Chapter 18 Brachial Plexus
Overview of the Brachial Plexus
The brachial plexus is a union of the ventral rami of the lower four cervical nerves and the greater part of the first thoracic ventral ramus (Figs 18.1, 18.2). The fourth ramus usually gives a branch to the fifth, and the first thoracic frequently receives one from the second. These ventral rami are the roots of the plexus; they are almost equal in size but variable in their mode of junction. Contributions to the plexus by C4 and T2 vary. When the branch from C4 is large, that from T2 is frequently absent and the branch from T1 is reduced, forming a ‘prefixed’ type of plexus. If the branch from C4 is small or absent, the contribution from C5 is reduced, that from T1 is larger and there is always a contribution from T2; this arrangement constitutes a ‘postfixed’ type of plexus.
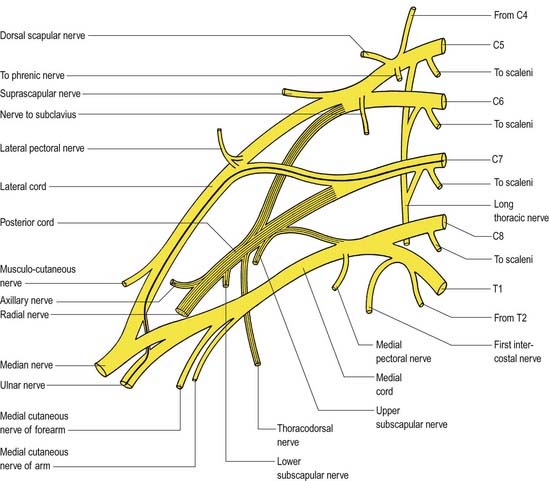
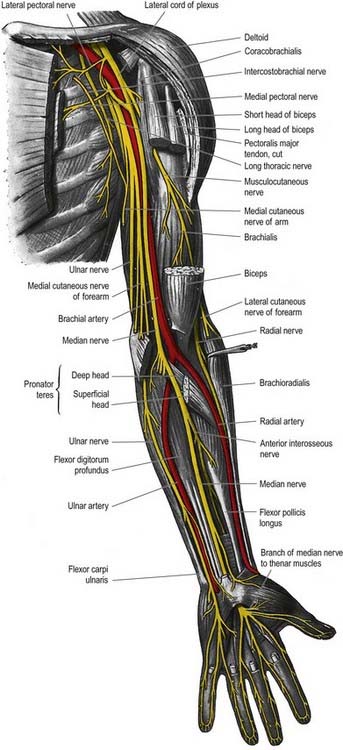
Fig. 18.1 Plan of the brachial plexus. The posterior division of the trunks and their derivatives are shaded; the fibres from C7 that enter the ulnar nerve are shown as a heavy black line. C4 to C8 and T1 and T2 indicate the ventral rami of these cervical and thoracic spinal nerves.
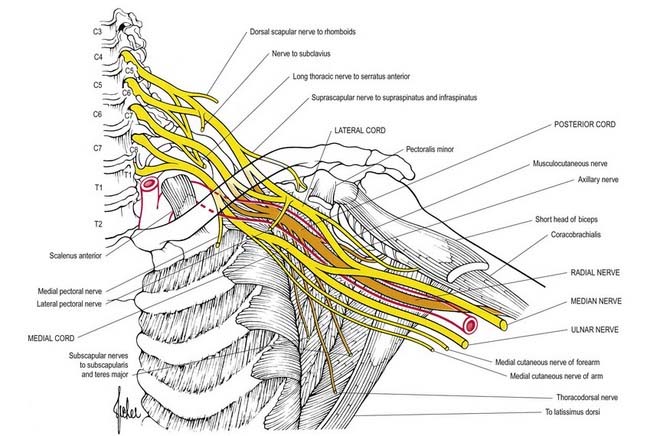
Fig. 18.2 Diagram of the brachial plexus, its branches and the muscles they supply.
(From Aids to the Examination of the Peripheral Nervous System, 4th ed. 2000. Saunders, London.)
Overview of the Principal Nerves
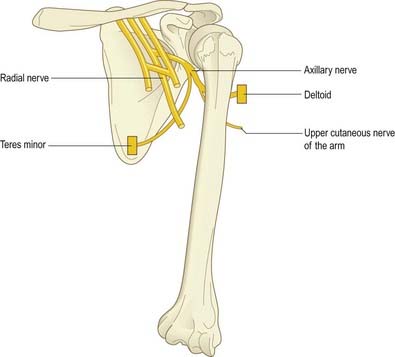
Axillary Nerve (C5, C6)
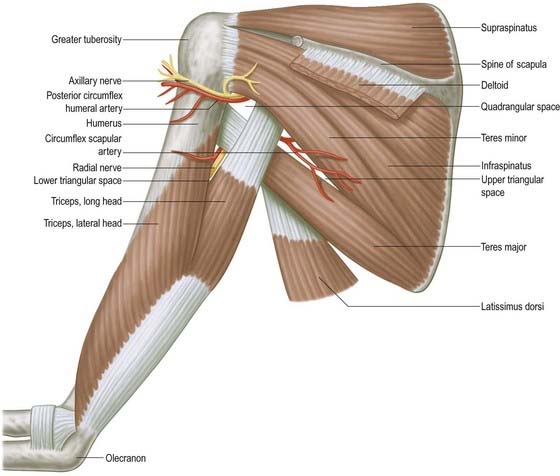
The axillary nerve is a branch of the posterior cord of the brachial plexus. It winds posteriorly around the neck of the humerus together with the circumflex humeral vessels and supplies the deltoid and teres minor and an area of skin over the deltoid region (Fig. 18.3).
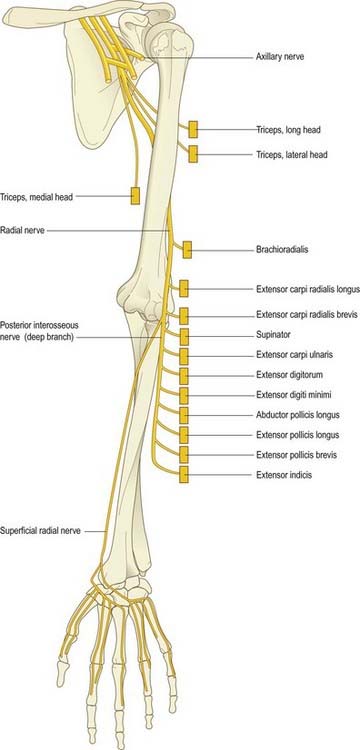
Radial Nerve (C5–8, T1)
The radial nerve is the continuation of the posterior cord of the brachial plexus (Fig. 18.4). In the upper arm it lies in the spiral groove of the humerus, where it is accompanied by the profunda brachii artery and its venae comitantes. It enters the posterior (extensor) compartment and supplies triceps, then reenters the anterior compartment of the arm by piercing the lateral intermuscular septum. At the level of the lateral epicondyle it gives off the posterior interosseous nerve, which passes between the two heads of the supinator and enters the extensor compartment of the forearm. The posterior interosseous nerve supplies these muscles. The radial nerve itself continues into the forearm in the anterior compartment deep to the brachioradialis. It terminates by supplying the skin over the posterior aspect of the thumb, index, middle fingers and radial half of the ring finger.
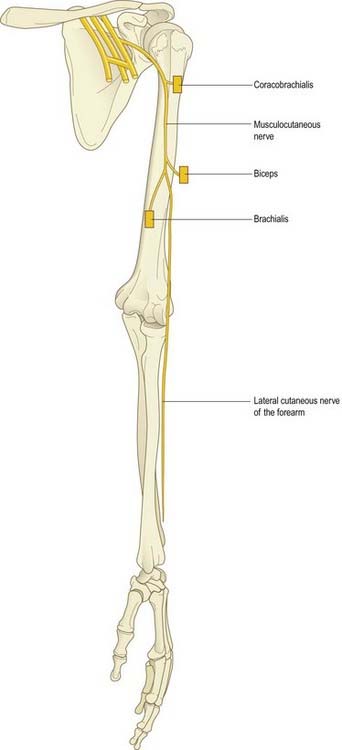
Musculocutaneous Nerve (C5–7)
The musculocutaneous nerve is formed from the continuation of the lateral cord of the brachial plexus. It pierces the coracobrachialis; supplies it, biceps and brachialis; then continues into the forearm as the lateral cutaneous nerve of the forearm (Fig. 18.5).
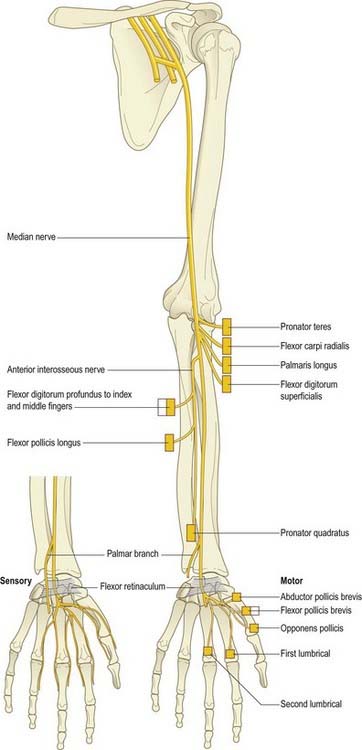
Median Nerve (C6–8, T1)
The median nerve is formed by the union of the terminal branch of the lateral and medial cords of the brachial plexus (Fig. 18.6). It has no branches in the upper arm. It enters the forearm between the two heads of pronator teres and gives off the anterior interosseous nerve, which supplies all the flexor muscles of the forearm except for flexor carpi ulnaris and the ulnar half of flexor digitorum profundus. The median nerve itself passes deep to the flexor retinaculum at the wrist. On entering the palm, it gives off motor branches to the thenar muscles and the radial two lumbricals and cutaneous branches to the palmar aspect of the thumb, index and middle fingers and the radial half of the ring finger.
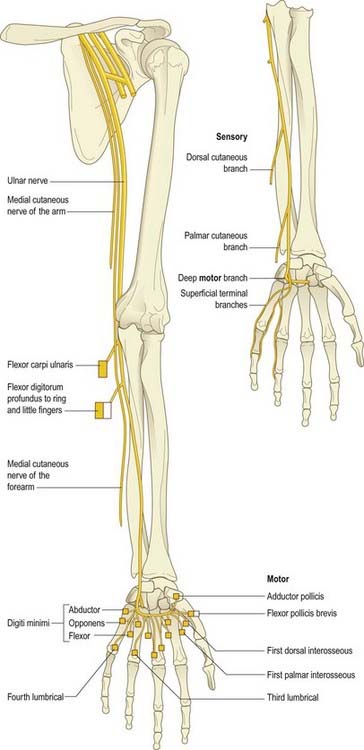
Ulnar Nerve (C7, C8, T1)
The ulnar nerve is the continuation of the medial cord of the brachial plexus (Fig. 18.7). Like the median nerve, it has no branches in the upper arm. It enters the posterior compartment of the upper arm midway down its length by piercing the medial intermuscular septum and passes behind the medial epicondyle of the humerus to enter the forearm. It passes to the wrist deep to flexor carpi ulnaris, giving branches to this muscle and to the ulnar half of flexor digitorum profundus. Just proximal to the wrist it gives off a dorsal cutaneous branch that supplies the skin over the dorsal aspect of the little finger and the ulnar half of the ring finger. The ulnar nerve crosses into the palm superficial to the flexor retinaculum in Guyon’s canal. It divides into a motor branch, which supplies the hypothenar muscles, the intrinsics (apart from the radial two lumbricals) and adductor pollicis, and cutaneous branches, which supply the skin of the palmar aspect of the little finger and ulnar half of the ring finger.
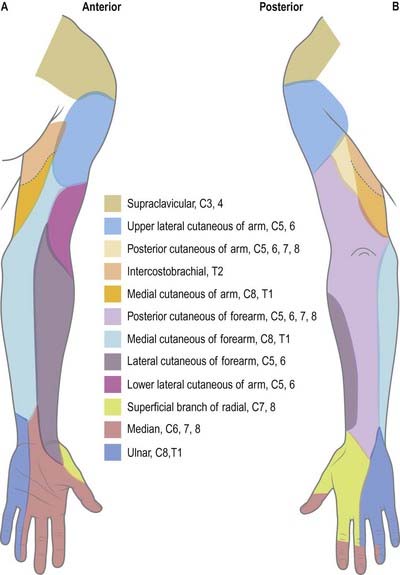
Dermatomes
Our knowledge of the extent of individual dermatomes, especially in the limbs, is based largely on clinical evidence (Fig. 18.8). The dermatomes of the upper limb arise from spinal nerves C5–8 and T1. C7 supplies the central part of the hand. Considerable overlap exists between adjacent dermatomes innervated by nerves derived from consecutive spinal cord segments.
Myotomes
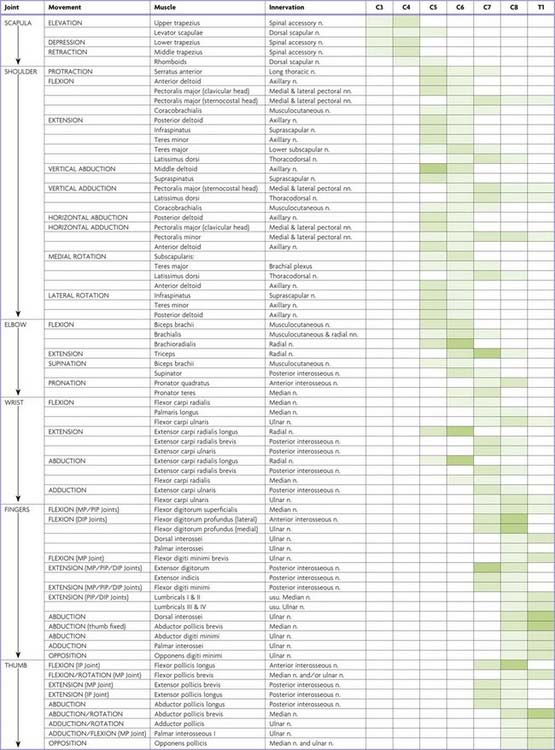
Each spinal nerve originally supplies the musculature derived from its own myotome. Where myotomal derivatives remain entities, they retain their original segmental supply. When derivatives from adjoining myotomes fuse, the resulting muscles do not always retain a nerve supply from each corresponding spinal nerve. Because muscles develop in situ, in the mesodermal cores of the developing limbs, it is impossible to identify their original segments by a developmental study. Most limb muscles are innervated by neurones from more than one segment of the spinal cord. Tables 18.1 to 18.4 summarize the predominant segmental origins of the nerve supply for each of the upper limb muscles and for movements taking place at the joints of the upper limb; damage to these segments or to their motor roots results in maximal paralysis.
Table 18.1 Movements, muscles and segmental innervation in the upper limb
Table 18.2 Segmental innervation of muscles of the upper limb
| C3, C4 | Trapezius, levator scapulae |
| C5 | Rhomboids, deltoids, supraspinatus, infraspinatus, teres minor, biceps |
| C6 | Serratus anterior, latissimus dorsi, subscapularis, teres major, pectoralis major (clavicular head), biceps, coracobrachialis, brachialis, brachioradialis, supinator, extensor carpi radialis longus |
| C7 | Serratus anterior, latissimus dorsi, pectoralis major (sternal head), pectoralis minor, triceps, pronator teres, flexor carpi radialis, flexor digitorum superficialis, extensor carpi radialis longus, extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi |
| C8 | Pectoralis major (sternal head), pectoralis minor, triceps, flexor digitorum superficialis, flexor digitorum profundus, flexor pollicis longus, pronator quadratus, flexor carpi ulnaris, extensor carpi ulnaris, abductor pollicis longus, extensor pollicis longus, extensor pollicis brevis, extensor indicis, abductor pollicis brevis, flexor pollicis brevis, opponens pollicis |
| T1 | Flexor digitorum profundus, intrinsic muscles of the hand (except abductor pollicis brevis, flexor pollicis brevis, opponens pollicis) |
Table 18.3 Segmental innervation of joint movements of the upper limb
| Shoulder | Abductors and lateral rotators | C5 |
| Abductors and medial rotators | C6–8 | |
| Elbow | Flexors | C5, C6 |
| Extensors | C7, C8 | |
| Forearm | Supinators | C6 |
| Pronators | C7, C8 | |
| Wrist | Flexors and extensors | C6, C7 |
| Digits | Long flexors and extensors | C7, C8 |
| Hand | Intrinsic muscles | C8, T1 |
Muscle Innvervation and Function
Table 18.1 provides the following information about the innervation and functions of muscles in the upper limb:
Movements
At the central nervous level of control, muscles are recognized not as individual actuators but as components of movement. Muscles may contribute to several types of movement, acting variously as prime movers, antagonists, fixators or synergists. For example, in the movement of the scapula around the thorax, serratus anterior acts as an antagonist of trapezius, but in the forward rotation of the scapula, the two muscles combine as prime movers. Moreover, a muscle that crosses two joints can produce more than one movement. Even a muscle that acts across one joint can produce a combination of movements, such as flexion with medial rotation or extension with adduction. Some muscles have therefore been included in more than one place in Table 18.1, but even these listings are not exhaustive.
Nerve Roots
The spinal roots listed as contributing to muscle innervation vary in different texts; this is a reflection of the often unreliable nature of available information. The most positive identifications have been obtained by electrically stimulating spinal roots and recording the evoked electromyographic activity in the muscles. This is a laborious process, however, and data of this quality are in limited supply. Much of the information in Table 18.1 is based on neurological experience gained in examining the effects of lesions, and some of it is far from new.
Major and Minor Contributions
Spinal roots have been given the same shading in Table 18.1 when they innervate a muscle to a similar extent or when differences in their contribution have not been described. Heavy shading indicates roots from which there is known to be a dominant contribution. From a clinical viewpoint, some of these roots may be regarded as innervating the muscle almost exclusively: for example, deltoid by C5, brachioradialis by C6, triceps by C7. Minor contributions have been retained in the table to increase its utility in other contexts, such as electromyography and comparative anatomy.
Clinical Testing
For diagnostic purposes, it is neither necessary nor possible to test every muscle, and the experienced neurologist can cover every clinical possibility with a much shorter list. In Table 18.1, red has been used to highlight those muscles or movements that have diagnostic value. The emphasis here is on the differentiation of lesions at different root levels. Other lists could be developed to differentiate between lesions at the level of the root, plexus or peripheral nerve; at different sites along the length of a nerve; or between different peripheral nerves. The preferred criteria for including a given muscle in such a list are that it is visible and palpable, that its action is isolated or can be isolated by the examiner, that it is innervated by one peripheral nerve or (predominantly) one root, that it has a clinically elicitable reflex and that it is useful in differentiating among different nerves, roots or lesion levels.
