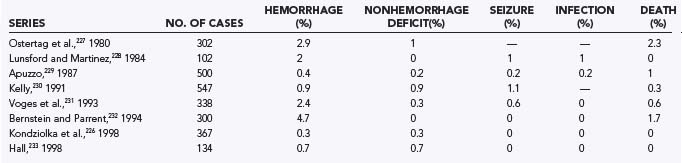
One of the most commonly performed stereotactic procedures is brain biopsy. Brain biopsies are safe and effective procedures. The procedure can usually be performed under monitored anesthesia care and can avoid the complications associated with general anesthesia. CT or MRI is used to stereotactically guide biopsy of a lesion through a small bur hole. Possible complications include hemorrhage, neurological deficits, seizures, and infections.226 The mortality rate in several large series has been less than 1%, and complication rates vary from 0% to 7% (Table 22-5).226–233 Seizures and infections are rare during brain biopsy. The most serious complication usually involves postoperative hematoma formation. Properly performed brain biopsies are more than 90% effective in establishing a tissue diagnosis in patients with radiographic lesions.226
Preventing complications related to brain biopsy requires adequate preoperative planning. Only patients in whom the results of brain biopsy may change medical management should undergo biopsy. Because thrombocytopenia or coagulopathies predispose patients to intracranial hemorrhage, all candidates should have normal coagulation profiles and platelet counts. Preoperative radiographic imaging is essential to rule out vascular lesions that may result in serious hemorrhage when biopsied. The planned trajectory must avoid vessels and important structures. Intraoperative hypertension may predispose patients to hemorrhage.226
When bleeding is discovered during a brain biopsy, allowing the blood to drain out of the needle may prevent the formation of a hematoma.226 Craniotomy may be required to control persistent hemorrhage. Instillation of thrombin through the biopsy canula has been used to control hemorrhage.234 Routine postoperative CT can be performed to rule out hematoma formation, and asymptomatic hematomas are often discovered postoperatively. Neurological deficits develop in about 10% of patients with asymptomatic postoperative hematomas.235 Most postoperative hematomas are managed by observation and serial CT.
Brain biopsies are increasingly being performed on patients infected with human immunodeficiency virus (HIV), who may be subject to several central nervous system infections or neoplasms. Biopsies in patients with acquired immunodeficiency syndrome have higher complication rates. Skolasky and coworkers reviewed 435 HIV-positive patients undergoing biopsy and determined that the morbidity rate was 8.4% and the mortality rate was 2.9%.236 Complications were associated with preoperative poor functional status and thrombocytopenia. It is not clear whether the presence of HIV infection predisposes to higher complication rates.
Stereotactic Radiosurgery
Stereotactic radiosurgery is a safe and effective treatment modality for vascular malformations, brain tumors, and in some cases, functional surgery. Stereotactically applied radiation provides precise delivery of high-dose radiation to a well-defined target. Complications in radiosurgery are related to the effects of radiation on the brain and structures in proximity to the lesion. Significant early complications rarely occur but can include seizures or worsening neurological deficits. Approximately a third of patients experience mild transitory symptoms, including headaches, nausea, and dizziness.237 Late complications develop 6 to 9 months after the procedure and can include facial palsy, trigeminal neuropathy, and visual symptoms.226 Exposure of the optic nerve to more than 8 to 10 Gy of radiation leads to visual deterioration and optic neuropathy.238,239 Patients may become symptomatic from radiation necrosis or local brain edema. In a review of 1600 patients undergoing radiosurgery with at least a 3-year follow-up, the rate of significant morbidity was 1.9%.226 The risk for carcinogenesis secondary to radiosurgery is estimated to be less than 1 in 1000.240
Gamma Knife radiosurgery has been applied effectively to the treatment of acoustic neuromas. The complications associated with acoustic neuroma radiosurgery are related to exposure of cranial nerves to radiation. The rate of facial nerve paresis after 5-year follow-up has been 21%, and the rate of trigeminal dysfunction has been 27%. Hearing was preserved in 51% of patients undergoing radiosurgery for acoustic neuromas.241,242 Peritumoral edema after radiosurgery has occasionally led to hydrocephalus.243 There is a significant increase in mass effect and tumor size, approximately 43%, after high-dose Gamma Knife radiosurgery for vestibular schwannomas that correlates with deterioration of facial and trigeminal function. The effect is much smaller at lower doses.244 Because tumor control is greater with larger doses of radiation, fractionated stereotactic radiosurgery is usually performed to allow increased control of growth while minimizing risk to the facial, cochlear, and trigeminal nerves.245 Intracanalicular tumors may be associated with higher cranial nerve morbidity when treated with radiosurgery.246 Improvements in target imaging and reduction in doses have led to lower cranial nerve morbidity.241,243
Radiosurgery has also been applied to cranial base meningiomas. The morbidity rate is about 5% to 8%.238,239,247,248 Most complications involve transient cranial nerve palsies and occur 3 to 31 months after surgery. High radiation doses applied to Meckel’s cave increase risk for the development of trigeminal neuropathy.239 Radiosurgery is also used to treat gliomas and brain metastasis. Preliminary reports indicate a morbidity rate of about 10% and a mortality rate of 1%.249 Early complications can involve increased ICP, which may lead to death.250 Radiotherapy for brain parenchymal lesions can result in seizure complications. Patients with lesions in the motor cortex are especially susceptible to seizures after radiosurgery.251 Gamma Knife radiosurgery for trigeminal neuralgia is generally well tolerated and associated with minimal morbidity. Loss of facial sensation has been reported infrequently.252
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree