Chapter 8 Behavior and Personality Disturbances
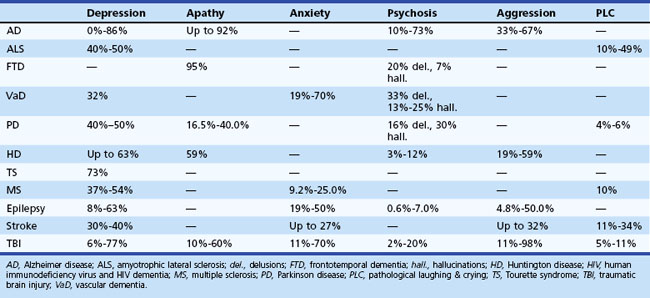
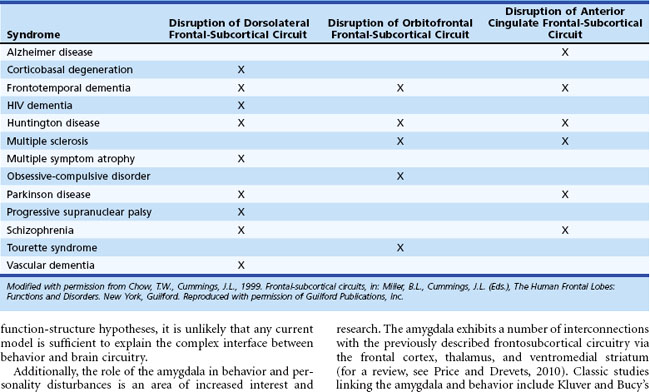
Behavioral and personality disturbances commonly occur in individuals with neurological disease or injury (Table 8.1). Identification and treatment of behavioral disturbances are critical because they are frequently associated with reduced functional capacity, decreased quality of life, and greater economic cost, caregiver burden, and morbidity. Dysfunction of various brain circuits, most notably the frontosubcortical and amygdaloid circuits, as well as psychological factors may contribute to increased rates of disturbances.
Frontosubcortical Circuitry
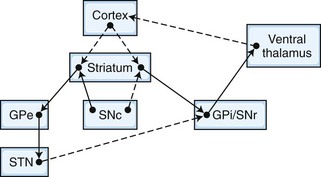
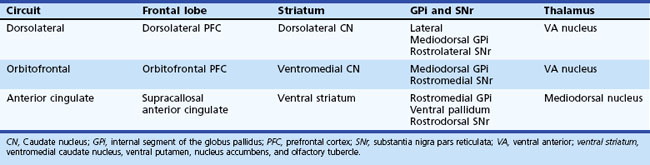
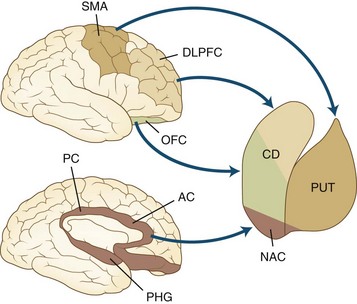
The frontosubcortical circuits provide a unifying framework for understanding the behavioral changes that accompany cortical and subcortical brain dysfunction. In the past 3 decades, a number of significant advances have been made in our understanding of the neuroanatomy, neurophysiology, and chemoarchitecture of the frontosubcortical circuits. An increasingly broad spectrum of neuropsychiatric phenomenology is now being interpreted in the context of dysfunction in this region. A brief overview of the frontosubcortical circuits and their signature behavioral syndromes is offered as a strategy to better understand the behavior and personality changes that accompany neurological conditions. Alexander and colleagues described five discrete parallel circuits linking regions of the frontal cortex to the striatum, the globus pallidus and substantia nigra, and the thalamus. These circuits consist of “direct” and “indirect” pathways. In general, the direct pathway facilitates the flow of information, and the indirect pathway inhibits it. The overall model for the frontosubcortical circuits can be observed in Fig. 8.1.
Five frontosubcortical circuits were initially described as motor, oculomotor, dorsolateral prefrontal, lateral orbitofrontal, and anterior cingulate gyrus. Table 8.2 gives descriptions of specific neuroanatomic pathways for these circuits. Efforts to link functional domains to this brain circuitry have been developed and revised over the past few decades. Disruption of dorsolateral prefrontal, lateral orbitofrontal, and anterior cingulate gyrus circuits is associated with behavioral and personality disruptions. Specific behavioral syndromes have been attributed to dysfunction in these circuits (Box 8.1) (Mega and Cummings, 2001). Disruptions at any point in the circuit (e.g., the frontal cortex, corpus striatum, globus pallidus) may result in alterations of behavior.
Box 8.1 Behavioral Syndromes Associated with Dysfunction of the Motor Circuits
Disruption of the dorsolateral circuit (Fig. 8.2) is associated with executive dysfunction, including poor planning and organization skills, memory retrieval deficits, and poor set shifting. Table 8.3 lists neurological disorders associated with disruption of this circuit. The orbitofrontal circuit (see Fig. 8.2) is associated with increased irritability, impulsivity, mood lability, tactlessness, and socially inappropriate behavior, whereas disruptions of the latter part of the orbitofrontal circuit may also result in mood disorder or obsessive-compulsive disorder (OCD) or both. See Table 8.3 for disorders associated with disruption of this circuit. Finally, the anterior cingulate gyrus circuit is associated with decreased motivation, apathy, decreased speech, and akinesia. See Table 8.3 for disorders associated with disruption of this circuit. Although these models may be heuristic in developing function-structure hypotheses, it is unlikely that any current model is sufficient to explain the complex interface between behavior and brain circuitry.
Additionally, the role of the amygdala in behavior and personality disturbances is an area of increased interest and research. The amygdala exhibits a number of interconnections with the previously described frontosubcortical circuitry via the frontal cortex, thalamus, and ventromedial striatum (for a review, see Price and Drevets, 2010). Classic studies linking the amygdala and behavior include Kluver and Bucy’s early work with monkeys with bitemporal lesions. Following selective lesions to the amygdala, monkeys exhibited less caution and fear when exposed to unfamiliar stimuli. Human case studies of individuals with amygdala lesions have also been described and have revealed similar findings. One individual with bilateral amygdala damage exhibited difficulty in recognition of fear and exhibited increased social interactions with features of disinhibition (Adolphs, 2010). Researchers have long implemented the amygdala in anxiety and fear. For example, changes in amygdala volume and functioning have been observed in posttraumatic stress disorder (PTSD) (Shin, Rauch, and Pitman, 2006). More recently, research has implemented the amygdala in a wider range of emotional and behavioral responses and syndromes. Although findings have been somewhat mixed, the amygdala has been implicated in mood disorders including depression and bipolar disorder (Hamidi, Drevets, and Price, 2004).
The current chapter focuses on behavioral and psychiatric changes in neurological disease and injury. Please see Chapter 34 for detailed information on assessment and description of common cognitive changes observed in neurological disease and injury.
Assessing Behavior and Personality Disturbances in Patients with Cerebral Dysfunction
Several factors present challenges in the identification and diagnosis of behavior and personality disturbances in neurological samples. First, there is significant overlap between other symptoms of cerebral dysfunction and symptoms of behavior and personality disturbances. For example, psychomotor retardation or reduced energy, libido, or appetite might reflect the underlying illness or injury (i.e., TBI, Parkinson disease [PD]) or they may reflect a depressive disorder. Second, cognitive symptoms may confound the detection of behavioral changes. For example, language and cognitive deficits occurring in individuals with cerebral dysfunction can affect the ability to fully assess for changes in mood or insight. In these situations, observed behavior and collateral report must be heavily considered when assessing for behavioral or personality disturbances. Third, the validity of the behavioral dysfunction assessed can vary depending upon the source. Ample research shows that clinical ratings acquired from the patient, a collateral or spouse, and a healthcare worker can vary widely (see, for example, Hoth et al., 2007). Patients with cerebral dysfunction may have impaired insight; thus, they may underreport behavioral difficulties. Similarly, caregivers may also provide biased information, as their current mood or degree of caregiver burden may influence their reporting of behavioral symptoms.
Assessment of Depression
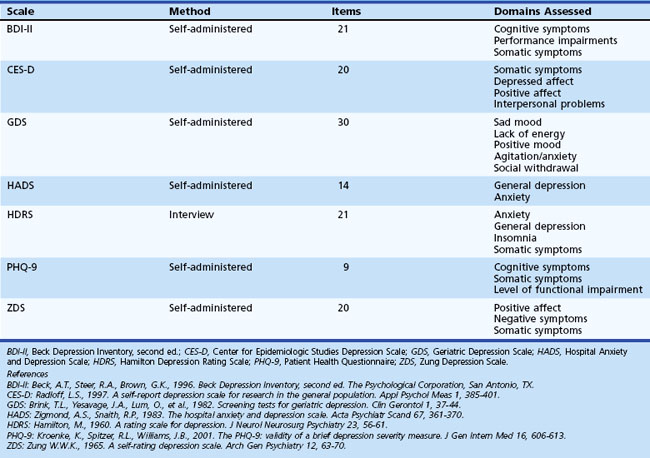
Symptoms of neurological illness or injury may manifest as depression. In fact, depression is frequently a very early symptom or precedes onset of illness in Huntington disease (HD) (Berrios et al., 2001), PD (Ishihara and Brayne, 2006), and Alzheimer disease (AD) (Green et al., 2003). There are several scales available for the assessment of mood disorders that might be useful in patients with acquired cerebral dysfunction. Although clinicians may not have enough time to thoroughly assess altered mood, self-report scales can be helpful in determining which symptoms are present and how bothersome or severe each symptom is. Table 8.4 offers additional information regarding these scales. Individuals scoring highly on these self-report measures may benefit from referral for additional evaluation and possible intervention by mental health professionals.
Domains assessed by the different measures vary such that certain scales may not detect some symptoms of depression. Two of the most commonly used measures are the Beck Depression Inventory (BDI) and the Hamilton Depression Rating Scale (HDRS). Research suggests that the BDI may be a useful screening tool in PD and Tourette syndrome, and the HDRS may be an appropriate screening tool in PD. However, these measures assess several symptoms such as psychomotor retardation and reduced energy that are common in neurological illness and injury. Thus, care must be taken to be certain that these measures do not suggest the person is depressed based on symptoms of neurological syndrome or injury. The Geriatric Depression Scale (GDS) was developed to be used in elderly populations and may be a useful screening tool for patients with early dementia and PD. The Patient Health Questionnaire (PHQ-9) is a self-report measure designed to be used in primary care settings and may be appropriate in neurological settings. See Chapter 9 for more detailed information on depression in neurological settings.
Assessment of Other Behavioral and Personality Disturbances
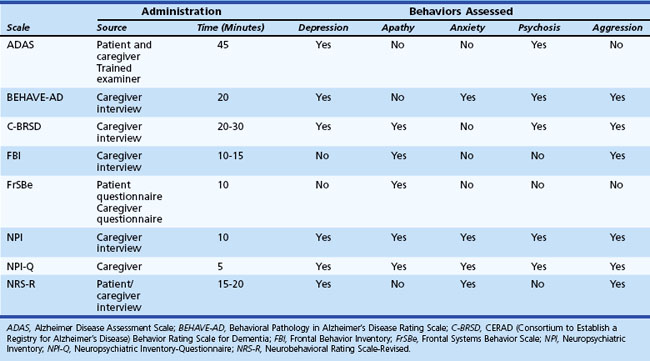
In addition to depression, other behavioral and personality disturbances occur in patients with cerebral dysfunction, and several measures have been created to assess them (Table 8.5). These measures were specifically designed to assess behavioral symptoms in AD: Alzheimer’s Disease Assessment Scale (ADAS); Behavioral Pathology in Alzheimer’s Disease Rating Scale (BEHAVE-AD); CERAD Behavior Rating Scale for Dementia (C-BRSD); general dementia: Neuropsychiatric Inventory (NPI); frontal lobe dementia: Frontal Behavior Inventory (FBI); TBI: Neurobehavioral Rating Scale-Revised (NRS-R); and damage to frontal regions: Frontal Systems Behavior Scale (FrSBe). Some measures such as the NPI and the FrSBe have been implemented in diverse conditions including AD, PD, HD, and multiple sclerosis (MS). In addition, the NPI, which is available in an interview and a questionnaire format, has been frequently used as an outcome measure in clinical trials. These measures might be useful ways to screen for a wide variety of potential behavioral disruptions among patients with neurological illness or injury.
Behavior and Personality Disturbances Associated with Cerebral Dysfunction
Alzheimer Disease
Based on 2000 census data, it is estimated that AD affects 5.1 million individuals in the United States (Hebert et al., 2003). Patients with AD experience a wide range of behavioral disturbances, including affective symptoms, agitation, aggression, and psychosis. Behavioral disturbances in AD are associated with increased caregiver burden, patient and caregiver abuse, greater use of psychotropic medications, more rapid cognitive decline, and earlier institutionalization. The relationship between behavioral changes in AD and neuropathological markers is equivocal. Some researchers report a correlation between behavioral changes in AD and increased white matter hyperintensities (WMH) (Berlow et al., 2009), while others have not observed this relationship (Staekenborg et al., 2008). Many studies do not document a correlation between the presence or absence of behavioral symptoms and whole brain or hippocampal volume (Berlow et al., 2009; Staekenborg et al., 2008). In contrast to frontotemporal dementia (FTD), social comportment is relatively spared in AD.
Use of atypical antipsychotic medications have historically been the preferred method of treatment for behavioral disturbances in AD including irritability, aggression, and psychosis. However, use of atypical antipsychotic medications in elderly adults may be associated with a nearly twofold increase in risk for mortality (Kuehn, 2005). Additionally, a multisite study of atypical antipsychotics (olanzapine, quetiapine, and risperidone) showed no significant difference in Clinical Global Impression Scale scores for any antipsychotic medication over a placebo group (Schneider et al., 2006). Moreover, significantly more participants found the side effects of the atypical antipsychotic medications to be intolerable compared to the placebo group (Schneider et al., 2006). In a retrospective observational study, behavioral symptoms were reduced in one-fifth to one-fourth of patients following treatment with antipsychotics, while a full half of participants exhibited worsening of symptoms (Kleijer et al., 2009). However, other retrospective observational studies have reported improvements in 33% to 43% of individuals with AD and behavioral disturbances treated with atypical antipsychotics (Rocca et al., 2007). The U.S. Food and Drug Administration (FDA) has issued a black-box warning on the use of antipsychotics in elderly persons with dementia. Antipsychotics may be beneficial in a small subgroup of individuals, but care must be taken in prescribing such medications, owing to the potential side effects in the context of questionable effectiveness. A review of the clinical trial literature for cholinesterase inhibitors and memantine suggests that individuals treated with these pharmaceuticals typically do experience a reduction in behavioral symptoms, including improved mood and abatement of apathy (Cummings, Mackell, and Kaufer, 2008).
Although the neurodegenerative process itself can be the cause of behavioral disturbances in AD, other causes must be explored: premorbid psychiatric diagnoses, medication side effects, or medical comorbidities to name a few. In many situations, behavioral disturbances may reflect an individual with impaired cognitive and language abilities attempting to communicate information to their providers (Sutor, Nykamp, and Smith, 2006). Given the nature of these behavioral disturbances and the limited availability of pharmacological interventions, behavioral interventions and environmental modifications may be among the most helpful strategies in managing undesired behaviors. Detailed discussion of such behavioral interventions is beyond the scope of this chapter, but for more detailed information, readers may wish to review Sutor and colleagues (2006).