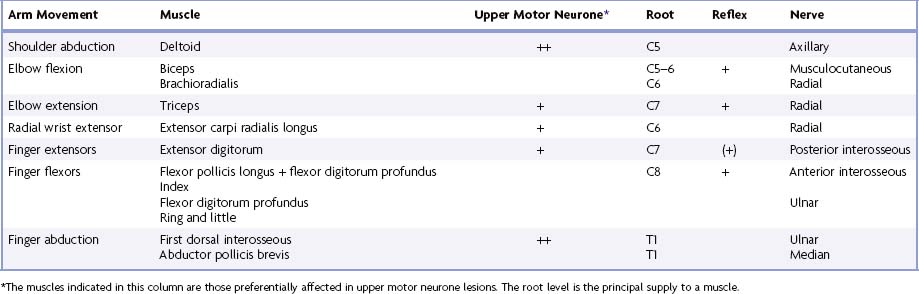
Determination of A Lesion’s Location
Any muscle to be tested must satisfy a number of criteria. It should be visible, so that wasting or fasciculation can be observed and the muscle’s consistency with contraction can be felt. It should have an isolated action, so that its function can be tested separately. The muscle tested should help differentiate between lesions at different levels in the neuraxis and in peripheral nerves, or between peripheral nerves. It should be tested in such a way that normal can be differentiated from abnormal, so that slight weakness can be detected early with reliability. Some preference should be given to muscles with an easily elicited reflex.
Table 18.4 lists movements and muscles chosen according to these criteria. For example, with an upper motor neurone lesion, shoulder abduction, elbow extension, wrist and finger extension and finger abduction are weaker than their opposing movements. Because this weakness may be more distal than proximal, or vice versa, normal shoulder abduction and finger abduction excludes an upper motor neurone weakness of the arm. Some muscles are difficult to test but are included for special reasons. For example, brachioradialis strength is difficult to assess, but the muscle can be seen and felt, it is innervated mostly by the C6 root, and it has an easily elicited reflex.
Brachial Plexus and Nerves of the Shoulder
In the axilla, the lateral and posterior cords of the brachial plexus are lateral to the first part of the axillary artery, and the medial cord is behind it. The cords surround the second part of the artery; their names indicate their relationship. In the lower axillae the cords divide into nerves that supply the upper limb (see Fig. 18.2). Except for the medial root of the median nerve, these nerves are related to the third part of the artery, and their cords are related to the second part; that is, branches of the lateral cord are lateral, branches of the medial cord are medial, and branches of the posterior cord are posterior to the artery.
Branches of the brachial plexus may be described as supraclavicular or infraclavicular.
Supraclavicular Branches
Supraclavicular branches arise from roots or from trunks:
| From roots | 1. Nerves to scaleni and longus colli | C5, C6, C7, C8 |
| 2. Branch to phrenic nerve | C5 | |
| 3. Dorsal scapular nerve | C5 | |
| 4. Long thoracic nerves | C5, C6 (C7) | |
| From trunks | 1. Nerve to subclavius | C5, C6 |
| 2. Suprascapular nerve | C5, C6 |
Long Thoracic Nerve
The long thoracic nerve is usually formed by roots from the fifth to seventh cervical rami, although the last ramus may be absent (Fig. 18.9). The upper two roots pierce scalenus medius obliquely, uniting in or lateral to it. The nerve descends dorsal to the brachial plexus and the first part of the axillary artery and crosses the superior border of serratus anterior to reach its lateral surface. It may be joined by the root from C7, which emerges between scalenus anterior and scalenus medius, and descends on the lateral surface of medius. The nerve continues downward to the lower border of serratus anterior and supplies branches to each of its digitations.
The long thoracic nerve is the most common nerve to be affected by neuralgic amyotrophy. Winging of the scapula may be the only clinical manifestation; it is best demonstrated by asking the patient to push against resistance with the arm extended at the elbow and flexed to 90° at the shoulder (Fig. 18.10; see Case 1).
Suprascapular Nerve
The suprascapular nerve is a large branch of the superior trunk (Fig. 18.11). It runs laterally, deep to trapezius and omohyoid, and enters the supraspinous fossa through the suprascapular notch inferior to the superior transverse scapular ligament. It runs deep to supraspinatus and curves around the lateral border of the spine of the scapula with the suprascapular artery to reach the infraspinous fossa, where it gives two branches to supraspinatus and articular rami to the shoulder and acromioclavicular joints. The suprascapular nerve rarely has a cutaneous branch. When present, it pierces the deltoid close to the tip of the acromion and supplies the skin of the proximal third of the arm within the territory of the axillary nerve.
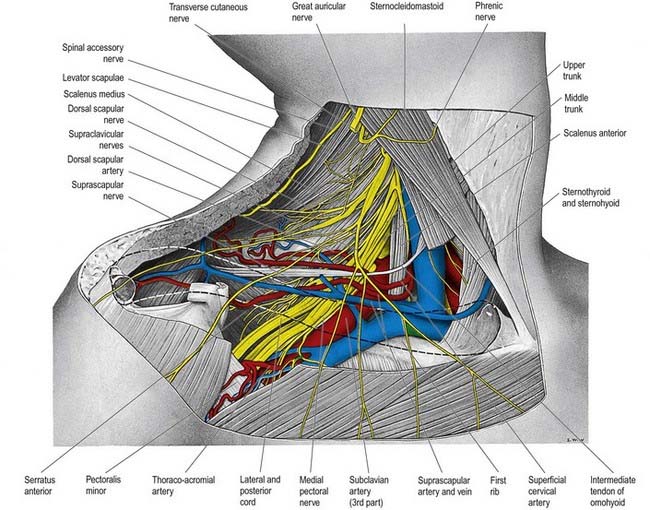
Fig. 18.11 Lower part of the posterior triangle showing the relations of the third part of the right subclavian artery. The clavicle has been removed, but its outline is indicated by a dashed line. In this dissection, the middle trunk of the brachial plexus gives an unusual contribution to the medial cord.
Infraclavicular Branches
| Lateral cord | Lateral pectoral | C5, C6, C7 |
| Musculocutaneous | C5, C6, C7 | |
| Lateral root of median | (C5), C6, C7 | |
| Medial cord | Medial pectoral | C8, T1 |
| Medial cutaneous of forearm | C8, T1 | |
| Medial cutaneous of arm | C8, T1 | |
| Ulnar | (C7), C8, T1 | |
| Medial root of median | C8, T1 | |
| Posterior cord | Upper subscapular | C5, C6 |
| Thoracodorsal | C6, C7, C8 | |
| Lower subscapular | C5, C6 | |
| Axillary | C5, C6 | |
| Radial | C5, C6, C7, C8, (T1) |
Lateral Pectoral Nerve
The lateral pectoral nerve (see Fig. 18.9) is larger than the medial and may arise from the anterior divisions of the upper and middle trunks or by a single root from the lateral cord. Its axons are from the fifth to seventh cervical rami. It crosses anterior to the axillary artery and vein, pierces the clavipectoral fascia and supplies the deep surface of pectoralis major. It sends a branch to the medial pectoral nerve, forming a loop in front of the first part of the axillary artery (see Fig. 18.9), to supply some fibres to pectoralis minor.