Clinicians may wish to refer patients to geriatric psychiatry and/or neuropsychology providers for identification and implementation of behavioral and environmental interventions. Common environmental interventions include use of familiar and personal belongings readily viewable in the environment to reduce confusion and agitation. Similarly, minimizing background distracters and establishing a standard predictable routine may also be helpful in reducing confusion and agitation. It is not uncommon for undesired behaviors (e.g., aggression) to receive significant attention while preferred behaviors (e.g., working on quiet activity) receive no reinforcement. To successfully reduce undesired activities, individuals need to increase desired activities through reinforcing preferred behavior, offering desired activities, and reducing reinforcement of undesired behavior. Finally, redirection is frequently attempted in individuals with cognitive impairment who are engaging in undesired activities. Redirection is likely to be most successful if done in a multistep process involving validation of emotion, joining of behavior, distraction, and only then followed by redirection (Sutor, Nykamp, and Smith, 2006). Table 8.6 lists more detailed information.
Table 8.6 Multistep Approach for Redirecting Patients with Dementia
| Step | Description and Example |
|---|---|
| Validate | Validation of the individual’s emotional state to establish rapport Example: “You look worried.” |
| Join | Join the patient’s behavior. Example: “You’re looking for your children? Well, I’m trying to find something too. Let’s look together.” |
| Distract | Distraction is easier after establishing a common goal. This works best when individuals have significant cognitive impairment. Example: “Let’s look over there where they are having coffee.” |
| Redirect | At this stage, redirection may be possible. Example: “That coffee smells good; do you want a cup?” |
Reprinted with permission from Sutor, B., Nykamp, L.J., Smith, G.E., 2006. Get creative to manage dementia-related behaviors. Curr Psychiatry 5, 81-96.
Depression
The true prevalence of depression in AD is controversial, with estimates up to 86%. One reason for the mixed findings lies in the different methods employed to assess depression in AD, such as family interviews and patient self-report. Some symptoms of depression are confounded with components of AD (e.g., concentration, energy, interest). The probability of depression in AD appears to be greater if there is a history of depression either in the patient or in the family. Table 8.7 suggests differences between the signs of depression and possibly confounding signs of dementia. Interestingly, there does not appear to be a clear relationship between depressive symptoms and severity of AD (Verkaik et al., 2007). Depression is associated with greater social and functional impairments in patients with AD (Starkstein et al., 2005), although others have not observed a correlation between depression and functional impairment (Landes, Sperry, and Strauss, 2005).
Table 8.7 Clinical Aspects Differentiating Dementia from Depression
| Major Depression | Dementia |
|---|---|
| Acute, nonprogressive | Insidious and progressive |
| Affective before cognitive | Cognitive before affective |
| Attention impaired | Memory impaired |
| Orientation intact | Orientation impaired |
| Complains of memory | Minimizes/normalizes memory |
| Gives up on testing | Obvious effort on testing |
| Language intact | Aphasic errors |
| Better at night | Sundowning |
| Self-referred | Referred by others |
Selective serotonin reuptake inhibitors (SSRIs) are the preferred mode of treatment for depression in AD. Although clinical trials are relatively few, sertraline and citalopram have been shown to be effective (Lyketsos et al., 2000).
Apathy
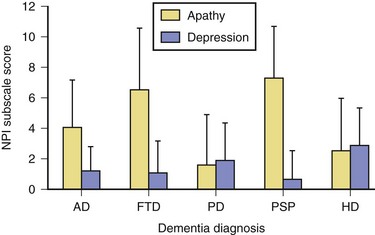
Apathy, defined as diminished motivation not attributable to decreased level of consciousness, cognitive impairment, or emotional distress, is among the most common behavioral changes noted in AD. Assessment of apathy in AD may be difficult because it may be unclear whether decreased activity is due to apathy or inability to perform activities. Consistent with expectations based on frontal-subcortical circuitry, apathy in AD has been shown to be associated with bilateral reductions in gray matter volume in the anterior cingulate cortex, orbitofrontal cortex, dorsolateral prefrontal cortex, and putamen (Bruen et al., 2008). Apathy in AD is associated with greater functional and cognitive impairment (Landes et al., 2005) as well as lower quality of life (Hurt et al., 2008).
Aggression
Aggressive verbalizations and acts are common in AD. Reported prevalence rates range from 25% to 67%, and studies have indicated that verbal aggression is more common in men and in individuals with delusions or agitation (Eustace et al., 2001) and is associated with increased placement in skilled nursing facilities. Sertraline has been associated with a 38% response rate for the treatment of aggression and irritability in AD (Lanctot et al., 2002).
Psychosis
Prevalence rates of psychotic symptoms in AD range from 10% to 73%, with rates in clinical populations exceeding community-based samples. Interestingly, hallucinations and delusions are significantly less common among individuals with early-onset AD (Toyota et al., 2007). Once present, delusions recur or persist for several years in most patients with AD (Fig. 8.3). The presence of hallucinations is associated with increased placement in skilled nursing centers.
Previously it was believed that individuals with AD experienced delusions secondary to significant cognitive difficulties. However, more recent research has identified additional correlates and biological markers of psychosis. Evidence from neuropsychological investigations suggests more executive and frontal dysfunction in AD with psychotic symptoms than AD without these symptoms. For example, delusions have been associated with reduced gray matter volume in the inferior right frontal gyrus and the inferior parietal lobule (Bruen et al., 2008). The presence of delusions in AD is associated with poorer performance on the Frontal Assessment Battery (FAB) but was not related to global measures of cognitive impairment (i.e., MMSE) (Nagata et al., 2009). Persons with AD and hallucinations are at significantly increased risk for mortality; however, delusions alone are not associated with increased mortality (Wilson et al., 2005)
The most common psychotic symptoms reported in patients with AD are delusions and hallucinations. The delusions are typically paranoid-type, non-bizarre, and simple. Complex or bizarre delusions seen in patients with schizophrenia are conspicuously absent in patients with AD. Misidentification phenomena, however, are common in AD. Whereas hallucinations in AD are more often visual than auditory, the reverse is true for schizophrenia (Table 8.8).
Table 8.8 Psychotic Symptoms in Alzheimer Disease versus Schizophrenia in Elderly Patients
| Psychosis in Alzheimer Disease | Schizophrenia in the Elderly | |
|---|---|---|
| Incidence | 30%-50% | <1% |
| Bizarre or complex delusions | Rare | Common |
| Misidentification of caregivers | Common | Rare |
| Common form of hallucinations | Visual | Auditory |
| Schneiderian first-rank symptoms | Rare | Common |
| Active suicidal ideation | Rare | Common |
| History of psychosis | Rare | Very common |
| Eventual remission of psychosis | Common | Uncommon |
| Need for many years of maintenance on antipsychotics | Uncommon | Very common |
| Average optimal daily dose of an antipsychotic | 15%-25% of that in young adult with schizophrenia | 40%-60% of that in a young adult with schizophrenia |
Reprinted with permission from Jeste, D.V., Finkel, S.I., 2000. Psychosis of Alzheimer’s disease and related dementias. Am J Geriatr Psychiatry 8, 29-34.
Frontotemporal Dementia
Frontotemporal lobar degeneration (FTLD) is a heterogeneous group of syndromes including semantic dementia (SD), progressive nonfluent aphasia (PNFA), and behavioral variant frontotemporal dementia (bvFTD). Consensus criteria for diagnosis of FTD have been described, with presence of behavioral change an important feature. While changes in personality and behavior are most commonly described in bvFTD, behavioral change has been reported across all FTLD syndromes to varying degrees. Caregiver distress is greater among individuals with FTLD and behavioral changes, particularly apathy and disinhibition, versus those with primarily aphasic difficulties (Massimo et al., 2009).