Axillary Nerve
The axillary nerve arises from the posterior cord (C5, C6). It is initially lateral to the radial nerve, posterior to the axillary artery and anterior to subscapularis (Fig. 18.12). At the lower border of subscapularis it curves back inferior to the humeroscapular articular capsule and, with the posterior circumflex humeral vessels, traverses a quadrangular space bounded above by subscapularis (anterior) and teres minor (posterior), below by teres major, medially by the long head of triceps and laterally by the surgical neck of the humerus. In the space it divides into anterior and posterior branches. The anterior branch curves around the neck of the humerus with the posterior circumflex humeral vessels, deep to deltoid. It reaches the anterior border of the muscle, supplies it and gives off a few small cutaneous branches that pierce deltoid and ramify in the skin over its lower part. The posterior branch courses medially and posteriorly along the attachment of the lateral head of triceps, inferior to the glenoid rim. It usually lies medial to the anterior branch in the quadrangular space. It gives off the nerve to teres minor and the upper lateral cutaneous nerve of the arm at the lateral edge of the origin of the long head of triceps. The nerve to teres minor enters the muscle on its inferior surface. The posterior branch frequently supplies the posterior aspect of deltoid, usually via a separate branch from the main stem, or occasionally from the superior lateral cutaneous nerve of the arm. However, the posterior part of deltoid has a more consistent supply from the anterior branch of the axillary nerve, which should be remembered when performing a posterior deltoid-splitting approach to the shoulder. The upper lateral cutaneous nerve of the arm pierces the deep fascia at the medial border of the posterior aspect of deltoid and supplies the skin over the lower part of deltoid and upper part of the long head of triceps. The posterior branch is intimately related to the inferior aspects of the glenoid and shoulder joint capsule, which may place it at particular risk during capsular plication or thermal shrinkage procedures (Ball et al 2003). There is often an enlargement or pseudoganglion on the branch to teres minor. The axillary trunk supplies a branch to the shoulder joint below subscapularis.
Musculocutaneous Nerve
The musculocutaneous nerve (see Fig. 18.9) arises from the lateral cord (C5–7), opposite the lower border of pectoralis minor. It pierces coracobrachialis and descends laterally between biceps and brachialis to the lateral side of the arm. Just below the elbow it pierces the deep fascia lateral to the biceps tendon and continues as the lateral cutaneous nerve of the forearm. A line drawn from the lateral side of the third part of the axillary artery across coracobrachialis and biceps to the lateral side of the biceps tendon is a surface projection for the nerve (but this varies according to its point of entry into coracobrachialis). It supplies coracobrachialis, both heads of the biceps and most of brachialis. The branch to coracobrachialis is given off before the musculocutaneous nerve enters the muscle; its fibres are from the seventh cervical ramus and may branch directly from the lateral cord. Branches to biceps and brachialis leave after the musculocutaneous has pierced coracobrachialis; the branch to brachialis also supplies the elbow joint. The musculocutaneous nerve supplies a small branch to the humerus, which enters the shaft with the nutrient artery.
Median Nerve
The median nerve has two roots from the lateral (C5, C6, C7) and medial (C8, T1) cords, which embrace the third part of the axillary artery and unite anterior or lateral to it (see Fig. 18.9). Some fibres from C7 leave the lateral root in the lower part of the axilla and pass distomedially posterior to the medial root, and usually anterior to the axillary artery, to join the ulnar nerve. They may branch from the seventh cervical ventral ramus. Clinically, they are believed to be mainly motor and to supply flexor carpi ulnaris. If the lateral root is small, the musculocutaneous nerve (C5, C6, C7) connects with the median nerve in the arm. It is described in more detail below.
Ulnar Nerve
The ulnar nerve arises from the medial cord (C8, T1) but often receives fibres from the ventral ramus of C7 (see Fig. 18.9). It runs distally through the axilla medial to the axillary artery, between it and the vein. It is described in more detail below.
Radial Nerve
The radial nerve is the largest branch of the brachial plexus. It arises from the posterior cord (C5, C6, C7, C8, [T1]; see Fig. 18.12) and descends behind the third part of the axillary artery and the upper part of the brachial artery, anterior to subscapularis and the tendons of latissimus dorsi and teres major. With the arteria profunda brachii it inclines dorsally and passes through the triangular space below the lower border of teres major, between the long head of triceps and the humerus. It is described in more detail below.