Behavioral Disruption
Atrophy within the frontal lobes leads to disruption of the frontosubcortical circuits and the characteristic behavioral syndromes in FTLD. Two classic behavioral syndromes have been described among individuals with FTD: an apathetic and a disinhibited subtype. Apathy is a very common symptom in individuals with FTD. Individuals may show little concern for personal hygiene and may appear unkempt. Moreover, symptoms of orbitofrontal syndrome, such as disinhibition, poor impulse control, tactlessness, and poor judgment are common. Loss of empathy, mental inflexibility, and stereotyped behaviors are also common. Symptoms similar to those observed in Klüver-Bucy syndrome, such as hyperorality and hypersexuality, may occur in late stages. Frequently the family members and caregivers are the ones who report these behavioral disturbances, as many patients with FTD experience reduced insight into their current difficulties. Behavioral change to varying degrees has been described in all FTLD syndromes, including SD and PNFA (Kertesz et al., 2010), although they frequently are less severe and/or occur later in the progression of the illness.
No curative treatments exist for FTLD. However, there has been some success with pharmacological intervention for behavioral dyscontrol. Although few large-scale studies have been completed, evidence suggests that behavioral disturbances such as disinhibition, overeating, and compulsions may show some response to treatment with SSRIs (Huey, Putnam, and Grafman, 2006).
Anosognosia
As noted in the consensus criteria, individuals with FTD frequently exhibit anosognosia. This loss of insight may reflect psychological denial of illness, inability to perceive symptoms, or lack of concern for their current difficulties. Among individuals with FTLD, individuals with bvFTD exhibit greater anosognosia than individuals with the aphasic subtypes of FTLD (Zamboni et al., 2010). Patients with FTD frequently describe significantly fewer problems with cognition and behavior than what their caregivers describe. Moreover, this observed discrepancy between patient and caregiver report is greater among individuals with FTD than in individuals with AD, particularly for language, behavior, and functioning difficulties (Salmon et al., 2008). Severity of anosognosia is not typically associated with severity of dementia (Zamboni et al., 2010). The relationship between impaired awareness and specific neuropathology is somewhat unclear. Some studies have shown an association between impaired awareness and right frontal disruptions (Mendez and Shapira, 2005) while others have shown a link between anosognosia and involvement of the right temporoparietal cortex (Zamboni et al., 2010).
Relationship to Primary Pathology
From a pathological perspective, individuals with FTLD vary with regard to the degree to which the frontal versus temporal lobes and right versus left hemispheres are affected. Significant research has looked at the relationship between patterns of behavioral syndromes and underlying neuropathology (see Josephs, 2007 for a review). Individuals with bvFTD typically exhibit greater frontal versus temporal atrophy, which is typically symmetrical. There is emerging evidence to suggest that individuals with bvFTD and primarily apathetic behavioral changes show greater frontal involvement, particularly right dorsolateral prefrontal cortex (Zamboni et al., 2008; Massimo et al., 2009). Individuals with primarily disinhibited behavioral change show greater involvement of the right mediotemporal limbic and temporal lobe (Zamboni et al., 2008), although others have described increased atrophy within the left dorsolateral prefrontal cortex (Massimo et al., 2009). Individuals with SD most typically exhibit atrophy and dysfunction within the left anterior temporal lobe, while individuals with SD and behavioral changes are more likely to also exhibit changes in the ventromedial and superior frontal lobes. Individuals with PNFA are most likely to show changes in left frontal and perisylvian areas.
Vascular Dementia
Depression
The mean reported prevalence of depression in VaD is 32%, although rates vary widely between studies (Ballard and O’Brien, 2002). Sample source likely influences the reported prevalence rates, with community samples endorsing lower rates of depression than clinic samples. Individuals with VaD and depression are less likely to have had a stroke and are more likely to have a prior history of depression and impairments in memory or attention than patients with VaD without depression. The relationship between age and depression in VaD is unclear, with increased rates of depression being reported in both younger and older samples.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree